March 28, 2024 ✒ Andrew Kantor
Scammers are targeting pharmacists, and they’re sophisticated enough to fool even the smart ones. One pharmacist in Ohio lost her life’s savings when scammers posing as the board of pharmacy — even with the BoP’s Caller ID — convinced her she needed to put up a $500,000 bond to avoid arrest from a narcotics investigation. The caller said that her pharmacist license had been linked to a narcotics investigation in Texas and there was a warrant out for her arrest. Her license – which pharmacists need to work – was at risk, the caller said. She would need to post a $500,000 bond or work with the FBI to clear her name. […] Over three months, she was terrified and followed the directions of people she thought were agents of the pharmacy board and other authorities. The scam went pretty far, including having a dark SUV to follow her occasionally. In the end, the pharmacist lost nearly everything. (And no, there’s no way to get that money back. It’s gone.) “Gift card” scams are obvious, but when your professional life seems to hang in the balance, it’s easy to miss any signs of shenanigans … if there are any. When in doubt, contact the office directly (in this case the Board of Pharmacy), using a phone number you’re certain is correct — not what the scammer gives you. And we won’t get into how AI is being used to sound like someone you know pleading for help…. Women are reporting getting pregnant while on GLP-1 drugs, even though they use birth control (or in some cases thought they were infertile). But before you raise your eyebrow, keep in mind these women are on TikTok, so you can’t really take what they say at face value. (Were they on real birth control? Were they really infertile, or just hadn’t conceived yet? Was is just a coincidence they got pregnant while on Ozempic?) That said, there is the possibility — raised by actual scientists — that GLP-1s interfere with birth control by slowing the drugs’ absorption, but it’s more theoretical than proven. All that said, keep in mind that being pregnant while taking GLP-1s is risky, “and women need to be monitored very closely.” As the out-of-pocket price of insulin has finally dropped thanks to pressure from various governments, you would assume insulin use would increase as more people could afford it. Strangely, though, those insulin price caps haven’t increased insulin uptake. One reason might be that the people who it affects most — those with commercial insurance — are more likely to be able to afford it, and thus less affected by price caps. (“Previous studies found Medicare enrollees’ prescription fills rose after Medicare implemented a new $35 cap on monthly insulin costs.”) But that’s just speculation. Markets are complicated beasts. Taking statins, it seems, can reduce your risk of gum disease. And considering gum disease can raise your risk of cardiovascular problems, it’s a double bonus. Researchers at the College of Dental Medicine at the Medical University of South Carolina found that statins (specifically simvastatin) turned down the responses of macrophages in the gums, meaning there was less inflammation and thus less chance of Bad Things like tooth loss of the need for root canal. Should statins be prescribed for people at risk for gum disease? Or could they tease out the mechanism and create a more-targeted drug? You know the mantra: More research is needed. “Positive Causal Link ID’d Between Computer Use, Erectile Dysfunction”. What’s interesting is that it’s not as simple as ‘more computer = less rising to the occasion.’ What Chinese researchers found is that men who were genetically predisposed to “leisure computer usage” were more likely to have trouble — how shall we put it? — leveling up. Interestingly, it’s only computer use that’s a problem, not sedentary behavior overall: There was no evidence seen of a link between watching television or driving for leisure and an increased risk for ED. A Philly-based company called Every Cure is into drug repurposing, but in a big way. Rather than seeing if Drug X can be used for Condition Y (or even “What conditions might Drug X treat?”) it’s using AI “to compare all drugs and all diseases.” While other organizations doing this kind of work may focus on a specific drug or disease, Every Cure looks at all cases, with the goal of making the connections that will impact the greatest number of patients. Chickenpox has been reduced so much in the US (at least until anti-vaxxers target it) that “the disease is now so rare in the US that doctors are misdiagnosing it half the time, according to a report from the Minnesota Department of Health.” What patients turned out to have was usually an enterovirus or simply “some other skin lesions or infection that was mistaken for chickenpox.” “Gotta go? New bladder device lets you know” It seems that with GLP-1 drugs being all the rage, people have forgotten that there have been other weight-loss drugs available for a long time. They’re “Half as Good as Ozempic for One-30th the Price,” but as one obesity doctor put it, when they came out “We didn’t have TikTok.” Those older drugs might have issues, of course, but they’re also usually covered by insurance and available as generics. They just don’t have the buzz. Pregnant from Ozempic? Plus sneaky pharmacy scams, why guys should avoid the computer, and more
Be careful out there
Ozempic … babies?
Economics is never simple
The X for Y files
Guys, maybe you shouldn’t be reading this
Short takes
Old drugs, new uses
Chickenpox mimics
You definitely want to choose your notification sound carefully
The Long Read: Pre-Ozempic edition
March 26, 2024 ✒ Andrew Kantor
One thing a lot of providers are learning after the UnitedHealth attack is that they need to think more about their cyberattack insurance. This sounds like I’m going to try to sell you something. I’m not. The gist is that their insurance might cover if something happens to them, but not if it happens to, say, their payment provider. So when patients sue, their insurance company will say, “We’re not paying because we don’t cover United Health. We cover XYZ Pharmacy.” (Here’s an analogy: Imagine your brakes are defective and you get into an accident, but your insurance company says it won’t pay because it covers you, not the company that made your defective brakes. It’s your problem to deal with BrakeCo — but meanwhile the guy you hit wants payment.) Thus even companies with cyberattack insurance are finding the limitations of those policies, while they’ve got patients demanding recourse. Eventually UnitedHealth will probably make everyone good, but that may be too late for a lot of small practices. It’s out! The CPE courses list for the 2024 Georgia Pharmacy Convention! That means instead of saying, “We have tons of CPE,” now we can say, “Check out the list of CPE courses you can take!” That full course list for the convention is right here, and more importantly the registration link is here: Medication errors are too often the cause of hospital readmissions — the transfer of patient data from inside pharmacist to outside pharmacist isn’t always smooth, especially when there are multiple specialist prescribers involved. A transition-of-care pharmacist can cut down medication errors, but that’s a lot of hours (30 to 50 minutes per discharge, multiplied by dozens of patients). Humans are slow. That’s why West Virginia University pharmacy researchers are developing an AI tool to The AI will do more than review a list of meds for potential interaction. It’ll be able to read clinician notes and medical history as well. “[I]n each patient’s profile, the tool will also be able to determine the risk of readmission and create an alert system for pharmacists.” As the 2024 legislative session winds down, we had some good news and some bad news in a very busy week. Check out Melissa Reybold’s latest Legislative Update for the details. Eli Lilly says its 10 mL vials of Humalog and Lispro injections are both in temporary shortage — meaning through the beginning of April. “Patients who need insulin immediately and cannot access their healthcare provider for an alternative treatment option should seek emergency care.” Adherence is a problem with any drug that needs to be taken for the long-term, but there seems to be one exception: the new obesity drugs. The limited amount of anecdotal reports so far indicate that “Patients seem to take them faithfully, week in and week out.” (Side note: A lot of patients didn’t start using them once they learned they had take them forever.) If you’ve ever caught or eaten catfish, you’ve undoubtedly asked yourself, “What can be done with all this lovely mucus?” Scientists at UC Davis decided to find out. Turns out there’s “a compound with powerful antibacterial properties” in there. It’s even safe (in general) for mammalian cells, but whether it could lead to a drug for humans is another question entirely. Kids who ride in newer school buses do better academically than the ones stuck in the older ones. What makes this study out of the University of Michigan interesting is that the buses were replaced randomly — i.e., it’s not as if kids in affluent districts did better. It was all about the bus. [A]mong districts randomly selected by the EPA to receive funding to replace the oldest, dirtiest, buses (pre-1990) with newer, cleaner buses, educational performance improved after the new buses were in use. Replacing newer buses, however, did not show the same benefits. So how did cleaner buses mean better test scores? Kids who rode cleaner buses were out sick less often. (Especially those with asthma, not surprisingly.) As for the affluence thing, the UMich folks said the improvement was equivalent to moving to a richer neighborhood (10% and 4% higher for reading/language arts and math, respectively) or having classes that were reduced by 7 to 10 students. (Because the US isn’t wealthy enough to upgrade old buses across the country, the EPA has an annual funding lottery to choose randomly which school districts can get them.) A study out of Dartmouth is getting a lot of airplay even though it’s about a condition that affects fewer than 100 people. It’s called prosopometamorphopsia or PMO, and people who have it see faces as freakishly distorted. (Live ones, anyway. Photos and drawings look normal.) The CNN story goes into a lot more detail, including an interview with a patient who explained “It’s like staring at demons. Imagine waking up one morning and suddenly everybody in the world looks like a creature in a horror movie.” Yeah, that’s right — it happened all of a sudden when he was about 56 years old. Some people with PMO see their own faces as distorted or even damaged. Two patients, “while standing in front of the mirror, saw one eye popping out of its socket and slithering down the cheek.” […] one patient described the right side of his doctor’s face in which the “eye became a ghastly staring hole, cheek bone a cavity; he had teeth on the upper lip, often had two ears.” Others with PMO have eloquently described faces as “like clocks in a Dalí painting” or “kaleidoscopically changing.”Lilly’s insulin shortage, cyber insurance failures, the better-school-bus effect, and more
Learning the limits of cyberattack insurance
Convention CPE course list released
 Remember: Early-bird registration for the convention ends March 31, so there’s not much time left to get the best rate. Go forth and register now!
Remember: Early-bird registration for the convention ends March 31, so there’s not much time left to get the best rate. Go forth and register now!A pharma AI to cut readmission
take their place help reduce their workload.The latest legislative update
Short takes
THIS drug I’ll stick with
Slimy goodness?
Better buses, better students
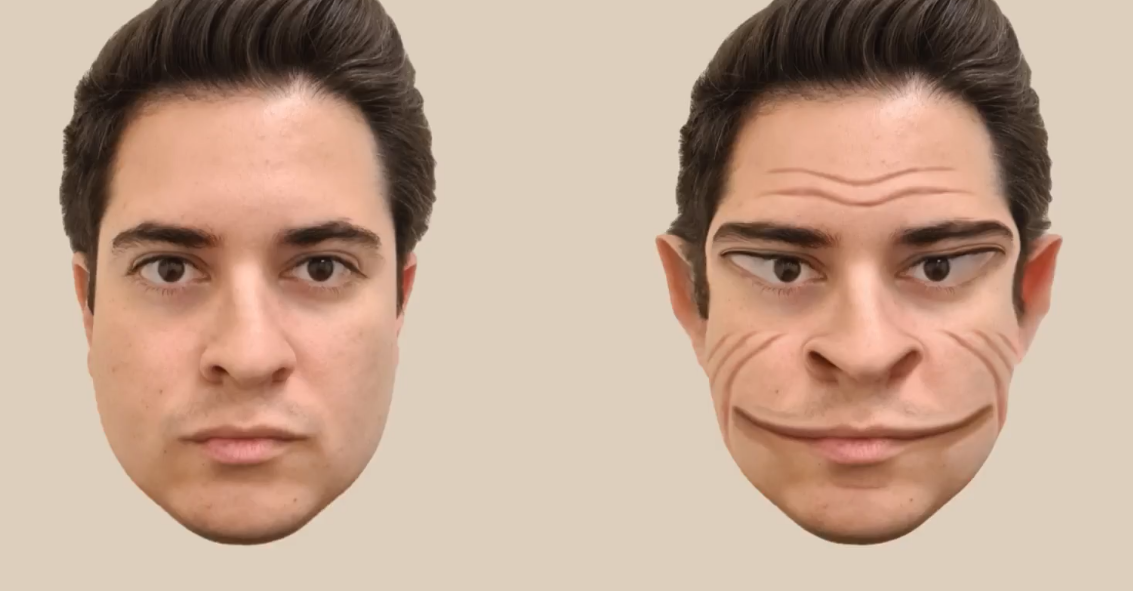
ICYMI: Face the face
March 23, 2024 ✒ Andrew Kantor
It’s the first GLP-1 weight-loss drug the program will cover, because it’s not technically a weight-loss drug — it’s only been approved for treating heart problems by CMS following the FDA’s approval of the drug for that purpose. So don’t be surprised to see some wink-wink from prescribers on this one. Apparently being double-joined increases your risk of long Covid. What do you call a woman who gets her birth control information from TikTok? “Mom.” Following in the footsteps of Boehringer Ingelheim and AstraZeneca, now GSK says it will cap the prices of its inhalers at $35 out of pocket … well, starting in 9 months. If someone’s got a corneal abrasion, why give them eye drops they must put in manually when you can have ’em pop in a contact lens that delivers antibiotics automatically* — while also acting as a bandage? That’s just what Canadian scientists developed because (unlike you and me) the lead researcher “knew there was a market for a drug-delivering bandage contact lens that could simultaneously treat the eye and allow it to heal.” If delivering drugs via contact lenses isn’t cool enough, here’s a twist: It reacts to an enzyme in the eye* that’s released during wound healing. Thus the lens… “… releases the drug in a way that is proportional to the amount of enzymes present at the wound. So, the bigger the wound, the higher the amount of drug released.” And yes, someone did call it “potentially a game changer.” * Matrix metalloproteinase-9 (MMP-9), as you probably guessed Usually you hear about amino acids having a positive effect on health — precursors to proteins and all that. But University of Wisconsin researchers found the opposite: Mice that cut down on their intake of isoleucine lived longer, got thinner, were less frail as they aged, and didn’t have as much cancer or as many prostate problems — even when their calorie intake was higher. The UW folks also found that obese people had more isoleucine in their bodies, confirming their suspicions. So what foods contain isoleucine? Yeah, that’s the problem: “Isoleucine is plentiful in foods including eggs, dairy, soy protein, and many kinds of meat.” Rather than count on people changing their diets, the scientists hope to figure out the mechanism at work and use it as a treatment target (or possibly find a way to block isoleucine absorption). APhA and the National Alliance of State Pharmacy Associations released their 2003 “Pharmacy Workplace and Well-being Reporting,” highlighting what pharmacy staff report are the biggest issues in their pharmacies. You can read the full report here (PDF), or just check out the news release here. Or you can cut to the chase and ponder the 10 most-reported issues: The Candida albicans fungus can be a big problem in hospitals. Usually it’s benign, sometimes it causes thrush, but too often it can lead to invasive candidiasis, where it infects the blood or the organs. If that happens, there’s a 25% mortality rate. There aren’t any great treatments for candidiasis, and killing C. albicans is tough — although that may have changed. Rather than a drug, Israeli researchers have found another fungus that outcompetes C. albicans, clearing it out of the intestines and reducing the risk of runaway infection. They named the new fungus Kazachstania weizmannii, and they found it living happily in human guts. In fact, where there is K. weizmannii you don’t find C. albicans, and vice-versa, meaning it sure looks like it could be weaponized. There are only 276 days till Christmas, so the folks at Drug Store News are wondering, “What will consumers’ shopping behavior look like for the 2024 holidays?” The answer: deals, discounts, and online shopping with free shipping and customer reviews. But don’t you worry — “[N]early 60% of all U.S. and U.K. respondents plan to attend Black Friday and Cyber Monday* physical events during the holiday 2024 season.” * Sure, shopping in person for Cyber Monday. That makes sense.Latest pharmacy workplace report, TikTok’s birth control misinformation, fungus fighting fungus, and more
Medicare to cover Wegovy
Short takes
Sure, why not?
Who woulda thunk?
Another inhaler price drop
Drug-delivery contact lens
The acid that makes you fat, frail, and sick
How you doin’?
Fighting fungus with fungus
Never too early
March 21, 2024 ✒ Andrew Kantor
There are a lot of competing explanations for chronic fatigue syndrome (CFS) and a good chance it’s got several possible causes. The latest one, though, is interesting: SSRIs. Korean researchers think CFS might be caused by excessive levels of serotonin in the brain. Thus SSRIs, by their very action, keeps those levels higher. To test this, they gave some mice high dozes of Prozac and others plain ol’ saline. Not surprisingly, after a month the brains of the Prozac group had higher levels of serotonin. But the interesting bit: They also developed behaviors that resembled the main symptoms of ME/CFS seen in humans, including unrefreshing sleep, PEM and orthostatic intolerance, but not cognitive impairment. These behaviors disappeared six weeks after the drug was stopped. Next up: Figuring out the molecular mechanism at work. Move over, cardiovascular disease. The latest research (out of US and Australian universities and the WHO Brain Health Unit) finds that neurological conditions have taken the top spot — that’s “stroke, brain injury, migraine, Alzheimer’s disease and other dementias, and nerve damage.” What’s going on? We’re getting older. Oh, and there’s “increased exposure to environmental, metabolic and lifestyle risk factors,” which is why diabetic neuropathy is skyrocketing. The good news? Despite the rising levels of neurological disease, both deaths and years “lost” to disability are down, thanks to better treatments … in the developed world, at least. Thanks to health Athletes who want every little edge possible might want to look at everyone’s favorite Thanksgiving side dish: cranberries. Yep, apparently taking cranberry extract means “better oxygen extraction by the muscle, improved lactate clearance, and slower muscle deoxygenation,” according to Quebecois researchers. (They might be a bit over-enthusiastic, though, calling cranberries “A runner’s best friend.”) A group of Welsh, Canadian, Chinese, and American researchers have reached the conclusion that if you have a mild case of Covid-19, it’s fine to take over-the-counter drugs to relieve the symptoms. But… Researchers at Florida Atlantic University say ‘not so fast’ — talk to a professional before doing something rash like taking Tylenol. They suggest that selecting an OTC medication to alleviate mild symptoms of Covid-19 should be based on the entire benefit-to-risk profile of the patient. Moreover, they say clinical decisions should be made by the health care provider for each of his or her patients. Acid-suppression meds and infants don’t mix, and it’s especially true for proton-pump inhibitors. Apparently those kinds of meds can increase the risk of a kid developing a food allergy. Based on data from… … Cleveland Clinic researchers found that “early exposure to acid-suppressive medications was associated with five to six times higher risk of food allergy and anaphylaxis, with similar trends observed for antimicrobials.” Yeah, five to six times the risk. That’s not small potatoes. And PPIs had the highest risk — 640% higher than average. Why? Dunno — someone else will have to figure that part out. For now, though, it’s a risk worth telling patients about. Humans can’t digest plants directly, but we’ve got gut microbes that do it for us. Here’s the problem (according to a study by Israeli researchers): Western diets are so low in the fiber that cellulose-eating bacteria need, we’re reaching the point that we can’t process plants at all. They looked at gut bacteria today and from humans more than 1,000 years ago, as well as in non-human primates. Back then (and in today’s wild primates), about 30-40 percent of gut bacteria was the stuff that could digest cellulose. Today, it’s down to 20 percent at best— and that’s in hunter-gatherer cultures (and people living a rural lifestyle with high-fiber diets). For people living modern lifestyles, only 5 percent of their gut bacteria can process plants. What does that mean? It means that we’re not getting as many of the nutrients in plants as we used to, and it’s getting worse. How will that affect health? You know the mantra: More research is needed. But for sure we need more fiber either in our diets or, well, maybe via supplements you have down this aisle right here….Cranberries for runners, surprise fatigue trigger, everyone wants glucose monitoring, and more
Antidepressant fatigue
The new worst conditions
Short Takes
Glucose monitors go mainstream
infomercials influencers and corporate marketing, diabetics aren’t the only ones looking to buy continuous monitors. They’re turning into TKTKThe cranberry boost
There is no news here
Suppress the acid, get the allergies
We’re losing the ability to digest plants
March 19, 2024 ✒ Andrew Kantor
When someone is diagnosed with type-1 diabetes, they often still have functioning pancreatic beta cells that keep working for years. They’ve got a “honeymoon period” before full-on diabetes sets in — time to make lifestyle changes to try to keep the diabetes at bay. Just like with marriage or a new job, being able to extend that honeymoon is a Good Thing, and a group of researchers (from too many institutions to list) think they’ve found a pill that will do it: ergocalciferol, aka vitamin D2. They ran a trial on 36 kids who had just been diagnosed and… … found that those volunteers given the vitamin D2 supplements saw improvements in insulin secretion capacity in beta cells—they observed decreases in the PI:C ratio compared to a placebo. Of course the trial was small (more research is needed), but considering that vitamin D3 gets all the love, it might be a chance for D2 to shine. As much fun as it is to wear a CPAP and make Darth Vader sounds*, Aussie researchers may have found a pharmaceutical solution. It’s a potassium channel-blocking nasal spray that has “the potential to increase the activity of the muscles that keep the upper airway open and reduce the likelihood of the throat collapsing during sleep.” They started with a small test — 10 volunteers — and got some good results: Seven out of the 10 people responded to the potassium channel blocker nasal spray showing a reduction in the frequency of upper airway collapsing episodes during sleep and lower blood pressure the next morning. Side note: With nasal-only breathing (we presume they taped shut the mouths of some volunteers), the spray didn’t help. * Or mimic Bane’s voice, for you Dark Knight fans The FDA has approved Madrigal’s Rezdiffra (resmetirom, to be technical) as the first drug ever for metabolic dysfunction-associated steatohepatitis (MASH), aka liver inflammation. Following in the footsteps of Boehringer Ingelheim, AstraZeneca now says it’s also going to offer a savings program so no one has to pay more than $35 a month for any of its asthma inhalers. This isn’t the same as lowering the price — perish the thought! — rather the company is making coupons available. Whether pharmacists and patients will be aware of those coupons … well, that’s another matter. As we’ve seen with insulin, it’s not even close to 100%. FYI, nine more drugs are in shortage (other than the ones you probably already know about) according to suppliers: We know that your various microbiomes are important, and that there are “good” and “bad” bacteria living in and on you, but the details are still being sussed out. Which bacteria are important for which people in which nooks and crannies is not 100% clear. But that doesn’t stop nefarious companies from offering at-home tests to tell you whether a particular biome is healthy or not … and, of course, selling you something to “fix” it. Thus a group of medical and pharmaceutical researchers has written an article in Science calling for more regulation of those tests, lest consumers be “financially exploited or harmed by inappropriate use of test results that neither they nor their doctors understand.” “There is no scientifically agreed-upon definition of a ‘healthy’ microbiome; the microbiome is dynamic and changes frequently; there is no clinical proof that these products work; and no standardization in the processes involved.” What’s the current respiratory virus situation? Here, have a chart: “Using X (formerly Twitter) has a negative impact on well-being” “…it was associated with an immediate drop in positive emotions such as joy and a surge in outrage, political polarization, and boredom.” Way back in August 2023 we told you how the first pill for postpartum depression — Zurzuvae (aka zuranolone) — got FDA approval and would be hitting pharmacies soon. Well that happened, but there’s a catch. Sage Therapeutics set Zurzuvae’s price at $15,900 for the 14-day regimen. And that means insurers are iffy about covering it or even offering guidance. Meanwhile, patients are waiting.Twitter is depressing, extending the diabetes honeymoon, more inhaler coupons coming, and more
D2 is for diabetes
Apnea drug for mouth breathers
Short takes
First drug for MASH (aka NASH)
AZ offers more inhaler coupons
More drugs in shortage
Experts: Don’t trust biome tests
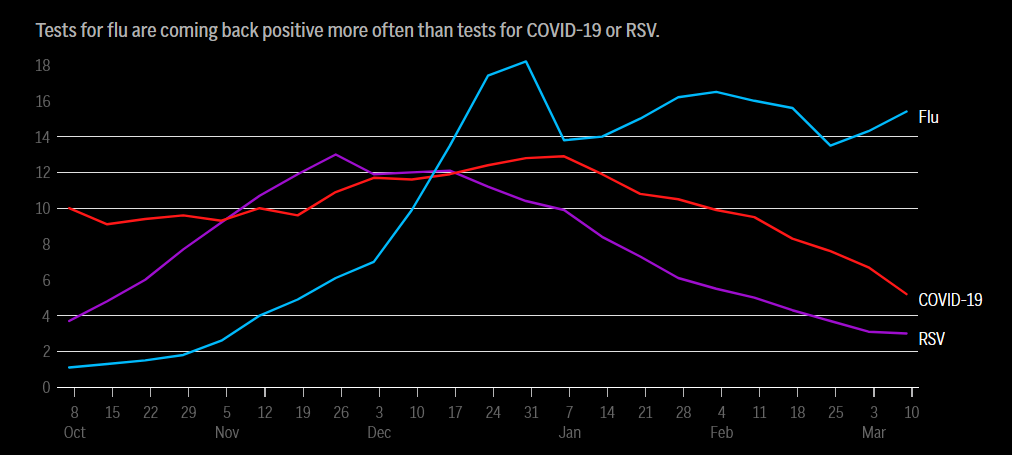
Respiratory update
Captain Obvious has dusted off his Tumblr account
The Long Read: Postpartum med remains elusive
March 16, 2024 ✒ Andrew Kantor
UnitedHealth Group reports that its pharmacy systems are back online, more than three weeks since it was attacked by an unnamed foreign government. The healthcare conglomerate expects the payment platform to be functional and begin restoring the medical claims network starting mid-March. UnitedHealth is likely to need several months to make a full recovery, according to security experts. There are some people, surprisingly, who don’t like either the idea of a colonoscopy or pooping into a cup. There’s good news on the horizon, though, as researchers at Seattle’s Fred Hutchinson Cancer Center have developed a blood test that’s as accurate as at-home poop-in-a-bottle tests. Of the 7,861 people included in the report, 83.1% of those with colorectal cancer confirmed by colonoscopy had a positive blood test for circulating tumor DNA. Meanwhile 16.9% had a negative test — in which a colonoscopy indicated colorectal cancer but the ctDNA test did not. It’s not as good as a colonoscopy, but it’s “an early effort” and could very well get more accurate over time. More importantly, it could mean a lot more people get screened and a lot more cancer gets caught early. The company that developed it, California-based Guardant Health, says the FDA will be reviewing the pre-market application in late March. If approved, Guardant will charge $895 for the test, which will hopefully be covered by insurance. …to Mercer College of Pharmacy’s Dean Brian Crabtree, who will be stepping aside at the end of July. He’ll be succeeded by Pamela Moye, currently a clinical professor of pharmacy practice, effective August 1. If the risk of a brain-eating amoeba isn’t enough to keep you from putting tap water into a neti pot, how about two brain-eating amoebas*? Yep, the CDC has confirmed that Acanthamoeba, although extremely rare, can be found in tap water — and if it gets into your nose it can eat your brain. * Amoebi? You might want to stop giving licorice to kids as a punishment. Swedish researchers have found that even a small amount can raise blood pressure. “This is mainly due to a substance called glycyrrhizic acid that affects the body’s fluid balance through effects on an enzyme in the kidney.” (Previous research suggested that it took a large amount to have the hypertensive effect.) A cow in Brazil has been genetically engineered to make human insulin in its milk. What makes this attempt different is that the technique only affects the DNA of the mammary tissue. Oh, and it worked: “Our goal was to make proinsulin, purify it out to insulin, and go from there. But the cow basically processed it herself. She makes about three to one biologically active insulin to proinsulin.” It’s still proof of concept, but the concept was proven. Next up will be to perfect the technique; this first cow couldn’t be impregnated, so they had to use hormones to induce lactation, resulting in less milk (and insulin) production. Money quote: “The mammary gland is a magical thing.” The other day we told you how when tryptophan is broken down in the gut, it produces byproducts that can lead to arthritis. But don’t give up on Thanksgiving turkey just yet. It turns out that tryptophan has another (good) trick up its sleeve: It can protect you from E. coli. Apparently (found Cornell researchers) some of the metabolites it breaks down into can make it harder for E. coli to attach to the lining of the gut and cause an infection. Instead, thanks to the tryptophan, “the pathogen benignly moves through and passes out of the body.” We all know that the maternal death rate in the US is awful, way behind other modern countries, and has been getting worse. Or do we? A group of Canadian researchers looked more closely at the data and conclude that the sky is, in fact, not falling. In short, the National Vital Statistics System counted any death where the victim was pregnant as a maternal death. Pregnant and killed in a car accident? Maternal death. Cancer? Maternal death. It’s even worse than that; sometimes that “Pregnant” checkbox was ticked by mistake: For example, hundreds of decedents, 70 years of age and older (including 147 women aged 85 years and older in 2013), were certified as pregnant at the time of death or in the year prior. The good news: Recalculated, the US maternal death rate is about 10.4 per 100,000 live births — half what the NVSS reported. The bad news: In contrast, Norway’s is 1.66. (Canada’s is 11.0 and Portugal’s is 11.8, so we’re not at the bottom of the barrel.) Paxlovid is far from perfect, but it’s still pretty good at keeping mild Covid from becoming not-so-mild Covid, and just as important for reducing the risk of long Covid. So why aren’t more people using it? There’s not one answer, but lack of knowledge — by patients and pharmacists — is high on the list.Cow makes insulin, colon-cancer blood test, neti pot danger x 2, and more
Change is back (sort of)
Colon cancer: no more probes or bottles?
A fond farewell…
Short takes
Put the distilled water next to the neti pots
Why do they even sell this stuff?
Insulin-making cow
Tryptophan’s good side
US maternal deaths
The Long Read: Missing Out on Paxlovid edition
March 14, 2024 ✒ Andrew Kantor
It’s been 18 months since Adderall officially went into shortage, and since then other stimulants have joined the list. Bad news: “[C]linicians and advocates alike say there is no apparent end in sight.” The good news is that there’s plenty of time for finger-pointing and plenty of places to point: manufacturers, PBMs, prescribers, the DEA, the FDA, telehealth, and of course politicians from The Other Side. Interesting side note: The shortage primarily affects generic versions of the drugs — in several cases (Vyvance, Concerta) the branded version is available, just much costlier. Yep, people with ADHD who are on medication can have their risk of death cut by a quarter. And that’s not just from natural causes, but from unnatural causes as well, including accidents and overdoses. To reach this conclusion, Swedish researchers (with help from US and UK colleagues) “followed nearly 150,000 Swedes aged 6-64 who were diagnosed with ADHD between 2007 and 2018.” They can’t say for certain exactly what the causal relationship is, but the connection is clear. Considering that people with ADHD are among the brightest and most productive, it’s important to keep them alive lon— When everyone’s favorite Thanksgiving-sleepiness punching bag is broken down by gut bacteria, some of the byproducts — particularly indole — can lead to inflammation. “We found that when indole is present, the mice start to develop autoreactive T-cells that are more inflammatory. They have less of those regulatory T-cells that help maintain balance in the immune system, and they start to develop antibodies that are more pathogenic. We found that the antibodies had flags for being more inflammatory when indole was present.” So wrote University of Colorado researchers who made the discovery. There’s good news: Knowing that “indole generation” can lead to arthritis means it might be a therapeutic target. Even better, tryptophan is also broken down into some anti-inflammatory compounds, so blocking indole would mean two steps forward. The FDA has given a breakthrough designation to Mind Medicine’s LSD-based drug, MM120. It still has to go through the whole approval process (and get its forever name), but at the moment it’s new and different enough to get the red carpet treatment. Said one researcher, “I’ve conducted clinical research studies in psychiatry for over two decades and have seen studies of many drugs under development for the treatment of anxiety. That MM120 exhibited rapid and robust efficacy, solidly sustained for 12 weeks after a single dose, is truly remarkable.” Back in May 2023 we told you how kids were overdosing on melatonin thanks to parents being unaware of the dangers of giving them too much. (It doesn’t help that what’s on the label and what’s in the drug don’t always jibe.) It’s bad enough when unwitting parents are overdosing their, but the OD trend is apparently being compounded by kids getting their grubby little hands on high doses of melatonin accidentally. The fact that the drug comes as gummies and without childproof packaging certainly makes that easier. All this comes from the latest of the CDC’s Morbidity and Mortality Weekly Report, which found that a whopping 70% of kids’ visits to the ER for medication exposure was for “unsupervised melatonin ingestion.” That was about 11,000 kids from 2019 to 2022, and gummies were their preferred method of dosing. Fun fact: Despite what 70% of primary care physicians think, melatonin is not recommended for insomnia. Having contracted polio in 1952, he was the last person to be kept on an iron lung. He died this week at age 78. Adding minerals to table salt is an easy way to get people the nutrients they need. In 1924, the US started adding iodine to salt to help tackle iodine deficiency, which can lead to stunted intellectual development. IQs literally rose after iodized salt was introduced. All that said, a new study (that included Emory University) found that adding folic acid to salt can reduce major birth defects, notably spina bifida and anencephaly. In the US and a bunch of other countries we add folic acid to grain for just this reason, but other countries can’t afford to do that. This new study proved that using salt worked just as well, while being a lot cheaper. “We proved that folic acid can get into the blood through salt. Hopefully countries that have not already implemented fortification programs can now look at their infrastructures and realize that salt fortification is cheap and it’s really easy to add in the amount of folic acid needed to save lives.”ADHD drugs cut death risk, leprosy returns to the South, another melatonin danger, and more
No, you won’t be seeing ADHD drugs anytime soon
… which is too bad, because they might reduce the risk of death

Tryptophan might lead to arthritis
A coming “breakthrough” drug … based on acid
Quick Takes
Kids keep OD’ing on melatonin
RIP, Paul Alexander
Salt can carry folic acid (and why that’s important)
March 12, 2024 ✒ Andrew Kantor
For people who live in rural areas, diabetes brings a much bigger risk of end-stage kidney disease, heart failure, and heart attacks. That’s on top of already being at a higher risk of diabetes in the first place. What’s going on? While the University of Maryland researchers say “our study didn’t address why these differences exist,” but … “…we do know that people living outside of city areas are less likely to receive care from diabetes specialists, to receive diabetes self-management education, and to be monitored for diabetes complications.” Twist: People in remote locations — that is, outside even small towns — seemed to have lower risks of diabetes complications like heart failure or dangerously high blood sugar. Untwisted: The UM folks think it might be because those folks are much less likely to see a doctor or visit an ER and be diagnosed in the first place. IT’S TIME TO REACH OUT TO YOUR STATE SENATORS. GPhA’s bill — HB 1363, which would require Georgia’s State Health Benefit Plan to pay independent pharmacies fairly for dispensing medication* — is headed to the Senate. The bill passed the House unanimously, but time is running out to get it heard in the Senate and the session could end without the bill being passed. How bad is the payment problem? Check out our flyer that explains the issue. Trigger warning: If you have an ounce of fairness in you, you’re going to be outraged. PLEASE take a moment to click here and read the details of how you can help with a simple phone call or email. And yes, we’ve included all the info and links you need. This is urgent — pharmacies and patients are relying on us to protect them! * This is obviously the broad-stroke explanation. The bill would require an actuarial study first, and it would use an index-based ingredient cost reimbursement plus a fair dispensing fee to determine payments. One of the issues with gut health is that it’s tricky to take supplements or probiotics and know if they’ll do any good. How can you help the “good” gut bacteria without also helping the “bad” stuff? British researchers have cracked a small part of the code. They’ve found two supplements that are apparently good for the good bugs; they seem to help improve memory and cognitive function: inulin and FOS (fructooligosaccharides). And both of them are cheap and available in supplement aisles — maybe even yours. They found the fibre supplement led to significant changes in the participants’ gut microbiome composition, particularly an increase in the numbers of beneficial bacteria such as Bifidobacterium. While there was no significant difference in muscle strength between the groups, the group receiving the fibre supplement performed better in tests assessing brain function […] together with tests of reaction time and processing speed. Bacteria secrete extracellular vesicles (EVs) — essentially a growth on the outside of the cell that acts “as a cell-to-cell communications system” carrying instructions to grow the biofilm that surrounds and protects the cell. Now Washington State University researchers have found a way to trick the cells by creating “death EVs” that look like the real thing but actually send the message, “Yeah, you can take down that pesky biofilm now,” which is double-plus ungood for the germ. Why yes, a Trojan horse analogy fits perfectly. “Adding the death extracellular vesicles to the bacterial environment, we are kind of cheating the bacteria cells. The cells don’t know which type of EVs they are, but they take them up because they are used to taking them from their environment, and with that, the physiological signals inside the cells change from growth to death.” There’s $5,000 up for grabs — that’s the annual award given to a P3 student pharmacist at one of Georgia’s four pharmacy schools thanks to the Jeff Lurey Independent Community Pharmacy Scholarship. Applications will be judged by the AIP Executive Committee, and the final three applicants will be asked to present to the AIP Board of Directors at AIP’s Macon meeting on April 20, 2024 for final selection. Applications are due by this Friday, March 15, 2024. (The winner will be notified by May 1 so he or she can make plans to attend the convention.) Don’t wait! Click here to apply today! If you want to lower your risk of atrial fibrillation, drink only water and fruit juice … and think twice before the fruit juice. That’s the conclusion of a data review by Chinese scientists who found that more than 2 liters a week of any kind of sweetened drink “is associated with 10% increased risk of incident atrial fibrillation (AFib) compared to non-consumers.” Sweet tea? Out. Diet Coke? Out. Coffee with sugar? Out. Water, it seems, is the only safe thing to drink because even fruit juice is loaded with sugars. We know that sugars are bad, but how can diet drinks lead to Afib, you ask? They contain MSG and aspartame, which “are found to be excitotoxins of cardiac tissue leading to ‘lone’ atrial fibrillation.” Side note: You probably want to avoid bottled water, too, because of all the extra nanoplastics. The only way to be safe Everyone and his mother, especially the federal government and UnitedHealth Group, is trying to A) bring UHG’s network back from the cyberattack, and 2) Get payments to the people who need them most, like small pharmacies and providers. But it ain’t easy.A supplement for memory, call to action on a critical Georgia bill, why you should only drink water, and more
Rural diabetes danger
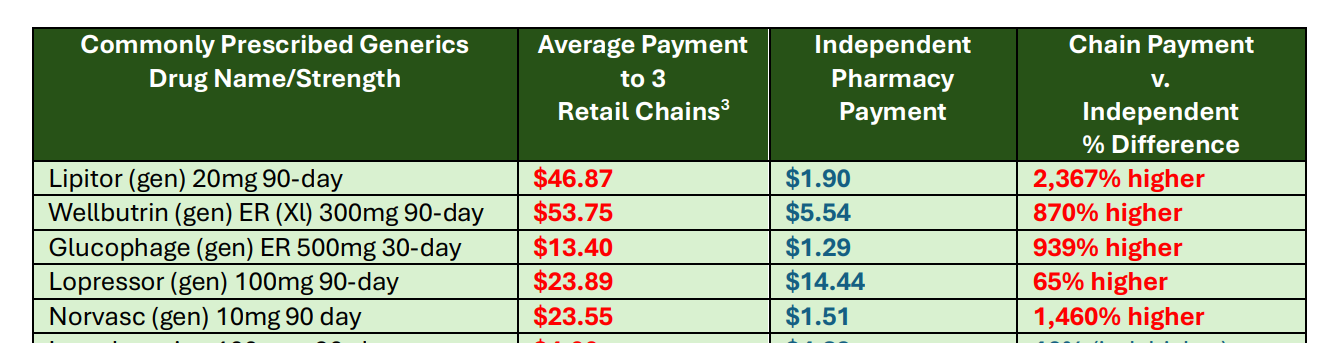
HB 1363 CALL TO ACTION
Memory supplements
Antibiotics: a Trojan horse to kill bacteria
Quick takes
P3 students! Have you applied for the Jeff Lurey Independent Community Pharmacy scholarship?
Who is eligible
What judges will consider (these aren’t requirements, just considerations)
Nothin’ but water

The Long Read: Ransomware Rebound edition
March 09, 2024 ✒ Andrew Kantor
The more severe someone’s psoriasis is, the more likely they are to have some type of inflammatory bowel disease. That’s what Israeli researchers looking at the health records of 61,000 patients found. In fact, someone with psoriasis is 47% more likely to have IBD than someone without it. More importantly, perhaps, was the connection with severity: “Patients with severe psoriasis exhibited a notably higher risk of developing IBD compared to those with mild psoriasis.” Why? The details aren’t clear, but it’s likely because the two conditions “share common underlying inflammatory pathways.” Regardless, they say, it’s worth keeping an eye on folks with psoriasis in case they develop Crohn’s disease or ulcerative colitis. The long-Covid mystery continues, and the latest suspect is iron. Well, the lack of it. A team of researchers from Cambridge and Oxford universities found whether someone contracts long Covid seems to be determined by how quickly their iron levels recover after their infection. People who took a longer time to demonstrate regulation, and had more severe initial infections, were at an increased risk of long Covid. Iron levels drop during infections, but the body’s method of making more red blood cells to compensate is thwarted by Covid’s inflammation. (That also explain why long-Covid sufferers are so tired.) Treating the inflammation might help, but iron supplements won’t: “It isn’t necessarily the case that individuals don’t have enough iron in their body, it’s just that it’s trapped in the wrong place.” Why lose only 6% of your weight in a few months (and have to use an injection) when you can lose twice that with a pill, Jetsons-style? Novo Nordisk wondered the same thing, and now the company says it’s got that high-powered pill. Well, in testing. The company claims that early data show its Amycretin “helped patients in the trial drop 13% of their weight over 12 weeks” with just a daily pill that “targets two hormones involved in regulating hunger and blood sugar levels: GLP-1 and amylin.” Of course, this was just an early trial; phase 2 testing won’t begin until later this year. It was enough to send Novo’s stock price soaring, though, and that’s what really matters. Independent lab (and product watchdog) Valisure says it “found high levels of benzene formed in acne products containing benzoyl peroxide,” and if you remember your 9th grade chemistry, benzene is something you want to avoid. Valisure tested dozens of prescription and over-the-counter benzoyl peroxide products and found that they were “fundamentally unstable and can generate unacceptably high levels of benzene when handled or stored at higher temperatures.” And by “unacceptably high,” they mean 800 times the FDA’s “conditionally restricted” concentration. The issue isn’t with impurities or the quality of the products, but the chemistry of benzoyl peroxide itself — that fundamental instability means it breaks down into benzene. Said the company, “This means the problem broadly affects benzoyl peroxide products, both prescription and over-the-counter, and necessitates urgent action.” “[S]ensory gamma rhythm stimulation clears amyloid in Alzheimer’s mice,” reads the headline. What it means in English is that a combo of flickering lights and clicking clicks at the right frequency — 40 Hz, aka the brain’s “gamma rhythm” — “can reduce Alzheimer’s disease (AD) progression and treat symptoms in human volunteers as well as lab mice.” That’s not from some shady website, either: It’s from a study out of MIT that found his particular frequency had surprising beneficial effects. Why it works … well, that they’re not clear about, although they think stimulating particular neurons at 40 Hz might improve the brain’s waste-removal — specifically “promot[ing] increased amyloid clearance via the glymphatic system.” But, as always, more research is needed. After CFCs were banned as propellants in asthma inhalers in the 1980s, drug makers used the switch to new propellants to extend their patents, especially for HFC inhalers. That means high prices for people without insurance … well, in the US anyway. The same asthma medication for which US patients pay top dollar is available elsewhere at much cheaper prices. Consider the following case for inhalers. The pharmaceutical company Teva sells QVAR RediHaler, a corticosteroid inhaler, for $286 in the US. In Germany, Teva sells that same inhaler for $9. Some uninsured patients cross the border to Canada or Mexico to get , but that’s not possible for most people — they’re stuck with un- or barely-affordable asthma meds. Following the introduction of a generic version of its Spiriva HandiHaler — and accusations by the FDA of patent shenanigans — Boehringer Ingelheim has suddenly announced that starting in June it will cap the out-of-pocket prices of its inhalers at $35 per month. Low doses of ibogaine, a seriously powerful psychedelic, might be a major tool to fight opioid addiction. Lots of people around the world swear by it, but there’s one problem: It’s not legal in the US … yet. In the United States, the renewed interest in ibogaine has largely been fueled by the thousands of Americans who have sought treatment abroad and returned home with tales about overcoming addiction after a single session. The fact that many of them are military veterans has helped ease some of the longstanding institutional resistance to psychedelic medicine.Brain-cleaning frequency, danger lurks in Clearasil, the IBD-psoriasis connection, and more
Unexpected(ish) skin-gut connection
Low iron, long Covid?
Move over, Wegovy
ICYMI: Clearasil releases benzene
40Hz is the frequency, Kenneth
Inhalers: the price of a deep breath
The good news
The Long Read: A different psychedelic
March 07, 2024 ✒ Andrew Kantor
Last month HHS made its first offer for what Medicare would pay for 10 expensive drugs. The drugmakers have now spit on the ground, implied that the offers insult the memories of their dear grandmothers, and made counteroffers that are still cuttin’ their own throats … but acceptable (barely) because HHS is a dear friend of uncle Horace. HHS will now roll its eyes, point out that it could do better in the back alley of a Detroit street market, and respond with a counter-counteroffer that’s still way better than those nogoodniks deserve. And so it will go. Old assumption: GLP-1 drugs slow down the workings of the digestive system, which is what makes people feel full — they are full. New reality: That’s true of natural GLP-1, but the artificial stuff lasts a lot longer in the body; that’s why it’s a weekly injection and not a daily one. By indiscriminately flooding the body with long-lasting molecules, the injections likely allow engineered GLP-1 drugs to penetrate parts of the body that the natural gut hormone cannot—namely, deep in the brain. The brain also has GLP-1 receptors that respond to the drugs. That’s why mouse studies have shown that Ozempic and kin suppress more than the desire to eat (e.g., the desire for alcohol), something that’s echoed in anecdotes from patients who say they’ve quit addictive behaviors. As the headline says, “Ozempic Is a Brain Drug.” Novo Nordisk says it might also slow the progression of chronic kidney disease. Those shifty Danes report that a phase 3 trial found Ozempic “[cut] the risk of death from that and major cardiac events by 24%.” The FDA has approved the first over-the-counter continuous glucose monitor — the Dexcom Stelo Glucose Biosensor System. It uses a wearable sensor (replaced every two weeks) and a smartphone app and, well, continuously monitors their glucose levels. The company says it’ll be available this summer, but hasn’t disclosed the price. The caveat: It’s not for people taking insulin. It’s only approved for people who have diabetes but are managing it via lifestyle changes, e.g., losing weight, exercising more, skipping the Oreos, etc. March 8 is the last day people can ask for them — at least until the feds start the program again in the fall. A new drug fights fatty liver disease with “a one-two punch that shuts down triglyceride production and fatty acid synthesis.” Punch #1: The drug inhibits an enzyme called DGAT2* that the liver needs to make triglycerides. Punch #2: It also decreases the amount of a protein called SREBP-1†, that regulates the expression of genes required for the liver to make fatty acids and triglycerides. The combined effect of stemming DGAT2’s role in triglyceride synthesis and blocking SREBP-1’s role in activating genes involved in fatty acid and triglyceride synthesis stops fat from depositing in the liver, reversing MASLD [metabolic dysfunction-associated steatotic liver disease, aka nonalcoholic fatty liver disease]. The University of Texas Southwestern Medical Center folks who developed the drug are already looking at phase 3 trials “in the near future.” * diacylglycerol acyltransferase 2, since you asked The US will probably be switching from quadrivalent flu vaccines to trivalent ones, as it’s been four years since we’ve seen the influenza B/Yamagata virus — one of the four ‘quads.’ Not seeing that strain means there’s no point including it in the vaccine, and removing it “gives us the space to replace B/Yamagata virus with a component that will give improved protection against the circulating influenza viruses.” “Firearm ownership is correlated with elevated lead levels in children, study finds”GLP-1s are brain drugs, feds and pharma do the dance, an OTC glucose monitor, and more
Capitalism in play
How GLP-1 drugs really work
Speaking of Ozempic …
First OTC CGM
Free Covid tests end March 9
Double trouble for fatty liver
† sterol regulatory element binding protein 1, of course Quad flu vax will probably be retired
Not the most well-thought-out headline, if you think about it



