April 20, 2024 ✒ Andrew Kantor
The latest poll about healthcare trust has some bad news for pharmacists: Trust in them (that is, you) dropped 3 percent from 2023 to 2024. That was only half the drop that trust in “friends and family” saw; maybe they got tired of being told, “No, dear, watermelon won’t cure your ingrown toenail no matter what you saw on TikTok.” Trust also dropped in pharma companies, government leaders, and journalists — all likely because people think they can find better information on their own. “The rise of empowerment is potentially something great,” said the CEO of Edelman Trust, which conducted the survey. “But without it being balanced with some form of trust in institutions, trust in expertise — if it’s all self-reliance, it’s like giving a kid the keys to a car and saying, ‘Go drive!’” The problem, of course, is that “empowerment” for many people means “believing whatever nonsense is being spouted on social media,” leading to people thinking mRNA vaccines contain nanobots, or that drinking bleach can treat Covid. Hey, pharmacists and pharmacy techs — want to learn about Abbott’s new FreeStyle Libre 3 continuous glucose monitor? How about if Abbott threw in a free dinner to go along with it? If you’re in the Columbus area this coming Tuesday, April 23, register for the aptly named “An Overview of the FreeStyle Libre 3 system.” The program is at Mabella Italian Steakhouse* at 6:30 p.m. and includes dinner while you listen to Bantwal Baliga, the director at East Alabama Endocrinology. Like we said, the program and food are free — but you do have to register. Click here to do that, then enter meeting ID 11165. * 6835 Midland Commons Blvd in Columbus (map) The good news for Eli Lilly is that Zepbound (tirzepatide) was shown in phase-3 trials to work against obstructive sleep apnea. It makes sense, of course. As GLP-1 drugs help treat obesity, they also help with the side effects, from heart issues to sleep apnea. The important part is getting FDA approval to treat those on-label, which would mean more insurance coverage for the drugs. …is that supply problems continue for Zepbound and other GLP-1 agonists. The drug isn’t expected to be out of shortage until June. The reason is simple: “insatiable demand.” Diabetes, obesity, heart issues, sleep apnea … what else might Mounjaro, Ozempic, and Zepbound be able to treat? How about fatty liver disease, kidney disease, brain disorders, Parkinson’s, Alzheimers, depression, bipolar disorder, anxiety … heck, just throw a dart at an ICD-10 chart. Forbes has the full rundown of what scientists are looking at. After pledging to lower the costs of its Flovent asthma med, GSK went and pulled it from the market, leaving generic fluticasone in its place — without that $35/month guarantee. Oh, well. Worse, the generic version still isn’t covered by many insurers, so American kids can’t get their daily-use inhalers unless their parents shell out the big bucks — or convince the insurers to pay for it. You would think insurance companies would be happy to cover cheaper generics, but you’re forgetting one thing: kickbacks. Insurers and PBMs don’t get kickbacks from drug makers on generic products, only on branded ones, so why bother covering the generics? That wouldn’t be good for shareholders, would it? GSK says its new, first-in-class gonorrhea treatment, gepotidacin, has passed its phase-3 trials with a 90+ percent success rate. That’s good news, what with STDs running rampant these days. Drug shortages here are a problem, but they’re worse overseas — specifically, in Britain, where they’re dealing with not only the general Europe-wide issues, but the continued fallout from Brexit. “Drug shortages in the UK more than doubled between 2020 and 2023 with Brexit likely to ‘significantly weaken’ the country’s ability to tackle supply chain snags.” Women have been dealing with menopause for a couple of hundred thousand years, and yet there’s still a bit of a stigma talking about it, the effects it can have on a woman’s body, and ways to help alleviate some of those negative issues. Worse, as this article in the Atlantic explains, many gynecologists will try to solve everything with estrogen (or, if they’re British, oestrogen). Since the 1960s it’s been the go-to magic bullet for women in and after menopause. Reality, though, is more complex — and we’ve learned a lot since the ’60s. Still, though, the lack of a “frank approach to sexuality” for both people born female and those who have transitioned there has kept many from realizing the benefits of other hormones. (Ironically, trans women often get better care when it comes to hormones.) The point of all this, and of the Atlantic article, is that it’s important for women to think beyond estrogen.Kids can’t get asthma meds, losing trust in pharmacists, looking beyond estrogen post-menopause, and more
Trust issues
CGM info and a free dinner, on Abbott
Ups and downs for Lilly
But the bad news….
On the subject of GLP-1 agonists
Please, sir, can we have our asthma meds?
Short takes
New antibiotic for gonorrhea
Elsewhere: Could Be Worse edition
The Long Read: menopause, estrogen, and women’s unused options
April 18, 2024 ✒ Andrew Kantor
We’ve covered the dangers of melatonin gummies a couple of times, whether it’s parents giving too much to kids, or kids popping them thinking they’re candy. Now, finally, someone has come up with a crazy idea to hopefully reduce some poisonings: labelling the bottles. The Council for Responsible Nutrition — the trade group for supplement manufacturers — has announced that it’s adopted new guidelines such as … All the guidelines are voluntary, and the CRN suggests they be implemented within a year and a half to 2 years. One good thing about US drug makers being so profitable is that those profits trickle down — after all, they’re paying a ton in taxes. Oh, wait. Corporations are supposed to pay a nominal tax rate of 21%. But in recent years, the biggest pharmaceutical companies had an average effective tax rate of less than 12%, according to an analysis by the Senate Finance Committee. The game, it seems, is to create a subsidiary outside US jurisdiction, sell that subsidiary your intellectual property rights, then “pretend like the profit is accrued to these offshore subsidiaries, even though the sales are back to the United States.” And thus, the “financial records for the top five drug companies in the U.S. showed that in 2023, all but Eli Lilly reported losing money in the US.” (Emphasis ours.) That’s right: When it comes to paying their share, the big pharmaceutical companies claim they’re losing money. Deadly bacteria — just like vampires, mosquitoes, and (according to Facebook) some politicians — are apparently drawn to the scent of blood. “We learned some of the bacteria that most commonly cause bloodstream infections actually sense a chemical in human blood and swim toward it.” Washington State University researchers say it’s one reason some conditions, like inflammatory bowel disease, can be deadly: Bacteria head straight for any internal bleeding. Having found the mechanism, they now hope to find a way to block it. This one comes out of the University of California-Riverside and it would be “universal” for a given disease (e.g., flu, Covid) “because it targets a part of the viral genome that is common to all strains of a virus.” So in the case of the flu, no more guessing the next year’s strain, and in the case of Covid-19, no more playing Whac-A-Mole™ with variants. The new strategy does away with Ye Olde strategy of getting the immune system to mount a response. Instead, it relies on the production of “interfering RNA” (RNAi) molecules that the body produces to attack a virus. Normally, a virus can block enough RNAi to thrive, but the UCR-developed vaccine counters this, leaving the virus vulnerable to RNAi attacks. “[The virus] can replicate to some level, but then loses the battle to the host RNAi response.” [T]he researchers say there is little chance of a virus mutating to avoid this vaccination strategy. “Viruses may mutate in regions not targeted by traditional vaccines. However, we are targeting their whole genome with thousands of small RNAs. They cannot escape this.” Pharmacists at two Rhode Island CVS locations … … are seeking to join the Pharmacy Guild, a U.S. trade union exclusively specializing in representing and unionizing pharmacy professionals, to fight for higher staffing levels, which they argue will lead to optimal patient safety and care outcomes. To fight postpartum depression, a quick dose of esketamine might be the ticket. Chinese researchers found that, at least for mothers with prenatal depression… …a single low dose of esketamine after childbirth decreases major depressive episodes at 42 days post partum by about three quarters. To get a jump on the next pandemic, the US will be partnering with 50 nations around the globe (or across the globe for you flat-Earthers). The idea is that we’ll help them “prevent, detect, and effectively respond to biological threats.” That way if something appears first in, say, East Freedonia, the Freedonians can slow its progress enough for America to be better prepared. The WHO has been trying to get an international pandemic plan in place, but that hasn’t happened. So here we are. (This isn’t just a “Hey, we’re gonna do this” announcement. It’s actually a huge program that’s well underway. Check out the State Department details. The Chinese government, it seems, is giving tax rebates to “companies that manufacture fentanyl analogues, precursors and other synthetic narcotics, so long as they sell them outside of China,” according to a report from the bipartisan House of Representatives’ select committee on China. For its part, Chinese officials pinkie-promised that they’re cooperating with US drug authorities to try to limit fentanyl production. They also said that the problem is US demand, not Chinese supply. Quoth: “It is very clear that there is no fentanyl problem in China, and the fentanyl crisis in the United States is not caused by the Chinese side, and blindly blaming China cannot solve the U.S.’s own problem.”Pharma companies losing money? Plus blood-hunting germs, warnings on melatonin, and more
The least they could do
The word is chutzpah

Out for blood
The next universal vaccine candidate
Short Takes
Elsewhere: CVS pharmacies look to unionize
Ketamine after birth
Preparing for the next one
With friends like these
April 16, 2024 ✒ Andrew Kantor
If a patient has a bacterial infection in the lower lungs, antibiotics would seem to be a good choice to treat it. Wrong. Researchers from Georgetown, the University of Wisconsin, and UGA found that that giving antibiotics to treat a cough — even when it’s caused by a bacterial infection — usually doesn’t work. The antibiotics prescribed in this study for lower-tract infections were all appropriate, commonly used antibiotics to treat bacterial infections. But the researchers’ analysis showed that of the 29% of people given an antibiotic during their initial medical visit, there was no effect on the duration or overall severity of cough compared to those who didn’t receive an antibiotic. Combined with simply not knowing whether a cough is bacterial or viral (and of course the whole overuse-of-antibiotics concern) it’s probably best to use “Basic symptom-relieving medications plus time.” Drugs in shortage have hit their highest level since 2001, according to data from the American Society of Health-System Pharmacists — that’s as far back as it tracked those numbers. Most medicines in active shortage at the end of March were central nervous system drugs, with 66 on the list, followed by antimicrobials at 43. Rounding out the top five are hormonal agents (34), chemotherapy (32) and fluids and electrolytes (25). Until the president is willing to press the big red “Lower Drug Prices” button on his desk*, there’s a lot of blame and speculation going around — it’s almost as if there are several issues at work. The DEA’s opioid reaction of tightening restrictions are a part. Wholesalers are a part. Drug companies are a part. You get the picture. Here’s an interesting tidbit: “[A] vast majority (60%) of manufacturers told the University of Utah Drug Information Service that they do not know or refused to provide a potential reason for the shortages.” The 40ish percent who did reply assigned blame equally to supply/demand, manufacturing issues, or “business decision.” * It’s right next to the “Lower Gas Prices” button. One of the issues with drug shortages is the competing priorities: Independence from Chinese manufacturers and an uninterrupted supply of critical meds. For example, one of the Chinese companies that Congress is investigating for its ties to the Chinese government also happens to make “blockbuster drugs for the American market that have been hailed as advances in the treatment of cancers, obesity and debilitating illnesses like cystic fibrosis.” No simple answers, huh? A new study out of Iran found that a combination of probiotics and vitamin D “significantly improves cognitive function in schizophrenic patients.” It was a small study (69 patients) based on the idea that both “good” gut bacteria and vitamin D can regulate the kind of inflammation that might be associated with schizophrenia. We say “might” because the causes of schizophrenia still aren’t clear. (“It has been suggested that anti-inflammatory strategies can be effective in the treatment of schizophrenia.”) They also suggested that “In the pathogenesis of schizophrenia, vitamin D deficiency is an important factor.” This is one of those studies that gets put in the ever-growing pile of “Data that might lead to a path that leads to a treatment.” We might be on the cusp of a ia vaccine. It’s still in the early-trial stage, but UK infectious-disease researchers — with help from some of those shifty Danes — have developed “CTH522,” which uses and outer membrane molecule of the Chlamydia trachomatis bacteria to create an immune response. Chlamydia, as you probably know, is the most common STD in the country and is easily treatable … if it’s found. It usually doesn’t present symptoms in women, but it can cause a lot of issues including vision loss and the inability to get pregnant. And with STD rates skyrocketing in these parts, a vaccine would be a Very Big Deal. Still, the vaccine candidate is very much in the early stages, but the fact that it exists at all is good news. In addition to all its other issues, the flu causes collateral damage to lung tissue — potentially life-threatening damage. Now, though, scientists at four major research institutions* have developed a drug that not only protects against that lung damage, but also “seemed to improve the adaptive response against the virus.” Well, in mice at least. Still, the drug “UH15-38,” removes one of the deadliest aspects of the flu for those mice: the inflammation that permanently damages the lungs. Some inflammation is good, as it means the immune system is in gear. But too much, obviously, can be a big problem. Here comes the science: The collaborating scientists achieved a Goldilocks amount of inflammation using clever chemistry. Their new drug inhibited one part of a major inflammation protein in immune cells: Receptor-Interacting Protein Kinase 3 (RIPK3). RIPK3 controls two cell death pathways in response to infection: apoptosis and necroptosis. Necroptosis is highly inflammatory, but apoptosis is not. Both pathways are used in the antiviral response. UH15-38 was designed to prevent RIPK3 from starting necroptosis while maintaining its pro-apoptotic properties. Even better, unlike current flu treatments (i.e., Tamiflu), UH15-38 works even if taken 5 days after initial infection. * Fox Chase Cancer Center, St. Jude Children’s Research Hospital, Tufts University School of Medicine, and the University of Houston If your garage is filled with a variety of chemicals — old paint, car fluids, that rusted can of something of Uncle Sonny’s — you might be increasing your risk of amyotrophic lateral sclerosis, aka ALS*. University of Michigan researchers knew that exposure to heavy-duty toxins at work was dangerous, but when they looked at home storage (i.e., in the garage), they found that even casual woodworkers and gardeners were at risk. Through statistical analysis, they found that the storage of chemicals — including gasoline and gasoline powered equipment, lawn care products, pesticides, paint and woodworking supplies — were significantly associated with ALS risk. The good news is that this only applies to attached garages. Detached ones are only risk if you spend too much time there. * Once called “Lou Gehrig’s Disease” until we learned that it isn’t what he actually had.Drug-shortage record, potential chlamydia vaccine, death in the garage, and more
When antibiotics fail (even though you’d think they would work)
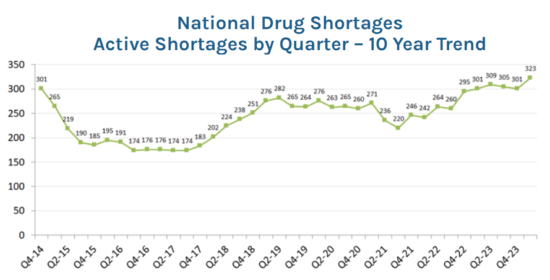
Drug shortages set new record
In a related story….
Supplements for schizophrenia?
Let’s applaud these scientists
Stopping flu’s deadly side
Bad chemical romance
April 13, 2024 ✒ Andrew Kantor
No one likes a bitter drug — coffee being the exception — and usually the solution is “Buck up, little soldier.” But there might be a solution, according to the folks at the Monell Chemical Senses Center (“Advancing discovery in taste and smell”): rosiglitazone, the diabetes drug. Apparently it can be added to other medications to make them taste better. It’s not perfect, but they see it as a good first step towards building a better bitter blocker. For now, though, “Rosiglitazone is valuable as a bitter blocker because it is potentially effective in most people and is part of a class of drugs already approved worldwide for treating diabetes.” Eli Lilly and Novo Nordisk have been fighting tooth and nail to prevent pharmacists from creating compounded versions of their GLP-1 drugs while those drugs are in shortage. Lilly just lost again in Florida where a judge tossed the company’s suit saying that it can’t “use state law as a back door to privately enforce” federal law — specifically the Food, Drug, and Cosmetic Act. The FDA is pretty clear: If a drug is in shortage, compounding it is AOK. (We’ll point out that the argument “XYZ Pharmacy is claiming to sell Ozempic™” is a legit trademark issue, but that’s different than “XYZ can’t sell compounded semaglutide.”) Just because you’ve hit 65, ladies, doesn’t mean you have to give up on hormone therapy. That’s according to the North American Menopause Society* — a new paper it published says, essentially, that fears of cancer and heart disease are unfounded … sort of. Rather, the risk is nuanced: A new large-scale study based on the records of 10 million senior Medicare women from 2007 to 2020, however, suggests that the implications of HT [hormone therapy] use beyond age 65 years vary by type, route, and dose. In other words, ‘there is no general rule for stopping hormone therapy in a woman based on age alone.’ * It now identifies simply as “The Menopause Society” Georgia got its third measles case this year according to the Department of Public Health. And no, this person wasn’t vaccinated. (He or she came here with an international group of students and is now in hospital recovering.) Three is a nice low number, but given how contagious measles is, fingers crossed that it stays low thanks to most people being vaccinated. On that subject … With 113 cases in the US so far this year, the country is poised to lose the measles-elimination status that it achieved almost 20 years ago. What does that mean? Essentially that measles cases have reached the tipping point where the disease is spreading faster than it can be contained and outbreaks continue. (“[T]here won’t be any economic, political, or practical penalties.”) While anti-vaxxers might celebrate, keep in mind that 68% of kids who contracted measles in the last couple of years required hospitalization, as well as 56% of people overall. The effects of marijuana continue to come fast and furious now that researchers can actually research it. The latest is on the plus side: Non-medical cannabis use is linked to “a lower likelihood of experiencing subjective cognitive decline.” Subjective cognitive decline is all about how participants answered the question, “During the past 12 months, have you experienced confusion or memory loss that is happening more often or is getting worse?” Individuals who used cannabis for non-medical reasons reported significantly reduced odds of experiencing subjective cognitive decline compared to those who did not use cannabis. This suggests that non-medical cannabis use, as opposed to medical or mixed-use, might have a protective association against the self-perception of cognitive decline. What was interesting to the SUNY Upstate Medical University researchers was that why people used cannabis (i.e., recreationally vs. medically) was more important than how much or what type they used. Regardless, if it turns out to be true, Shaggy and Scooby will probably be doing pretty well in their old age. This year New York implemented a new pricing-transparency law that showed just how much money PBMs got from transactions with independent pharmacies. And when they saw how much money they were losing, “Nearly all independent pharmacies surveyed across New York have stopped selling certain name-brand medications.” [P]roviders are more aware that they can lose more than $200 each time they dispense certain prescriptions. […] The most common medications they’ve stopped selling to avoid such losses include weight loss drugs Ozempic and Wegovy, Merck’s diabetes medication Januvia, and Bristol Myers Squibb’s blood thinner Eliquis. Respondents also said they’ve ceased selling Symbicort, which treats asthma, and Biktarvy, an antiretroviral medication to treat HIV and AIDS. As a spokesman for the New York City Pharmacists Society explained, “It is not sustainable economically for them to carry these drugs.” Yes, owning a cat can increase your risk of schizophrenia. A new Aussie meta analysis of 17 studies found that “cat exposure is associated with an increased risk of broadly defined schizophrenia-related disorders” but not, however, for “psychotic-like experiences.” The big caveat is that almost all of those studies show correlation rather than causation, so it might be that whatever causes someone to want a cat also causes them to develop schizophrenia*. (Above link goes to the paper. For the news story click here.) * Yes, there are jokes to be made here, but they would be in bad taste so we’ll let you make them behind closed doors. A couple of cats in Kansas caught a rare fungal infection called sporotrichosis. Normally that’s not news, but the Kansas Department of Health and Environment (and later the CDC) got involved when one of the cats scratched a vet tech and gave the infection to her. They didn’t diagnose the fungal infection quickly enough, so results could have been better. The vet tech was put on an antifungal for eight months, and her infection cleared. The first cat also got an antifungal, but she eventually got sicker, and her owners had her euthanized. The second cat was treated much more quickly and recovered. When pot is good for your brain, plus NY’s painful PBM fallout, Lilly’s latest loss, and more
Bitter battle won?
Lilly loses another case
Hormones after 65? You bet
Short takes
Georgia gets another measles case
19 years down the drain?
Marijuana vs dementia
Elsewhere: “I shouldn’t have looked”
Cat news
One flew over the catbox
Fungus among them (and us)
April 11, 2024 ✒ Andrew Kantor
Oral meds for treating a urinary tract infection aren’t anything new, but what about a vaccine? And what about one that’s a mouth spray? That’s just what British clinicians say they have in a drug called MV140. It’s given twice a day for three months — don’t worry, it’s pineapple-flavored — after which “54 percent of study participants remained UTI-free for nine years after the vaccine, with no notable side effects reported.” They had already shown it worked in the short term, and now they have the long-term safety data. Next they want to expand the test group before talking about bringing it to market. Why yes, they do call it a “game-changer.” Apparently you can treat abnormal heart rhythm at home. All that’s needed is etripamil, a nasal spray calcium-channel blocker, according to researchers at Weill Cornell Medicine. Paroxysmal supraventricular tachycardia (PSVT) isn’t usually deadly, but with shortness of breath, chest pain, dizziness, or fainting involved, it can send people to the ER and even end with short-term hospitalization. But with etripamil on hand it’s like having an asthma inhaler — patients “experienced symptom relief on average in 17 minutes.” This was the second, larger trial of the drug (more than 1,100 patients), designed to show that “etripamil is safe and effective under more real-world circumstances.” Which it did. A new drug called zilebesiran, — an investigational drug, we should point out — does well by people who can’t keep their blood pressure under control. A single injection “reduced systolic blood pressure by between 4 to 12 mmHg on average” for at least 3 months and usually twice that. The basic science: Zilebesiran works by reducing the body’s production of angiotensinogen, a hormone primarily made in the liver that helps to regulate blood pressure by constricting blood vessels. Reducing blood-vessel constriction allows blood pressure to fall. It can be used alone, but it works even better in combo with other anti-hypertensives. Big ol’ caveat: Although the study was done out of Brigham and Women’s Hospital in Boston, it was funded by Alnylam Pharmaceuticals, the manufacturer of zilebesiran. Take from that what you will. The Dawgs moved up nine spots in the US News & World Report rankings of US pharmacy schools, now coming in at #15 out of 141. High-five! Pfizer says its Abrysvo RSV vaccine works a treat for folks under 60. It’s going to ask for approval for the vaccine at least for high-risk people in the 18-59 category. Ka-ching! Acetaminophen during pregnancy doesn’t increase the risk of having a kid with autism, ADHD, or an intellectual disability — so says a big US/Swedish study using data from 2.4 million Swedish kids, including 186,000 whose mothers used acetaminophen during pregnancy, even if they called it “paracetamol.” Imagine what went down at Nature Made HQ: Marketing director: I’m going on vacation for two weeks. Don’t do anything stupid while I’m away. Jimmy from marketing: Sure thing, boss. So, everyone, what sports seasons are starting soon? Kevin from marketing: Baseb— Susan from marketing: April is National Pickleball Month! Jimmy: Great! How can we celebrate it? Susan: Pickled-flavored vitamin gummies! Kevin (quietly): I was gonna suggest Cracker Jack-flavored. Jimmy and Susan: Shut up, Kevin. Researchers at the University of Rochester tested a crazy They tested the ventilation in 100 rooms of various sizes on a campus for special needs kids by measuring carbon dioxide levels. Surprise, surprise! Kids who spent more time in rooms with “suboptimal ventilation” were more likely to get Covid. They also found that spending time in the rooms with newer ventilation systems (MERV-13, if you’re keeping score) reduced the incidence of Covid thanks to better filtering. Meanwhile downstate at Columbia, researchers tested ceiling-mounted far-UV lights as germ killers. “Far-UV” doesn’t hurt people (it can’t damage living skin) but it’s brutal for bacteria. They mounted the devices in a room with lab mice, where cage-cleaning releases a ton of norovirus particles, then tested the air. “Based on our initial sensitivity tests, we expected to see a reduction in airborne virus of around 66%,” said the senior author. Instead, “The result—a reduction in infectious airborne viruses of 99.8%—surpassed expectations and was far greater than what could be achieved by typical air filtration and ventilation.” Now they’re testing the lights in more locations, with the goal of being able to use the devices to keep public spaces disease-free. A nasal spray for the heart, 6-month BP drug, Nature Made’s weird decision, and more
Surprise delivery 1: Oral spray for UTIs
Surprise delivery 2: Nasal spray for tachycardia
Blood pressure: One shot for 6 months
Short takes
Congrats to UGA CoP
RSV vax for everyone?
No Tylenol/autism connection
Why not to drink at work

It’s almost as if Covid is an airborne virus
theory hypothesis: Could improving air quality and circulation cut Covid infections?Safer UV kills airborne germs

April 09, 2024 ✒ Andrew Kantor
Mess with a child’s gut bacteria in the first year and you could raise the risk that he or she develops autism or ADHD. That’s what Swedish and American researchers found after looking at the health records of 16,000 Swedish children born between 1997 and 1999 — kids the Swedes have studied over the past 25 years. “We can see in the study that there are clear differences in the intestinal flora already during the first year of life between those who develop autism or ADHD and those who don’t.” What’s going on? They think something is affecting those bacteria — e.g., antibiotic treatment. For example, “Children who had repeated ear infections during their first year of life had an increased risk of being diagnosed with a developmental neurological disorder later in life.” In fact, they’ve narrowed it down to two particular bacteria that affect risk — “the presence of Citrobacter bacteria or the absence of Coprococcus bacteria increased the risk of future diagnosis.” That info might lead to a concurrent treatment (some kind of probiotic?) to go with antibiotics. As usual, though, more research is needed. What if asthma wasn’t caused by inflammation, rather the inflammation was a result of the disease? That, say British cell biologists, is exactly the case. It’s the mechanical constriction of the airways that leads to an asthma “attack,” including inflammation. Current treatments focus on that inflammation, but that only alleviates symptoms. The issue may lie in the death of the airway’s epithelial cells: When the airway contracts, a process called cell extrusion kills the epithelial cells lining it. So many epithelial cells dying leads to inflammation and excess mucus — an asthma attack. Thus blocking cell extrusion might be a way to prevent attacks rather than dealing with symptoms. And guess what? There’s already a chemical that does that. “[A]n inhaler such as Albuterol opens the airways, which is critical to breathing but, dishearteningly, we found it does not prevent the damage and the symptoms that follow an attack. Fortunately, we found that we can use an inexpensive compound, gadolinium, which is frequently used for MRI imaging, to stop the airway damage in mice models as well as the ensuing inflammation and mucus secretion.” Don’t forget: Early-bird registration for the Georgia Pharmacy Convention ends this Thursday, April 11. Save $50 by registering by then! People who get coronary stents often continue taking aspirin after the procedure. They shouldn’t. A new study out of Mount Sinai found that the standard-of-care guidelines are probably wrong. The best thing patients can do (that we know of) is to use ticagrelor alone. “Our study has demonstrated that withdrawing aspirin in patients with recent ACS [acute coronary artery syndromes] one month after PCI [percutaneous coronary intervention] is beneficial by reducing major and minor bleeding through one year by more than 50 percent. Moreover, there was no increase in adverse ischemic events, meaning continuing aspirin was causing harm without providing any benefit.” What do you someone who tests their partner for STIs by sending a picture of his nether regions to an app? A patient. Yep, there’s an app called Calmara.ai claiming to detect sexually transmitted infections from a photo of a gentleman’s privates. In seconds, the site scans the image and returns one of two messages: “Clear! No visible signs of STIs spotted for now” or “Hold!!! We spotted something sus.” Pro tip: It doesn’t work — “Doctors say it’s a disaster”. What are Many users [on TikTok] also snack on sticks of butter as a weight loss tactic, with some using butter as a meal replacement. Add “skin issues” to the list of side effects of taking semaglutide. Specifically, a study out of Brown “found a higher incidence of ‘altered skin sensations’” among patients taking it, including dyses-, hyperes-, or paresthesia (i.e., various unpleasant or abnormal touch sensations) as well as alopecia or other “adverse dermatologic events.” Scripps Research chemical biologists have developed a vaccine against xylazine, the latest ultra-potent chemical that’s being added to street drugs (and adding to the overdose crisis). It works by training the immune system to attack the fentanyl so it doesn’t add its effect to whatever it’s mixed with. That’s important because naloxone doesn’t work against xylazine, so it’s critical to take it out of the equation. Granted this is still just proof-of-concept, but assuming the technique proves out, it could also be used to create a vaccine against fentanyl — another drug that’s naloxone-proof. Wondering how your pay stacks up against your peers in other states? The good folks at Becker’s have you covered. (Spoiler: There isn’t that much difference state to state, except maybe between the highest paying (California) and the lowest paying (Rhode Island). )A different take on asthma, how antibiotics can lead to autism, skin “issues” from semaglutide, and more
Autism from antibiotics?
Fighting asthma’s cause
Two more days!
Heart surgery? Skip the aspirin
From the Stupidity Files
Say “Cheese”
“Stupid don’t get tired.” —Alonzo Bodden
infomercials influencers peddling for health now? (spins Wheel of Idiocy) Butter. Eating sticks of butter. Why? “Proponents claim it aids weight loss by contributing to feelings of fullness and has other wellbeing benefits like improved mood and energy.”More semaglutide effects
Xylazine vaccine
Short take: Pharmacist pay by state
April 06, 2024 ✒ Andrew Kantor
When you think of the risks of acetaminophen, you usually think of liver damage. But a new study out of UC Davis found that regular use at moderate doses (500 mg per day) “causes numerous signaling pathways inside the heart to be altered.” The results suggest that long-term medium- to high-dose acetaminophen use could cause heart issues as a result of oxidative stress or the buildup of toxins that are produced as acetaminophen breaks down. […] While our bodies can usually clear such toxins before they cause damage, it may be harder for the body to keep up when medium- to high- doses are taken consistently over time. They point out that the study was done in mice, but the lead author still said, “These results prompt me to consider using acetaminophen at the lowest effective dose and for the shortest duration possible.” They could be used to treat Parkinson’s. In one of the first hints of success against the disease, French researchers found that lixisenatide — a GLP-1 receptor agonist — helped reduce some symptoms in a trial of 156 people with Parkinson’s that lasted about a year. During that time, Parkinson’s symptoms like tremor, stiffness, slowness and balance worsened in those taking the placebo but not in those taking the drug. It’s not entirely a surprise, as it’s been known that there’s some connection between diabetes and Parkinson’s. They’re hoping to do a larger study, but Sanofi is pulling lixisenatide from the market because it’s not selling very well. UGA engineers have developed a better, stronger, faster test for Covid-19. Unfortunately it requires specialized equipment and is only useful (at this point) for large-scale population testing. Still, it’s faster than the gold standard PCR tests and just as accurate — even better, it gives a reading of a patient’s viral load rather than just a positive/negative reading. It can also be updated easily to test for new variants. Eventually they hope to be able to cut the price of the equipment to read results so individuals could afford the devices, and those devices could share results with a central database. Because people will be happy to do that. The Brits are turning to AI to cut prescription errors. Oxford University wonks have created “DrugGPT,” which, rather than being trained on the sum total of human knowledge, is specifically fed information about drugs and medical conditions. It’s meant to be an assistant to clinicians — a kind of double-check before sending patients home. Doctors and other healthcare professionals who prescribe medicines will be able to get an instant second opinion by entering a patient’s conditions into the chatbot. Prototype versions respond with a list of recommended drugs and flag up possible adverse effects and drug-drug interactions. Not only does this double-check the docs, it also gives an explanation for its choices, and that explanation (written by a friendly robot) can help with adherence. CVS Health will cover Opill — the OTC birth control pill — at no cost to most patients on its health plans A study by Pfizer (!) found that Paxlovid doesn’t do much to help people who have been fully vaccinated against Covid. The FDA has approved Zevtera (ceftobiprole medocaril sodium for injection) for treating staph infections, acute bacterial skin and skin structure infections, and kids with community-acquired bacterial pneumonia. Zantac came, Zantac caused cancer, Zantac left* — and thousands of lawsuits followed. Now drugmaker Sanofi said it’s settled 4,000 of those suits. Actually, it could be as many as 5,000 because the settlement covers 49 states. Only Delaware suits weren’t settled … but there are something like 20,000 of them. Sanofi won’t say how much it’s paying out, but the company did focus on the important part: It shouldn’t affect the stock price. * Zantac returned, reformulated A preliminary study has found that using e-cigarettes can increase a person’s risk of heart failure by 19%. (That’s based on health data from almost 176,000 Americans, 29,000 of whom said they used vapes.) Worse, if they also use other nicotine products that risk jumps to 59%. The caveat is that the study was observational and doesn’t explain the relationship — it’s correlation, but not necessarily causation. You know the mantra: More research is needed. Side note: E-cigs are so risky it’s ethically impossible to do human studies on them beyond this kind of statistical analysis. That says something. “Skin Wetting Helps Cool Older Adults in Very Hot, Dry Weather” CVS covers The Pill, cooling down old folks, surprise Tylenol danger, and more
Heart damage from Tylenol?
GLP-1 drugs’ next trick
UGA’s better(ish) Covid test
Robot double-checks
Short takes
CVS covers The Pill
Paxlovid limitations
A new antibiotic
Zantac: Some suits settled
E-cigs increase heart risk
Captain Obvious gets his squirt bottle ready
April 04, 2024 ✒ Andrew Kantor
After freaking out over the very idea that their biggest customer wanted to negotiate prices like some kind of dirty capitalist, drug companies reluctantly entered negotiations with HHS over a whopping 10 high-priced drugs. The government made offers, the pharma companies submitted counteroffers, and now the feds have responded — and the pharma companies are saying, ‘Heck, it wasn’t as bad as we expected.’ Next: “Medicare and each drugmaker can meet for haggling sessions as many as three times in the next several months.” Early-bird registration for the Georgia Pharmacy Convention — save $TK! — has been extended until this Monday, April 10. You have one week to register and get the best rate! Of course, if you want to spend a little more, please wait until the 11th, but that’s kind of silly, innit? Not only did bird flu make the jump to dairy cows, then it jumped from a cow to a human in Texas. His primary symptom was conjunctivitis, but he’s still being isolated while being treated with Tamiflu while awaiting the mockery that will surely come his way. “So far, there are no signs that the virus has evolved in ways that would help it spread more easily among people, federal officials have said.” Hmm. The other day Medicare gave permission for part D plans to start covering Wegovy for heart issues (but not weight loss). Now the first private plans — from CVS Health, Elevance (CarelonRx), and Kaiser Permanente — have said they’ll start paying for them. Again, this is only for “reducing the risk of heart attacks and strokes in people who have cardiovascular disease [and] meet body-weight criteria.” And it’s only Wegovy that’s covered because it’s got a study showing it reduces cardiovascular risk — although with this treasure box opened you can expect the other GLP-1 drugs to have similar studies soon. Another win for anti-vaxxers as measles cases in the US jumped by 51 percent in just one week. The really scary part is that more than half of cases (56 percent) “have required hospitalization for isolation or management of virus complications.” And for kids it’s higher: 68 percent. So no, it’s not just a matter of being a bit sick for a few days. The good news is that the number of cases is still low — about 100 cases nationwide across 17 states. The latest version of ChatGPT “Outperformed Physicians in Clinical Reasoning in Head-To-Head Study.” That means it did more than just look up a list of symptoms and make a guess; it was given the patients’ complaints, vital signs and other basic patient info, and the results of diagnostic tests. Then it gave its differential diagnoses, which were compared to those of 21 attending physicians and 18 residents using a test of clinical reasoning called r-IDEA. [T]he chatbot earned the highest r-IDEA scores, with a median score of 10 out of 10 for the LLM [large language model], 9 for attending physicians and 8 for residents. It was more of a draw between the humans and the bot when it came to diagnostic accuracy—how high up the correct diagnosis was on the list of diagnosis they provided—and correct clinical reasoning. ChatGPT was, however “just plain wrong” more often when it came to actually providing reasoning for its answers. (I.e., it got the answers correct as often as humans, but didn’t get there the right way. Take from that what you will.) Canada, like most of the world, has universal healthcare for its citizens — but that hasn’t included pharmaceutical coverage. That, though, is changing as the country prepares to roll out prescription benefits nationwide. And one of the first parts of that rollout is free contraception for women. The government will pay for the most widely used methods to avoid pregnancy, such as IUDs, contraceptive pills, hormonal implants or the day after pill, for the nine million Canadian women of reproductive age. (Also part of this initial rollout is complete coverage of diabetes medication. That’s not as big a deal because insulin is, like, two bucks a month up there anyway.) With all the fuss about weight loss, you know who’s hurting? Companies like General Mills, maker of Cocoa Puffs and Lucky Charms. So what are they doing about it? Jumping on the “anti-diet” movement to convince people that being overweight is just fine*. General Mills has toured the country touting anti-diet research it claims proves the harms of “food shaming.” It has showered giveaways on registered dietitians who promote its cereals online with the hashtag #DerailTheShame, and sponsored influencers who promote its sugary snacks. * No, we’re not implying that there’s anything wrong with not being a Barbie doll, weight-wise. But from a health perspective there are some serious issues when someone feels it’s okay to dive into the Twinkie box mouth wide open.Pushing Lucky Charms, Part D starts covering Wegovy, ChatGPT beats diagnostic docs, and more
The dance continues
More early birds welcome!
ICYMI
Wegovy gets first Part D coverage
Measles continues to spread
Well this is slightly embarrassing
Elsewhere: Maple Syrup edition
The Long Read: Go Big or Go Home edition
April 02, 2024 ✒ Andrew Kantor
The latest needle-free insulin delivery system comes from those thrifty Dutch. (And yes, they call it a “game changer.”) Unlike microneedle patches and such that other universities are developing, the one the Dutchies have developed — they call it “BuBble Gun” — uses high pressure to force the drugs through the skin. Apparently this doesn’t hurt, despite the description: With BuBble Gun, a laser beam is directed at the fluid medicine in a glass cartridge, heating it until it boils and creates a bubble. This bubble grows until it squeezes the liquid at high velocity—30 to 100 meters a second—out of its tube and, in the case of a medicine, into the skin. Rather than piercing the skin, the way a needle would, the drug is pushed between skin cells. Their biggest hurdle right now is adjusting the pressure to account for different skin thicknesses. Here’s an eyebrow raiser: Up to 30% of cardiovascular-related deaths may be attributed to salt intake. Based on a cohort study of 64,000 patients over 7 years, Vanderbilt University researchers found that not only does excess sodium increase the risk of death from by 7 to 13 percent, it seems that just a 1,000 mg increase in salt intake was responsible for … Maybe a bit of salt substitute (or simply potassium chloride) is in order. STIs for people over 55 are on the rise, big time. Rates of chlamydia, gonorrhea, and syphilis in people ages 55 and up more than doubled in the U.S. over the 10-year period from 2012 to 2022, according to data from the Centers for Disease Control and Prevention. “The trend is prompting doctors to call for more discussions with older people about sexual health.” We’ll leave those discussions to you. Cases of tuberculosis in the US shot up by 16% from 2022 to 2023 to hit the highest level in more than a decade, probably due to more cases worldwide, as well as a post-pandemic jump. (The good news is that we still have one of the lowest rates in the world.) No one is entirely sure what causes chronic fatigue syndrome, but at least one mystery about it has been cleared up: It’s “unambiguously biological,” not, as some clinicians said, a psychological condition. “It’s a systemic disease,” wrote the authors (“75 multidisciplinary scientists and clinicians”), “and the people living with it deserve to have their experiences taken seriously.” They compared healthy people to those who reported chronic fatigue syndrome and found those with CFS had testable biological differences in the immune system and the fecal microbiome, as well as “Reduced neurotransmitter metabolism” and “Autonomic nervous system dysfunction,” among several other markers. What’s still unclear is how CFS develops, and whether there will be simple biomarker they can find (rather than a list of checkboxes). An oncologist’s reminder: Cannabis is not a cure for cancer. Never has been. It might help alleviate some symptoms, but the potential side effects — an wide variation in strengths and types — mean patients need to tread (or, rather, toke) carefully. Covid, flu, and RSV are all on the decline (although flu numbers are still above normal). The next drug in shortage is Eli Lilly’s Zepbound, the hottest of the GLP-1 weight loss drugs. It’s simply because of “unprecedented demand.” While the FDA hasn’t (yet) officially listed it as in shortage, patients are having a hard time getting it. “It’s like The Hunger Games,” said the president of the Obesity Medicine Association. “Well, actually more like the anti-Hunger Games.” A new report from the Global Health Technologies Coalition and Australia’s Policy Cures Research — two organizations that look at how biomed investment affects poorer countries — found that when the US government invests in health research around the world, it not only helps in the short term, it pays some serious long-term dividends. Our $46 billion in healthcare-research spending (over 15 years)… … gave rise to $104 billion in economic activity, created 600,000 new jobs, and is expected to spur another $102 billion in industry investments in the United States and beyond. And that’s on top of preparing us at home for various tropical diseases that are making their way north. Not to mention that, you know, healthy people produce more, create jobs, and of course pay taxes. “Oatzempic’ — how drinking watery oatmeal with lime can help you lose 40 pounds in just a couple of months. (Spoiler: It can’t.) “Believing what is being said on social media can be like believing everything that people say on dating app profiles.”Salt is deadlier than expected, plus TB on the rise, respiratory viruses on the decline, and more
Insulin under pressure
Salt really does kill
Diseases on the march
Grandma and grandpa are letting their guards down
Consumption is jumpin’
Big ol’ study: Chronic fatigue is real
Short takes
Managing cannabis expectations
Respiratory virus update
Patients can’t get Zepbound
Shocker: Investing pays returns
Today’s TikTok dopiness
March 30, 2024 ✒ Andrew Kantor
GLP-1 drugs are still not approved by Medicare for treating obesity, but they are approved for treating diabetes and cardiovascular issues. And that alone means that “Medicare Spending on Ozempic and Other GLP-1s Is Skyrocketing.” Ozempic alone accounts for 2% of the entire Medicare Part D budget. Think about that — and think about what’s going to happen when GLP-1s are approved for more conditions. The blockbuster diabetes drug Ozempic could be manufactured for less than $5 a month, even as Novo Nordisk charges almost $1,000 per month for the injection in the U.S. before insurance, a new study suggests. Researchers found that a month’s supply of the treatment could be made for an estimated 89 cents to $4.73, figures that include a profit margin. (Emphasis ours.) Pharmacists! Technicians! Get yer immunization training! GPhA is offering the two most popular courses in our library on the same day: Saturday, April 20 at the Marriott City Center in Macon (map). Both include in-person and home study, and both give you the training you need to keep up with the latest in immunization best practices. For pharmacists: The live portion of “APhA’s Pharmacy-Based Immunization Delivery: A Certificate Program for Pharmacists” is from 8:00 am to 5:00 pm. It’s $349 for GPhA members ($499 for non-members). Click here for more info. For technicians: The live portion of “GPhA Immunization Training for the Pharmacy Technician” is from 3:00 to 5:00 pm. It’s $199 for GPhA members ($249 for non-members). Click here for more info. And both give you a nifty certificate for your wall that you can use to impress you boss and your patients. Sign up now before they fill up! If you have any info about the hackers that attacked the Change Healthcare network, there’s a $10 million reward “for information that would lead to the identification or location of anyone who engaged in the ‘malicious cyber activities’ against U.S. infrastructure on behalf of a foreign government.” According to UVA researchers, long Covid might be caused by “abzymes” — antibodies the body produces in response to the disease, but that act like enzymes. They end up interfering with processes that you probably don’t want interfered with, like blood pressure, clotting, and inflammation. If patients with long COVID make abzymes that activate proteins that control processes such as coagulation and inflammation, that could explain the source of some of the long COVID symptoms and why long COVID symptoms persist even after the body has cleared the initial infection. It also may explain rare side effects of COVID-19 vaccination. Right now this is still in the “hypothesis with some evidence to support it” stage, so — as always — more research is needed. In rural areas, people can have multiple addictions — having both alcohol- and opioid-use disorders isn’t uncommon. The problem, found UCLA researchers, is that even though both disorders can be treated at the same time, most patients were only treated for one or the other. In all, 85.3% of patients with a dual disorder were prescribed a medication for only one condition, compared to patients struggling with opioid use only (63.7%) or those battling alcohol issues only (10.3%), the study found. And it’s not as if treating both is complex. Naltrexone does the trick. So what’s happening? They don’t know. They do know that these folks need more support than they’re getting, but medical care is hard enough to come by in a lot of rural areas. It can help prevent the recurrence of colorectal cancer. A new Dutch/French study of 1,719 patients with colorectal cancer found that “[C]onsuming >4 cups/day of coffee compared to an intake of <2 cups/d was associated with a 32% lower risk of CRC [colorectal cancer] recurrence.” Bird flu has jumped to dairy cows in at least three states. That is all. “Eggs May Not Be Bad for Your Heart After All” reads the headline. They might not affect cholesterol, and they might even be good for people with diabetes. Who woula thunk? It’s been appearing in various news outlets, too, just in time for Easter. One thing, though: The study was funded by Eggland’s Best — a brand of eggs. It also refers to fortified eggs, not your run-of-the-mill eggs. Your grain of salt Coffee vs. colon cancer, the reality of GLP-1 pricing, iffy egg news, and more
The crazy cost of GLP-1s
Meanwhile….
Double-whammy immunization training
Reward!
The latest cause of long Covid
Half-help for rural folks
Short takes
Coffee’s latest trick
Still nothing to see here, citizen. Move along
Questionable egg news




