August 12, 2022 ✒ Andrew Kantor
A new virus — Langya henipavirus (LayV) — has infected dozens of people in China. (“Dozens” = 35.) The question: Is this a legitimate concern, or are we on viral hair-triggers because of, you know, other viruses? The answer, per the GPhA Buzz Crystal Ball™, is … it’s probably nothing to worry about unless you’re a cable news producer looking to fill time. Do you want to worry? Fine, here: “[Other] henipaviruses, like Nipah and Hendra, are known to cause severe illness in humans and animals, with death occurring in 40 to 70% of cases” according to the CDC. A federal judge has ruled that Walgreens contributed to the opioid crisis in San Francisco by dispensing ”hundreds of thousands of red flag opioid prescriptions without performing adequate due diligence.” The sort-of twist is that the ruling is that it’s the company’s fault, not the employees’: “The evidence showed that Walgreens did not provide its pharmacists with sufficient time, staffing, or resources to perform due diligence on these prescriptions.” Walgreens said it plans to appeal, and that it didn’t actually make or market the pills — it just didn’t keep track of how many it was dispensing. Your enemies are in prison, your friends are all French ambassadors. Now it’s time to think: What new pharmacy-related laws should Georgia have? GPhA needs your ideas as our advocacy team prepares for the 2023 legislative session. Our best legislative priorities come from members. You folks are on the front lines, after all, but you have to tell us. And GPhA gets it done with an unmatched record of results: Most of these ideas came from members who told someone on the advocacy team, “There oughta be a law.” If there’s a law or policy issue you want to see changed — something that will improve patient care or the practice of pharmacy — tell us about it! It’s super easy — barely an inconvenience: E-mail your idea to VP of Public Policy Melissa Reybold at mreybold@gpha.org. Yes, it’s that simple. “Dear Ms. Reybold, there’s one law I think Georgia really needs….” Give as much info as you can without boring her. All right, we’ll make it a little harder: You have to do it by 5:00 pm this coming Saturday, August 13. The latest drug that will upend the antibiotic landscape is … fabimycin. Never heard of it? That’s because it’s a new compound developed at the University of Illinois at Urbana-Champaign. Chemists there took an antibiotic that worked against gram-positive bacteria, did a little science to it, and created one they say works against those nasty gram-negative bacteria. And really well, too, fighting off 300 drug-resistant bacteria. “[Fabimycin] proved potent against more than 300 drug-resistant clinical isolates, while remaining relatively inactive toward certain gram-positive pathogens and some typically harmless bacteria that live in or on the human body.” Will we ever hear of it again? After more research, perhaps. Saliva of veterans suffering from Post Traumatic Stress Disorder contains a specific microbiotic signature. That is, it might be possible to test someone for PTSD by looking for a particular combination of bacteria in their saliva. Fun side facts: The Israeli researchers who discovered this also noted that 1) “the saliva bacteria of those exposed to air pollution showed a correlation to the picture with PTSD,” and 2) more education seemed to provide a “protective influence.” “New Study: 36% of YouTube Videos Contain Misleading Hay Fever Information” (The real shocker: “43% of videos on allergic rhinitis contained useful information.”) People with higher levels of cholesterol and fatty acids in their blood are more likely to suffer longer from diseases, and that includes being more likely to have long Covid. British researchers found that, Covid or not-Covid, if someone’s symptoms took longer to disappear, they were like to have the same pattern of harmful fats in their blood. “The blood markers in asymptomatic people had a healthier pattern that we know is associated with a lower risk of heart attacks and diabetes. The people with long-lasting symptoms showed higher levels of ‘bad cholesterol’ and unhealthy fatty acids.”Walgreens gets blamed, fast PTSD test, trusting YouTube videos, and more
Here we go again?
Walgreens loses in SF trial
Imagine you’re a tyrant

The next next antibiotic
Saliva test for PTSD
Captain Obvious says “Gesundheit”
Bad blood, long symptoms
August 11, 2022 ✒ Andrew Kantor
“Almost a Third of Patients Don’t Take Drugs as Directed” says a new study out of Canada, and if that many Canadians aren’t taking their meds, can you imagine what it’s like here? In a study that examined more than 200,000 patients and 91,000 unique prescriptions, overall nonadherence rates ranged from 13.7% for patients prescribed antidepressants to 30.3% for patients prescribed antihypertensive therapies. What’s the problem? It might be cost (Canadians’ healthcare is paid for by the government, but not prescriptions), but the researchers say that they just don’t know. “We assume that people are following our instructions. We’re often giving people second and third prescriptions before we even check if they’re taking their first one.” Get 20 hours of CE (!), the world’s best update on immunization skills, and a certificate to impress your patients — all from GPhA, starting August 21, with APhA’s Pharmacy-Based Immunization Delivery: A Certificate Program for Pharmacists. This ever-popular certificate training program prepares pharmacists with comprehensive knowledge, skills, and resources necessary to provide immunization services to patients across their lifespan — skills you need now more than ever. Sunday, August 21, 2022 8:00 am – 5:00 pm Georgia Pharmacy Association Classroom CLICK HERE for more information and to register! When a drug maker tests a drug, one thing it probably doesn’t consider is the patients’ posture. And yet (Johns Hopkins researchers realized), all those fluids churning around the stomach must have an effect. “When the pill reaches the stomach, the motion of the stomach walls and the flow of contents inside determine the rate at which it dissolves. The properties of the pill and the stomach contents also play a major role. So they built … StomachSim, a stomach-simulation computer program. (Sorry, “a biomimetic in-silico simulator based on the realistic anatomy and morphology of the stomach.”) Their goal is to use it to figure out how the position of the stomach might affect the absorption of medication — “unique insights into the complex physiological processes behind the oral administration of pills.” When it comes to improving how asthma patients use their inhalers, who do you think is a good choice? Why yes, as a matter of fact it is pharmacists. Granted, the folks at the Cleveland Clinic did more case studies than study-studies, but their conclusion sure makes sense. They tested the effect of having a pharmacist demonstrate and check inhaler technique before hospital discharge, then again at a follow-up visit. Result: Fewer errors and fewer problems. Fun facts: “exhalation before inhalation” was the most common error, followed by patients not holding their breath after inhalation. A new international study found that “a median of about 66,000 people are infected with [SARS-related coronaviruses] each year in Southeast Asia,” and that “suggests that bat-to-human SARSr-CoV spillover is common in the region, and is undetected by surveillance programs and clinical studies.” The good news: Many of those strains that infect humans “may not be able to replicate well in people, cause illness, or be transmitted sufficiently among people to cause an outbreak.” The bad news: “Many.” (Above link goes to the paper in Nature Communications. For the short news story, click here.) Giving fluoroquinolone to patients with chronic kidney disease increases their risk of an “adverse event” — and higher doses lead to higher chances. What kind of adverse event? We’re talking hospital visits for “nervous system and psychiatric disorders, hypoglycemia, or […] collagen-associated events.” The rate isn’t high, thankfully — around 0.9% on a low dose or 1.2% on a higher one, but still, that’s 1 out of 100 patients being hospitalized, and it’s not considering fluoroquinolone’s other possible side effects: aortopathy, arrhythmia, hyper- or hypoglycemia, neuropathy, or tendinopathy. This suggests, say the Canadian researchers who did the study, “that fluoroquinolones should be prescribed cautiously and at lower doses among older adults with advanced CKD.” British bioscientists say they’ve found a way to treat a cause of asthma, rather than just its symptoms, and it could lead to long-term treatments. The target: pericytes, stem cells in the lining of blood vessels. During an asthma attack, they move to the airway walls and then do what stem cells do — they turn into other cells. Like, for example, muscle cells, which tend to block the airways. What the Brits found is that 1) pericytes get the signal to move to the airways via a protein called CXCL12* and 2) a molecule called LIT-927 can block that signal. Asthmatic mice that were treated with LIT-927 had a reduction in symptoms within one week and their symptoms virtually disappeared within two weeks. The researchers also found that the airway walls in mice treated with LIT-927 were much thinner than those in untreated mice, closer to those of healthy controls. The usual mantra: “[F]urther research is needed before we can begin to test this in people,” including determining dosage, timing, what other effects LIT-927 might have, and what cool name they can give it. Combining drugs to treat osteoporosis (especially the postmenopausal kind) is often the best treatment. But which drugs? There’s no clear answer. Why not? Maybe because no one thought to ask the computer. Until a group of German researchers, that is. Using evidence of how bone is broken down and renewed, and how different kinds of osteoporosis medications work, they “built a mathematical model of bone renewal that predicts the effects of various osteoporosis medications in postmenopausal women.” They literally created an equation for osteoporosis: Then they tested it on various med combinations — and even the order those combinations were given. And that led to a surprising (and useful) finding: They […] found that combinations that cause the most rapid increases in bone density do not always strengthen bone in the long term and can instead cause a rebound of accelerated bone loss after the treatment stops. The end result wasn’t The Answer for the best meds combo for osteoporosis. The goal is to inform clinical trials that can confirm what the computer came up with, and hopefully design personalized treatment plans. Is prolonged skin-to-skin contact the only way it spreads? (Not exactly.) And how did the virus change to make this outbreak different? (It didn’t.) The details are in “What scientists know — and don’t know — about how monkeypox spreads” from Stat.Electronic stomach, lots more SARS infections, teaching to inhale, and more
I thought it would have been higher
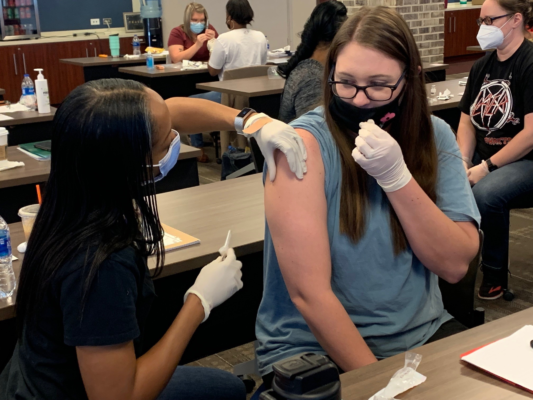
Pharmacists: Your hot immunization date is coming
SimStomach
Teaching technique
Something to look forward to in an upcoming season
Fluoroquinolone risks
Hitting asthma at its source
* Also a droid in the upcoming series, “Star Wars: Random Background Characters” on Disney+
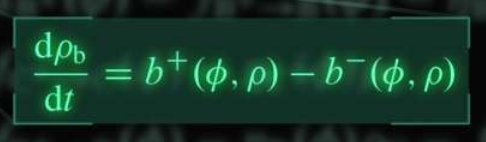
Drug combo equation
The Long Read: The Spread of Monkeypox edition
August 10, 2022 ✒ Andrew Kantor
On the latest list of “50 Highest Paying Medical Jobs in the U.S.” that is, just below prosthodontists and just above optometrists. (Topping the list are cardiologists and anesthesiologists, if you’re thinking of a second career.) Optum (the PBM) is going to be offering Sanofi’s insulin products at $35 a month for people who don’t have health insurance. All they have to do is go to the Optum Store (essentially the retail pharmacy), “get qualified,” and they’ll get a card allowing them to get Sanofi insulin for $35 at any retail pharmacy. Could Optum be doing this out of the goodness of its heart? Maybe. But then there’s this: “A mail service option will soon be available for people who prefer home delivery through the Optum Store.” We reported, you decide. So what exactly does the soon-to-pass Inflation Reduction Act mean for Medicare pricing and drug companies? The folks at the Kaiser Family Foundation have a handy chart. (It’s part of a deck of charts and info on the effects of the bill.) Remember, if you’re against allowing Medicare to negotiate drug costs, they’re price controls; if you’re in favor of the new rules, they’re spending controls. Something for everyone! That’s what an Argentinian research team found after studying long Covid and cognitive impairment in about 766 people, most of whom tested positive for Covid-19. The connection became clear. “All the subjects that had a severe cognitive impairment also had anosmia. We established an association between olfactory dysfunction and cognitive performance and impairment.” And their analysis showed which way the cause-effect went: “[S]everity of anosmia, but not clinical status, significantly predicted cognitive impairment.” Why this is the case, well, that’s not clear. Yet. At the moment, though, maybe you shouldn’t let someone make major life decisions if they’ve lost their sense of smell. The body uses a hormone called aldosterone to regulate salt and water (this is good). Too much of it, though, like any good thing, is a problem. For patients with chronic kidney disease, it can lead to kidney failure. It gets worse. The Boston University researchers who discovered this also found that “aldosterone plays a role in the progression not only of [chronic kidney disease] but also heart and blood vessel problems*.” [E]ach doubling of aldosterone concentrations in the blood was linked to an 11% increased risk of CKD progression. […] The risk was similar regardless of whether or not patients also had diabetes. The good news is that the existing kidney drug finerenone can counteract the overabundance of aldosterone and help prevent that kidney disease from getting worse. Good news! A combination of aspirin and an anti-platelet agent (e.g., ticagrelor) works a treat to prevent clotting after coronary artery bypass surgery. Bad news! A combination of aspirin and an anti-platelet agent (e.g., ticagrelor) “carries a significant risk of clinically important bleeding” after coronary artery bypass surgery. “So,” said the cardiothoracic surgeon and lead author of the study, “the benefit comes at a price.” The advice: “Physicians should base their decisions on patients’ individual circumstances.” Charlotte’s Web could’ve had a very different ending. (Psst: Soviets did it.) Pfizer is getting ready to start phase-3 trials of the Lyme disease vaccine it bought from Valneva (soon to be called the “Pfizer vaccine,” of course). Millions of hikers and lawn-mowers across the country await the results. They tested both two- and three-dose regimens and found that three doses works better — that’s what they’ll be testing now. (Doses two and three are given two months and six months after the first, in case you’re interested.) Obligatory: There was once a Lyme vaccine (Lymerix), but thanks to a combination of anti-vaxxers, hypothetical side effects, price, and a bit of sensationalism, it was pulled from the market in 2001. The retailer got itself a strongly worded letter because some third-party sellers — whose products were fulfilled by Amazon — were selling mole-removal products. And that’s a no-no. “There are no over-the-counter (OTC) drugs that can be legally sold for mole or skin tag removal,” the agency said, wagging a metaphorical finger. Despite the letter, at press time a GPhA Buzz investigation* found you could still buy the stuff: “Eating grapes could hold remarkable potential for health benefits” … according to a study funded by the California Table Grape Commission.When long Covid means dementia, clot-busting dangers, zombie pigs, and more
Pharmacists are #25
PBM to provide $35 insulin
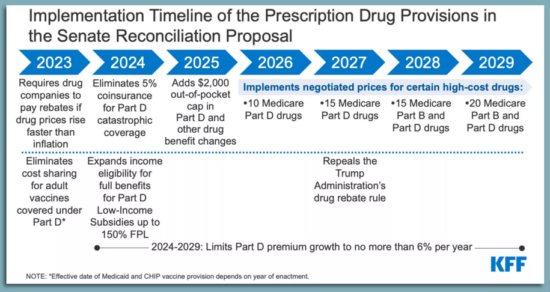
Medicare changes in a chart
Stop. Can you smell the roses?
The kidney disease hormone
* Because aldosterone activates the mineralocorticoid receptor, which can lead to high blood pressure, among other issues. But you knew that.
Should you call the clotbusters?
ICYMI: Some (zombie) pig
Lyme vax almost ready for prime time
FDA slaps Amazon
* I searched on “mole removal” on Amazon
It annoys me that these stories get press coverage without a disclaimer
August 09, 2022 ✒ Andrew Kantor
Current wisdom: Insulin resistance (through unknown-as-yet mechanisms) causes changes in the endothelial cells lining blood vessels, and that leads to fat buildup and cardiovascular disease. But what if that’s (as the headline says) backwards? That’s what researchers at Boston’s Joslin Diabetes Center are suggesting. Their finding: That it’s the endothelial cells in control and driving metabolism, rather than being on the receiving end. In a reversal of scientific dogma, the findings suggest that vascular dysfunction may itself be the cause of undesirable metabolic changes that can lead to diabetes, not an effect as previously thought. And then, to complicate matters, there’s a sort of feedback-ish loop in effect. Problems with the endothelial cells lead to insulin resistance (they found). That’s problem one. Problem two: Insulin is also what comes back to those same endothelial cells and causes them to produce nitrous oxide. Nitrous oxide triggers the production of brown fat cells — the good fat. So … 1) problems in blood vessels lead to 2) insulin resistance, then insulin resistance 3) means those blood vessels produce less nitrous oxide and 3) that means less calorie-burning brown fat. Or, as the chief researcher put it, “Everything is connected.” With demand for the Jyenneos smallpox vaccine skyrocketing, the FDA is considering allowing one dose to be split into fifths, quintupling the supply. How can that work? By giving it intradermally instead of subcutaneously. “There’s some advantages to intradermal administration, including an improved immune response to the vaccine,” [FDA commish Robert] Califf said. “It’s important to note that overall safety and efficacy profile will not be sacrificed with this approach.” The American Society of Health System Pharmacists is asking HHS to allow pharmacists to deliver the smallpox/monkeypox vaccine (via a PREP Act declaration, like with Covid vaccines) to make it easier for people to get it. You know the reasons; no word from HHS yet. If you’re a gang member or mob boss, scars are good. If you’re trying to pump insulin, no so much. The problem: Implantable insulin pumps are a great idea, but the immune system will attack them, form scar tissue around them, and eventually clog the pump. MIT engineers came up with an unusual solution: They surrounded the pump with a balloon that could be inflated and deflated. It doesn’t need to be often, either — just every 12 hours, in testing, was enough to drive away the immune cells that lead to scar tissue formation, like trying to paint a balloon that inflates before the paint can dry. And while scar tissue did form eventually — you can only fool Mother Nature so long — the collagen fibers were aligned, which (they believe) allowed the meds to get through anyway. It’s been tested on mice and cadavers, so (live) human tests are next. The big news this weekend was the passage of the Inflation Reduction Act of 2022. Despite the headlines, there were actually wins on both sides of the aisle when it comes to the pharma-related portion of the bill. For Democrats, CMS will finally be able negotiate drug prices like the rest of the world … on 10 older drugs that don’t yet have a generic version. That’s all. (The bigger deal is that it’s a foot in the door of drug-price negotiation.) But Republicans got wins too, although they’re being overshadowed by the press around the price-negotiation news. The GOP prevailed by preventing the imposition of a $35 out-of-pocket cap on insulin on private insurance plans, as well as in other, non-pharma parts of the bill (e.g., there will be no requirements for paid family leave, nor funding for universal preschool or an expansion of the child tax credit). As for price negotiations, despite one side saying it will mean unicorns and rainbows and the other predicting angry dragons and rains of despair, chances are the effects will be, like the weather, partly cloudy or partly sunny. Cats predicting death. Dogs detecting Covid. They are sooooo last year. Now we have the world premiere of “Locusts Detecting Cancer.” Locusts, it seems, can distinguish between cancer cells and normal cells and even distinguish different kinds of cancer. And as tempting as it may be to send swarms of locusts through doctors’ offices*, the reality is boring: “[T]his work could provide the basis for devices that use insect sensory neurons to enable the early detection of cancer using only a patient’s breath.” This’ll be a Big Deal soon enough: In an effort to get their hit of nicotine, teens are turning to gum, lozenges, and gummies, often flavored just for them (mmm, “fruit medley”!). They contain plenty of drug, are easier to hide in school than vapes, are entirely unregulated, and are now second in popularltiy only to e-cigarettes , according to research out of USC. It’s almost as if companies want to hook them on an addictive drug while they’re in middle school. Latest on the list of “what can vitamin D do for you” is … reduce inflammation. Maybe. The whole cause/effect thing isn’t entirely clear. When you’ve got chronic inflammation, the liver produces more C-reactive protein. But (say Aussie researchers), if you take vitamin D, the levels of that protein go down. Their conclusion: “[T]he findings suggest that boosting vitamin D in people with a deficiency may reduce chronic inflammation.” But note the weasel words “suggest” and “may.” That’s because there’s a black box in operation here. Does vitamin D affect the inflammation, or could it be affecting the protein? Or maybe it’s backwards — low C-reactive protein means lower vitamin D? Right now there seems to be a connection, but more work is needed to figure out just what it is. A problem with many vaccines is that they don’t last long once they warm up. That’s why the whole cold chain thing is such a big issue. The result, say Swiss researchers, is that half of vaccines go to waste. So, being Swiss, they came up with an elegant solution. It’s a hydrogel — “a biocompatible, synthetic polymer known as ‘PEG’ that serves as a protective, ‘cloaking device’” for large molecules like vaccine proteins. So instead of wrapping the vial in a blanket of cold that has to be maintained, the Swiss wrap the individual molecules in the polymer, which can keep the proteins safe up to about 150°F. And to remove the coating? Just dissolve it with a sugar solution. It’s still in the lab phase (i.e., “more research is needed”) but the Swiss Federal Institute of Technology is already flinging around Buzz’s favorite phrase: “game changer.”What the locusts smell, splitting the pox vax, hot nicotine candy, and more
Could we have the diabetes/heart disease connection backwards?
Monkeypox vaccine update
Five-for-one split
What about you?
Pump it up (the implant, that is)
Everybody wins … sort of
A useful plague of locusts
* Especially during Passover
Next in nicotine
Can D do this too?
Making vaccines last
August 06, 2022 ✒ Andrew Kantor
Here’s a weird one: People who have a high level of the protein prostasin in their blood are significantly more likely to have diabetes. Why? The Swedish and Chinese researchers who discovered the connection aren’t sure. Is it somehow helping cause the diabetes? Is it a marker for a different cause? Regardless, “those with the highest levels of prostasin […] were almost twice as likely to have diabetes than those with the lowest levels.” But wait, there’s more. Those who also had a high level of blood sugar (perhaps the were already diabetic) were at much higher risk of dying from cancer. For every doubling in prostasin concentration, the risk of cancer death rose by 24% in those without high blood sugar, and by 139% in those with high blood sugar. The diabetes-cancer connection was already known, but this might give insight into the mechanism. And it certainly makes for a blood test to pay attention to. Wondering which animals around the world have been infected with Covid-19? There’s now an interactive dashboard for that. As adding fentanyl to street drugs becomes passé, the latest deadly additive is … xylazine. Yeah, the animal tranquilizer is showing up (ironically) as an additive to fentanyl and cocaine. It started being reported in Puerto Rico, Philly, and now Massachusetts (in anywhere from 28 to 90% of the drugs tested — but we all know it won’t be long before it’s everywhere. The danger is not that someone might OD on xylazine, but that, as a sedative, it will make an opioid overdose worse by slowing the heart. There’s a lot of speculation about how and why xylazine is on the rise. It may be added to fentanyl or heroin to help extend the effects of an opioid high. Dealers also may be using this relatively inexpensive and easy-to-order sedative because of supply chain gaps with other drugs. Oh, yeah, and it’s not easily detectable with a test strip (like fentanyl) nor affected by naloxone. Moderna says it’s considering turning its mRNA-vaccine muscle toward making monkeypox vaccines. It depends, of course, on whether cases continue to rise and spread and, presumably whether those deep government pockets will be where the payment comes from. “Our platform is pretty well established and our ability to rapidly scale has been demonstrated. If we were to go after a monkeypox clinical development program, it would be to very quickly progress toward an approvable set of endpoints in a clinical study.” But can the mRNA tech handle that large monkeypox viral protein? Perhaps we’ll find out. People who have an opioid-abuse problem aren’t getting the meds they need to quit. In fact, say NYU researchers, “Almost 90 Percent of People with Opioid Use Disorder [are] Not Receiving Lifesaving Medication.” Part of the problem is obvious: More than 70% of residential treatment programs don’t offer methadone, buprenorphine, or extended-release naltrexone — drugs that can cut (or potentially eliminate) half or more of overdoses while helping people quit. “We need to rethink how treatment for opioid use disorder is delivered, eliminate stigma, make it easier for people to enter and remain in treatment, as well as ensure that all treatment programs provide and encourage use of evidence-based medications that we know save lives.” The most reliable info to date on long Covid: 1 in 8 people infected end up with it. That’s based on a Dutch study of more than 76,000 people and 23 symptoms that are officially (or semi-officially) associated with persistent symptoms. What makes this study different is that the Dutchies took into account that some of these symptoms existed before Covid infection, so they can’t really be attributed to long Covid. (“Symptoms such as fatigue and headaches might be worsened during the pandemic also in people without Covid-19, for example.”) There are lots of ways to try to tackle the issue of antibiotic resistance including phages (see below) and augmenting or repurposing old drugs. But Aussie researchers have an new idea: proteins. Specifically, they’re looking at guanylate-binding proteins, which the human immune system uses as one of its weapons to kill bacteria. By themselves or combined with antibiotics, GBPs could be — after much more research of course — another new weapon. Resistance may eventually be futile after all. “We are now finding more and more GBPs that can kill different types of drug-resistant bacteria. This includes bacteria that can cause meningitis, pneumonia and sepsis. […] The ultimate goal is to use these proteins to eliminate meningitis, pneumonia and sepsis entirely.” Bacteriophages — bacteria-killing viruses — are one of the most promising tools against drug-resistant germs. But once you introduce them to kill the bacteria, you start an arms race between the good viruses and the bad bacteria. Israeli and German microbiome researchers have a possible solution, and it almost seems obvious: One phage good? More phages better! Looking to fight gut inflammation, they’re “using a cocktail of phages that use multiple lines of attack against Klebsiella pneumonia bacteria, preventing them from evolving resistance to the mixture.” And because phages target a single bacteria (unlike broad-spectrum antibiotics) this cocktail doesn’t affect anything else in the gut. The downside? Phages have to be found, and it took them five years (“a a painstaking fishing expedition”) to isolate phages that attack K. pneumonia. Congress is set to pass the “Inflation Reduction Act” which would allow Medicare to negotiate the prices of [insert drumroll] a whopping 10 drugs … in 2026. That would go up to a staggering* 20 drugs by 2029. (For comparison, the rest of the world can negotiate the prices of every drug.) The pharmaceutical industry is against the bill, of course, threatening to stop trying so hard to develop new drugs if their executives and shareholders face lower paychecks.Move over, fentanyl; 12.5% long Covid; a flag for diabetes, and more
A marker for diabetes (and cancer)
What else has Covid?

After fentanyl
mRNA for monkeypox
The addiction drugs they can’t get
Quickie Covid data
Killing bacteria
A new kind of germ killer
You can’t fight the phage cocktail
A tiny change to drug pricing looms
* This is sarcasm.
August 05, 2022 ✒ Andrew Kantor
It’s 3:00 am and you’re not in a Denny’s mood. How about getting a Covid test instead? Good news: The Georgia Department of Public Health has opened a bunch* of 24/7 kiosks throughout the state offering free tests. (Here’s the map.) Fill out the quick form and the kiosk dispenses a kit. Swab, dip, etc., and put it back in the kiosk. The next day it’ll be picked up and given a super-accurate PCR test — you’ll be notified of the results by email or text. Pharmacists, do you have enough continuing ed under your belt to renew your license? If not, no worries — GPhA has ways of Gives you 23.0 hours of CPE (in person plus home study)! In-person sessions: Sunday, August 21 —or— Sunday, December 11 (8:00 am – 5:00 pm) in GPhA’s Sandy Springs classroom Click here for details and to register. Gives you 21.0 hours of CPE (in person plus home study)! Live via Zoom; Sunday, September 18 (8:00 am – 5:00 pm) Click here for details and to register. Gives you 20.0 hours of CPE (in person plus home study)! In-person session: Sunday, October 2 (8:30 am – 12:30 pm) in the GPhA Sandy Springs classroom Click here for details and to register. A big GPhA Buzz shout-out to GPhA member Al Dixon of Richmond Hill Pharmacy in Bryan County, who was featured in a WSB-TV story on rising drug prices. Specifically, it was based on AARP of Georgia s reminding everyone that drug prices have risen “73% in the last seven years, hurting Georgia’s seniors.” And who’s to blame? PBMs. (Yeah, the article misspelled his name. Over and over. ) The CDC is expected to update it’s don’t-get-Covid guidelines in the next few days “to ease quarantine recommendations for people exposed to the virus and de-emphasize 6 feet of social distancing.” It’s also going to “de-emphasize regular screening testing for Covid-19 in schools” and stick with its test-to-stay strategy. All this, of course, assumes that there won’t be a major surge when students return to school and an unexpected definition of “cultural studies.” It’s now officially a public health emergency in the US. That just means more hyperactive news stories … and more importantly, “Federal health officials can now expedite preventative measures to treat monkeypox” and have some more flexibility in how they do it. Luckily, it’s rarely fatal (but very uncomfortable) and only spread through intimate skin-to-skin contact. There’s a monkeypox vaccine (although it can be hard to get), but what about treatments? One that’s out there is TPOXX (aka tecovirimat) which is approved to treat monkeypox’s nasty cousin, smallpox. And while TPOXX has been tested for monkeypox on animals, it’s still officially an investigational drug when it comes to humans. So if you want to use it here in the US of A, that means paperwork. Lots of paperwork. Will that change now that this is an emergency? Should it? Read on. The Brits have identified new symptoms of the disease. Upon reading the headline, I thought to share those new symptoms with you. Upon reading the article, however, I prefer to simply provide the link. For those of you who clicked and read, here’s a picture of a bunny and a kitten: Some moles don’t know their place. Rather than sit still and maybe be the subject of an awkward glance, they start to grow until they become melanoma, the really bad skin cancer. Why do some have to be that way? Who hurt them? Who did this to them? Boston University researchers think they know. If they’re right, it could open the door to treatments not only for melanoma (and pre-melanoma) but potentially other types of cancer. It’s all about the Hippo tumor suppressor pathway which, to oversimplify, tells cells when to stop growing. When the Hippo tumor suppressor pathway is itself suppressed, “those cells rapidly go on to form melanoma in multiple experimental models.” Keep it working properly, and moles stay moles. Next up, as always, more research. CVS announced that it’s joining Amazon, Walgreens, and that group of hobos under the bridge and getting into the primary care business. The company wants to offer longer hours at its doctor [sic] offices so people can visit as early as 6 a.m., as late as 9 p.m., or on the weekends. Completely unrelated, America’s physician shortage continues to the point that Time magazine is offering solutions. Also unrelated, a new study out of the University of Chicago found that “It would take a primary care physician 26.7 hours per day to follow national recommendation guidelines for preventative, chronic disease and acute care for an average number of patients.” The Brits are simply not satisfied with how well bleach works to kill germs. It’s just too slow. A northern-England hospital had an idea: a disinfectant based on hypochlorous acid, a natural compound that also comes from chlorine and is used in the U.S. as a disinfectant. They call their product Pathisol, and researchers at Teesside University (home of Barry the Beaver) are testing it in a clinical environment for the first time, misting entire wards with the stuff. The benefit, if it pans out: “Pathisol can disinfect a surface in two minutes, which is five times faster than bleach. It can also kill 99.99% of pathogens, including hospital superbug Clostridium difficile.” It’s also cheaper to make than bleach and more environmentally friendly — and you get to apply with a cool spray gun.CDC relaxes (for now), CVS has big plans, Georgia gets Covid-testing kiosks, and more
Covid kiosks
* We didn’t bother to count.
It’s a license renewal year
making you talk helping you meet your requirements tout de suite, and get some spiffy certificates for your wall while you’re at it.APhA’s Pharmacy-Based Immunization Delivery Certificate Training Program
APhA’s Delivering Medication Therapy Management Services Certificate Training Program
NASPA’s Pharmacy-based Point-of-Care Testing Certificate Program
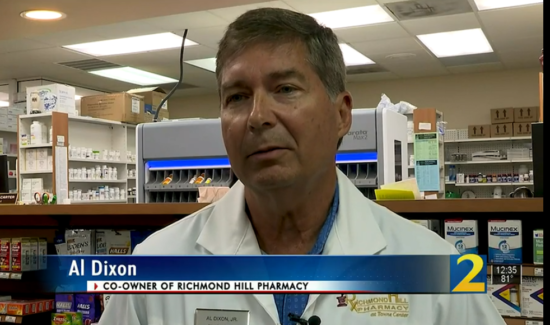
You can call him Al
CDC say relax
Monkeypox updates
Urgent, urgent, emergency
Whither TPOXX?
Eeew

When moles go bad
CVS on the bandwagon, but who’ll drive it?
Disinfecting: Better, stronger, faster

August 04, 2022 ✒ Andrew Kantor
As the school year starts, an Adderall shortage is the last thing we need, and yet here we are. Both 20-mg and 30-mg tablets of Teva’s branded ADHD drug Adderall are currently on back order in the U.S., with the company eyeing a release date in early- to mid-August. Teva not only makes Adderall, it also makes most generic amphetamine salts, but the company says not to worry, “[We] expect full recovery for all inventory and orders in the coming weeks.” It’s almost time to render unto Mary that which is Mary’s. (Meaning Mary Ritchie, GPhA’s director of membership.) Your GPhA 2022–23 dues invoice will be coming to your mailbox soon, so keep an eye out. And please, if you would be so kind as to send it back quickly, it’ll make Mary’s life a bit easier. Thank you! Would you like your pharmacy to appear in on a reality show called “Show Me” — if we promised that it would not require compromising your virtue? If so, NCPA is looking for you. Think of it like “Kitchen Nightmares” or “Bar Rescue” but with less cursing and alcohol, and more lab coats and plastic bottles. “Show Me” will feature “NCPA members facing typical pharmacy challenges who get the help they need from some peers who’ve been there and done that.” You and your pharmacy could be on it — you just need to apply with a video to prove you’ve got what it takes for your close up. Click here for the details, some tips, and the submission form. Being cold, it seems, inhibits cancer growth. That’s what Swedish researchers discovered, and the mechanism is actually quite simple: [C]hilly temperatures activate heat-producing brown fat that consumes the sugars the tumors need to thrive. Similar metabolic mechanisms were found in a cancer patient exposed to a lowered room temperature. They even did some preliminary human testing and found that being at about 60°F vs. 82°F makes a difference — “The imaging scans picked up increased brown fat and lowered tumor glucose uptake during the lower versus the higher temperature.” Yesterday, the hospital-owned nonprofit Civica Rx launched CivicaScript, and it began selling it’s first drug, abiraterone, for a lot less that the list price. A month’s supply of abiraterone 250 mg will be sold to pharmacies for about $160 a bottle with a maximum retail price of $171 — about $3,000 less than the average price for someone with Medicare Part D coverage. More interesting for those with crystal balls is that CivicaScript is part of a larger trend of non-profits arising to take on the pharmaceutical companies — and high drug prices — by offering cheaper generics and price transparency. Separate studies out of Israel, the US, and Japan all conclude — to one degree or another — that three (or preferably four) doses of an mRNA vaccine protects people from Omicron. Not perfectly, but it reduces the risk of symptoms and hospitalization enough to say, “It’s effective.” This wouldn’t be the Covid pandemic if there wasn’t one snag after another. Today’s (well, yesterday’s) hiccup: Although the EU, like the US, has approved Novavax’s Covid-19 vaccine as an alternative to the two mRNA shots out there, the European Medicines Agency now wants that vaccine to carry a warning that both myocarditis and pericarditis are potential side effects, in addition to the existing “severe allergic reactions.” Eating a bit of Jarlsberg cheese — and only Jarlsberg cheese — “may help to stave off bone thinning,” according to a study out of the Norwegian University of Life Sciences. But before you rush out to the dairy section, note that the study was funded by Tine, “Norway’s largest producer, distributor and exporter of dairy products.” (Oh, and if you’re thinking, “I‘d rather have Camembert than Jarlsberg,” I have bad news for you.) Side reading: Experts call into question some significant limitations of the study. Chillin’ the cancer, Adderall shortage, grain-of-salt cheese news, and more
Potential slow start to the school year
Dues renewal is nigh!
If you show me yours…
Good news for Walt Disney
The Short Read: CivicaScript Debuts edition
Latest Covid vaccine news
Three studies, one variant family
Novavax warning
Bring cheeses into your life?
August 03, 2022 ✒ Andrew Kantor
Here’s a surprising bit of news: There are apparently a bunch of online pharmacies — “rogue” pharmacies, mind you — selling chemotherapy drugs like imatinib without proper prescriptions. The research (by UNC School of Pharmacy researchers) was straightforward: They simply searched online for where to buy chemo meds to get an idea of the scope of the problem. “By simply searching Google, Bing, Yahoo, and DuckDuckGo, we found 44 websites that sold and shipped imatinib in the U.S.; 13 of these websites sold imatinib without a prescription, and more than three-quarters did not offer a way for patients to speak with a pharmacist. This is a significant concern for patient safety.” And that’s based on just the first 10 pages of search results. (Fun fact: You can actually look past the first page of results. Who knew?) They didn’t actually buy any of these drugs, but they point out that … well, let’s just say that quality control might be lacking, although the prices were often significantly lower than patients would normally pay — the very reason these sites exist. Columbia University researchers have created a database of nearly 20,000 potential pediatric adverse drug events (ADEs) — interactions that can occur at all stages of development, many of which haven’t been reported yet. That last part is the gem: Existing databases, such as the FDA Adverse Event Reporting System, “only capture data from patients who experienced adverse events,” while the Columbia database uses computer modeling to identify issues before they occur. The database, which is made freely available (via a site called PDS Portal), isn’t meant for clinical use; it’s designed for drug researchers, although “Clinicians can use it as a gut check.” Banana Boat is recalling some batches of its Hair & Scalp Sunscreen because it may contain benzene, which you don’t want anywhere near you. It’s only three lots, and it doesn’t (yet) affect any other Banana Boat products. Get the deets from the official FDA recall page. Two types of meds — beta blockers and antiplatelet drugs (including aspirin) — increase your risk of heart attacks in hot weather. Somehow (the Yale researchers who discovered this don’t know how) they make the heart more susceptible when the weather gets warmer. Antiplatelet medication use was associated with a 63% increase in risk and beta-blockers with a 65% increase [in heart attacks]. People taking both drugs had a 75% higher risk. Non-users of those medications were not more likely to have a heart attack on hot days. To get even more complicated, statins tripled the risk of heart attack for younger people on hot days, but didn’t have that effect on older patients. If you’ve had a kidney stone, there’s a good chance you never want another. The folks at the Mayo Clinic have some advice: Make sure you’re getting enough calcium and potassium. Their new study looked not at preventing first time kidney stones, but at stopping recurrence. Some of their findings aren’t surprising, such as “drink more fluids.” But the surprise was that “Low dietary calcium and potassium was a more important predictor than fluid intake of recurrent kidney stone formation.” The study concludes that diets with daily intake of 1,200 milligrams of calcium may help prevent first-time and recurrent kidney stones. [It didn’t have a specific recommendation for potassium, so take your best guess.] As the legalization of marijuana spreads, so too do the number of studies on the stuff — including some with eyebrow-raising conclusions. (Not, like, shocking. Just unexpected.) For example, smoking marijuana might reduce incidence of sinus problems like congestion, sneezing, and sinus pain … at least according to a study from USC’s Keck School of Medicine. The study of nearly 2,300 U.S. adults found that while cigarette smokers were often plagued by such symptoms, the same did not hold true for regular marijuana users. Actually, they don’t know which way the causation goes, so it’s possible “people who already have nasal or sinus symptoms might steer clear of marijuana.” The mantra, as always: “The only way to find out […] is with further research.” Why does eating too much red meat increases the risk of heart problems? We know it does, but what’s the mechanism? A surprising (possible) answer comes out of Tufts University: It’s the gut bacteria. “Chemicals produced in the digestive tract by gut microbes after eating red meat may help explain part of the higher risk of cardiovascular disease associated with red meat consumption.” Not that cholesterol and salt are helping, but gut bacteria produces trimethylamine N-oxide (TMAO) when it digests red meat, and high levels of TMAO are double-plus ungood for people, with links to cardiovascular issues, kidney disease, and diabetes. In other words, by eating red meat you’re feeding bacteria that, er, expels poison into your gut. A lot of hospitals have “smart” IV infusers that can automatically calculate the correct dose and rate for delivering drugs, but — at least in Britain — many aren’t used “because they are difficult to configure and maintain.” So instead of a pump that’s configured by a pharmacist and smart enough to sound an alarm if something’s amiss, you have a dumb pump “set by ward staff who calculate and input infusion rates themselves — increasing the risk of drug errors.” That’s what researchers from Manchester, England, England* found based on data from the UK’s National Health Service; they calculated that “1 in 10 IV drug administrations are associated with an error, and up to 1 in 10 of those were associated with harm.” Heart meds hate heat, red meat secret revealed, cancer-drug shenanigans, and more
Rogue chemo drugs
Big new drug-interaction database
ICYMI: Banananana Boat recall
Heat, meds, and heart attacks
Stopping stones: Water good, calcium better
What cannabis can do (entry 261)
Why is red meat bad?
Smart IVs, safe patients
* Across the Atlantic sea
August 02, 2022 ✒ Andrew Kantor
Diabetics taking higher doses of insulin have a higher rate of cancer, especially if they’re insulin-resistant. Yeah, read that again. The findings, out of Ohio University, are based on health records of 1,300 patients over 28 years, so the increase can take a long time to appear. (And the it’s further muddied by the idea that having diabetes itself might raise the risk of cancer.) Of note is that insulin-resistance. The epidemiologists who ran the study suggest that, to mitigate cancer risk, “improving insulin sensitivity may be preferred than simply increasing the insulin dose.” Is it time to renew your workers’ compensation or business liability insurance? Talk to Hutton Madden first: (404) 375-7209 or hutton.madden@phmic.com. The U.S. hit a new low for the number of uninsured people — only about 8 percent of Americans are now without some kind of medical coverage according to the latest CDC data (PDF). This is the lowest level in … well, in the modern, employee-based-healthcare era. The bad news: A lot of people will be unable to afford coverage when this calendar year ends, because that will also end pandemic-related measures to help people pay for insurance. The good news is that Congress might vote to keep them in place, along with support for people in states that haven’t yet expanded Medicaid coverage. For quite a while (i.e., more than 50 years), Asians and Eastern Europeans have been using cytisine as drug to help quit smoking; it’s a partial agonist against nicotinic acetylcholine receptors*, like Chantix (aka varenicline), but it’s “natural” in the sense that it’s a plant alkaloid. Canada only just approved it a few years ago, but in most of the Western world it’s eclipsed by Chantix — in fact, my spell-checker recognizes varenicline but not cytisine. Why is that? For one, previous studies found that while cytisine is better than placebo, it’s not quite as good as varenicline. For two, varenicline makes some companies a lot of money. But varenicline has issues (suicidal behavior, anyone?) so in 2018 the FDA approved a study of cytisine on our freedom-blessed shores. So, does it work? The result is an rock-solid, unequivocal “It seems to, yeah”: “At the 12-month follow-up, the quit rate was 32.1% in the intervention arm and 7.3% in the control arm.” One interesting note: The researchers who conducted the previous study suggest that “populations more accepting of ‘natural’ products would respond better to cytisine than to varenicline.” It’s just three weeks away — GPhA’s Immunization Delivery Training for Pharmacy Technicians! In half a day — 3 hours at home, 3 hours in the classroom — you’ll score yourself 6.0 hours of CE, and be able to tell your boss that you are 100% ready to give immunizations. With the coming Covid surge, monkeypox, and whatever else is on the schedule, you want to be ready. And GPhA will make sure you are. Sign up now for the live training on Saturday, August 20 in Sandy Springs. Space is limited, so don’t wait! Click here for all the details and to register! If you have a roundworm (C. elegans) that you want to live forever, what’s the trick? One way: Improve its mitophagy — the mechanism for replacing worn-out mitochondria*. That mechanism, though, wears out with age, leading to a lot of dead mitochondria lying about, and thus unhealthy cells. But now Israeli researchers say they’ve found a way to keep the mitophagy going strong, using molecules they created (“distinct designer diamines”) that … … promote mitophagy, and thereby enhance healthspan in C. elegans and protect human cells against oxidative damage. Naturally, they’ve already formed a company to try to turn the discovery into an actual drug. Eventually. Could it be a “one-two punch” from the varicella zoster virus (VZV) ‘waking up’ the herpes simplex virus (HSV-1)? Both viruses were known to maybe kinda sorta have a connection with Alzheimer’s, but now a collaboration between researchers at Oxford and Tufts universities found that individually they aren’t a danger but … … exposing brain cells harboring dormant HSV-1 to VZV led to a reactivation of the herpesvirus and a cascade of the toxic plaques known to be signs of Alzheimer’s. The fact that VZV can reactivate the herpes virus doesn’t mean that other viruses can’t do the same. The critical bit of info, they feel, is that reactivating dormant HSV-1 might be a trigger for Alzheimer’s disease, and that needs to be explored. Not many drugs have gone from prescription to over-the-counter lately, and here’s an interesting reason: The U.S. doesn’t have much of an “behind-the-counter” alternative, where customers must ask for a medication and (in theory) get advice or consultation with a pharmacist. That might be changing, as the FDA considers a new rule called “Additional Condition for Nonprescription Use.” (Then again, the idea has been around for at least a decade, so don’t hold your breath.) If the rule is approved, though, it could open the gateway to a lot more no-prescription-needed drugs, giving the FDA a way to split the difference when it comes to meds that seem almost safe enough to be on the rack, but not quite. The answer will keep changing as new studies come out, but the latest — courtesy of the American Heart Association, and based on “An analysis of physical activity and medical records for more than 100,000 people over 30 years” — says the answer is [insert drumroll here] … … at least 300 minutes of moderate physical activity per week, or 150 minutes of vigorous activity. “What?” you say, “That’s not what the headline reads.” True — the headline is the current guideline. What the story says is that there’s an increased benefit for doing two to four times that. The reduction [in mortality] was 21-23% for people who engaged in two to four times the recommended amount of vigorous physical activity, and 26-31% for people who engaged in two to four times the recommended amount of moderate physical activity each week.Immortal Israeli roundworms, OTC alternative, insulin’s cancer risk, and more
Unexpected insulin danger
Hutton is waiting
U.S. hits a positive milestone
A different anti-smoking tool?
* I think I got that grammar right.
Techs: Get that immunization training!
Did Israelis find the key to immortality?
* All together now: “The powerhouse of the cell.”
Today’s potential Alzheimer’s cause
Between the rack and your counter space
What’s the right amount of exercise to live longest?
July 30, 2022 ✒ Andrew Kantor
Post-menopausal women dealing with osteoporosis can take teriparatide — but there’s an important note. The synthetic hormone will restore their bones’ mineral quality, but it has to be taken for 24 months — not fewer. “[T]he full benefits of teriparatide treatment on forming bone quality are realized only with a full-course treatment,” said the leader of the Austrian team whose study figured this out. And there’s good news: After two years, the women’s bone quality was “similar to that of healthy premenopausal women.” Congrats to the team from the UGA College of Pharmacy, who — along with the University of Arkansas for Medical Sciences (last year’s winner) and University of South Carolina (don’t call it “USC”) — are finalists for NCPA’s 2022 Student Business Plan Competition. It’s not clear what the next step is, but whatever it is, we’re pulling for the Dawgs! The winners will receive two cash prizes (amount unknown) — one for the team’s NCPA student chapter, and one for the team’s school to promote independent pharmacy. More importantly, they get a year of bragging rights. So here’s where we stand with Covid booster shots for the fall: The FDA said that people under 50 won’t need a booster yet — it’s saying wait till the fall when Omicron-specific boosters are available. To make sure they are available, the U.S. has arranged for 66 million doses of an updated version of Moderna’s vaccine. Combined with 105 million doses the government already agreed to buy from Pfizer […] the latest deal puts the U.S. booster dose supply at about 171 million shots. Transparent face shields are popular among the more cautious people when in a potential Covid-catching situation. They add an extra layer of protection without interfering with breathing or speaking. Well, bad news. Turns out most of them don’t do much after all. British researchers put them to the test using a “coughing machine” (really) that spewed out dyed droplets onto shielded mannequin heads. Result: “The lab tests showed that all of the face shields provided some protection, but none gave high levels of protection against external droplet contamination.” That’s because there were gaps, and people turn their heads (and droplets get caught in air movement). You need a pretty big shield — “closed across the forehead and extended well around the sides of the face and below the chin” — to be effective. That’s the headline I would use if I was running a tabloid. The reality is that “Eating More Ultra-processed Foods [is] Associated with Increased Risk of Dementia,” and ketchup happens to be one that’s mentioned. Ultra-processed foods are high in added sugar, fat and salt, and low in protein and fiber. They include soft drinks, salty and sugary snacks, ice cream, sausage, deep-fried chicken, yogurt, canned baked beans and tomatoes, ketchup, mayonnaise, packaged guacamole and hummus, packaged breads and flavored cereals. (Note that the article’s definition of “ultra-processed food” doesn’t quite jibe with the typicaldefinition. Add salt to peanuts and they’re “processed”; to be “ultra-processed” they need to have several additives, and possibly colors and flavors, too.) There have been three waves of opioid deaths over the past two decades — that’s the “opioid crisis.” We’re entering a fourth wave now, say researchers at Northwestern, and it’s going to be a bad one. The first three waves were caused by (in large part) opioid pills, heroin, and fentanyl, respectively. The fourth wave is fueled by “combining synthetic opioids with stimulants such as cocaine and methamphetamines.” “This is a bigger problem because you have people misusing cocaine and methamphetamines along with an opioid, so you have to treat two things at once, and the fentanyl is horribly volatile.” First: “Peanuts Help Weight Loss, Blood Pressure, Glucose Levels” (funded by the Peanut Institute of Albany, Georgia). Second: “Daily Avocados Intake Improves Diet Quality, Lowers Cholesterol Levels” (funded by the Avocado Nutrition Center). A study out of Rush University found that strawberries — actually, a compounded they contain called pelargonidin — might reduce the risk of Alzheimer’s by reducing the “neurofibrillary tau tangles” in the brain: “The data suggests that pelargonidin may protect the aging brain from developing Alzheimer’s disease pathology.” “We suspect the anti-inflammatory properties of pelargonidin may decrease overall neuroinflammation, which may reduce cytokine production.” Notice all the “mays” and “mights”? Yeah, this is a bit preliminary. The big question here at Buzz HQ: Who funded the study? It would cost €27.50 to find out, which is €27.50 more than our budget for scientific papers. Results of a survey released by the American Medical Association found there’s a small percentage of Americans with very interesting views about their healthcare data. Face shield failure, the next opioid wave, strawberries vs Alzheimer’s, and more
Teriparatide: All you need is just a little patience
UGA’s plan enters competition finals
* Technically the Good Neighbor Pharmacy NCPA Pruitt-Schutte Student Business Plan Competition (GNPNPSSBPC)
Fall booster plans
Shields up! (or not)
This’ll work — flower not required
Ketchup can lead to dementia
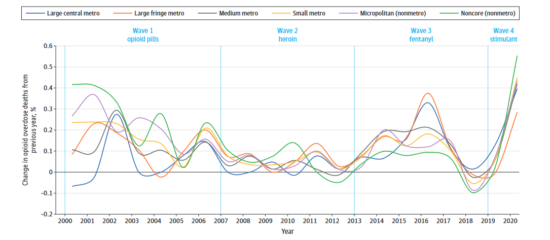
I see trouble on the way
Nutrition news
I hope they have lots of grains of salt at Texas Tech
But what about strawberries?
Not everyone’s worried about healthcare privacy



