January 29, 2025 ✒ Andrew Kantor
After having the last settlement over its role in the opioid crisis thrown out by the Supreme Court, the Sackler family has reached a new one with the collection of governments (local, state, and federal) — and this one doesn’t give the Family blanket immunity from other lawsuits. The basics of the new settlement: Note: “The deal still needs court approval, and some of the details are yet to be ironed out.” The Justice Department is suing Walgreens in a double-whammy: It’s accusing the company and its subsidiaries of not only “dispens[ing] millions of unlawful prescriptions in violation of the Controlled Substances Act,” since August 2012, and then getting reimbursed for those prescriptions from federal health programs, which would be a violation of the False Claims Act. (This is all based on four whistleblower lawsuits, which the DoJ took over.) “Our complaint alleges that Walgreens pharmacists filled millions of controlled substance prescriptions with clear red flags that indicated the prescriptions were highly likely to be unlawful, and that Walgreens systematically pressured its pharmacists to fill prescriptions, including controlled substance prescriptions, without taking the time needed to confirm their validity. But wait, there’s something else You might expect Walgreens to respond with a typical denial and ‘see you in court,’ but the company took an interesting tack. It argued that there’s no law requiring pharmacists to pay attention to “red flags” when it comes to filling prescriptions: “We are asking the court to clarify the responsibilities of pharmacies and pharmacists and to protect against the government’s attempt to enforce arbitrary ‘rules’ that do not appear in any law or regulation and never went through any official rulemaking process. The good folks from the Academy of Employee Pharmacists are throwing a big ol’ shindig — a networking event in Marietta for every pharmacist and technician in the state. (And they even throw in some CE so maybe you can claim it as a tax deduction*.) The deets: Saturday, February 22, 2025 6:00 – 9:00 PM Dave & Buster’s in Marietta (map) Want more info? Sure thing — click here for everything you need to know. * We’re not tax experts, so you probably want to ask someone who is, but it seems like you could. Scientists still aren’t entirely sure why we need sleep, although “to clean out junk from the brain” seems to be at least one reason. Research out of the University of Rochester seems to bear that out, showing how the glymphatic system does its cleaning when powered by neurotransmitters and brain fluids. The pharma twist: They also found that Ambien, aka zolpidem, can suppress that cleanup process. That would mean that long-term use could lead to a buildup of toxic proteins in the brain and potentially lead to (or at least factor into) diseases like Alzheimer’s. But you know the mantra: More research is needed. Tau proteins are … let’s call it “part of the Alzheimer’s pathology.” Scientists know it’s somehow involved in the disease but not exactly why or how. Now University of Pittsburgh researchers have an interesting Could it help to “fine-tune the brain’s immune response,” they wonder? Or maybe there’s a way to attack those viral proteins before they elicit an immune response. Either way, as above (and always), they “plan to explore those questions in future research.” * Well, subdued “Frequent social media use tied to higher levels of irritability”. Trigger warning: This is a story about abortion. One dose of the prescription-only drug acetate (aka Ella) prevents fertilization after sex, like a better version of Plan B. Now a preliminary study by US and Mexican researchers has found that doubling the dose from 30 mg to 60 mg and adding misoprostol makes it terminate a pregnancy, just like mifepristone + misoprostol. In fact, it seems to be slightly more effective. Ulipristal has been FDA-approved for about 15 years for preventing pregnancy, and this finding will undoubtedly have the usual suspects trying to ban it. That has OB/GYNs concerned. As one put it, “There is a risk that the findings of this study could be misapplied and used by politicians to try to restrict ulipristal for emergency contraception.” A Mississippi state senator has filed a bill called “the Contraception Begins at Erection Act.” As written by Sen. Bradford Blackmon, the bill would make it “unlawful for a person to discharge genetic material without the intent to fertilize an embryo.” Well, it’s time to say good-bye to all you wonderful readers. After today, GPhA’s astounding Holly Hanchey will take over GPhA Buzz, which will continue on its weekly schedule. It’s been great fun writing these the past … yikes, almost 8 years. And who knows what the future holds? Thank you all for reading, thank you all who are GPhA members, and thanks to everyone who’s taken the time to write in. I wish you all fair winds and following seas, open roads*, and straight flights. My watch is over. * People in Atlanta can only dream Walgreens in the crosshairs, Mississippi’s hard choice, the risk of Ambien-powered sleep, and more
Sacklers settle lawsuit … again
DoJ targets Walgreens
Party (and learn) with AEP
How Ambien can hurt sleep
Herpes – dementia connection?
theory hypothesis — one that involves the herpes simplex virus (HSV-1). They think that the virus might trigger an immune response in the brain, and part of that response is the release of tau proteins to protect the brain. When the viral infection is cleared*, those tau proteins might hang around, eventually helping to ‘clog’ the brain.Captain Obvious watches “Squid Game 2” instead
Mifepristone alternative
Elsewhere: Smaller Government edition
Good-bye, farewell, and … amen?
January 22, 2025 ✒ Andrew Kantor
You probably know about the whole ‘telehealth prescribing of controlleds’ issue. During the pandemic it became a big thing. Afterwards, the DEA wanted to end the practice but got a ton of pushback so it postponed any changes for a year. Then it thought about doing it again, and got just as much pushback. The latest: Seeing the writing on the wall, the DEA has now floated the idea — sorry, “released a notice of proposed rulemaking” — that would create three categories of telehealth prescribers. Category 1: “Special registration” — for mid-level practitioners to prescribe schedule III-V controlled substances via telehealth. Category 2: “Advanced special registration” — for those who want to prescribe schedule II controlleds. They could only prescribe within the state they practice in, and no more than half of their scripts could be via telehealth. Category 3: For telemedicine platforms to prescribe schedule II-V controlled substances. The agency is also proposing various fees for the registration (some of which are pretty hefty), as well as other requirements, e.g., checking PDMPs for abuse. But right now it’s just a proposal, so there’ll be more to come, for sure. Cobb County is suing insulin makers and PBMs, accusing them of colluding to keep the price of insulin high. Officials say the county was overcharged “in a price-fixing scheme,” and it wants its money back. The words “racketeering” and “deceptive trade practices” turned up, so you know this is serious. Who is the county suing? The usual suspects: Eli Lilly, Novo Nordisk, and Sanofi-Aventis, and CVS Caremark, Express Scripts, and OptumRx. As usual, we’ll remind you that the scientists who first created insulin for diabetes 100+ years ago refused to patent it specifically so it would always be affordable. Congrats to the UGA College of Pharmacy, which scored almost $1.2 million in a grant from the Georgia Opioid Crisis Abatement Trust (GOCAT) to help fight the opioid crisis in rural Georgia. Specifically, the team will equip pharmacists in smaller communities with the tools, training, and support necessary to provide life-saving resources, reduce stigma, and establish essential support networks for individuals at risk for overdose. A survey by Rite Aid found that a lot of people don’t know what a pharmacist can do for them. Here, have some numbers: 72% of people said they were familiar with the fact that pharmacists dispense medication. (Yes, that implies that 28% of people don’t know that pharmacists dispense meds.) Of course, you might not offer all these services — heck, you might not have time — but it’s worth knowing that there are a lot of people who think of pharmacists as just bottle-fillers … and apparently 28% think you just hang around as eye candy. Bird flu was found on a commercial farm in Elbert County — the state’s first case of H5N1 in a commercial setting. That means not only are all operations within 10 km* of the farm being quarantined pending further testing, but “… poultry exhibitions, shows, swaps, and sales (flea market or auction market) in the State of Georgia are suspended until further notice.” * Yes, the Georgia Department of Agriculture used kilometers. %$@*& commies. Another case when you don’t need opioids: after wisdom-tooth removal. A study out of the University of Rochester found that not only did OTC medications (400 mg ibuprofen plus 500 mg acetaminophen), work, they worked better than the hard stuff (5 mg hydrocodone and 300 mg acetaminophen). Participants taking the non-opioid medications reported significantly less pain during the first two days after surgery when pain is most severe and were more satisfied with their pain management and slept better, compared to those taking opioids. CMS is preparing the next round of its drug-price negotiations, and it released the list of 15 drugs that will be subject to the forces of capitalism. Not surprisingly, brand-name semaglutide (Ozempic, Rybelsus, Wegovy) is on the list. According to CMS, “These 15 drugs, together with the 10 drugs that Medicare already negotiated, represent about a third of Medicare Part D spending on prescription drugs.” It’s actually about 36%, and yeah, that’s a lot. Lowering the price Medicare pays will have a ripple effect, too — it will help reduce seniors’ co-pays (although those are now capped at $2,000 thanks to the Inflation Reduction Act), and it will also cut state and federal spending on Medicaid. Next up: The drugmakers have until the end of February to choose whether to negotiate or not participate in Medicare.Cobb County’s lawsuit, DEA’s next idea, sick Georgia chickens, and more
DEA’s telehealth plan
Cobb County is ticked off about insulin
UGA gets $$$ to fight opioids
If they don’t know you by now…
ICYMI: Georgia chickens get the flu
“At no time did hydrocodone outperform the nonopioid”
Next Medicare negotiations
January 15, 2025 ✒ Andrew Kantor
In case you haven’t heard, the Georgia Board of Pharmacy is reminding pharmacists and technicians that the board will never, ever call and ask you for money. Scammers, on the other hand, will do just that — and even fake BoP phone numbers (so don’t trust your Caller ID). That’s right — today, January 15, is the deadline to submit a nomination and tell us about an extraordinary person or two. Help choose the best of the best in Georgia pharmacy — with the 2025 awards being presented with both pomp and circumstance at the Georgia Pharmacy Convention on Amelia Island, Fla. What awards, you ask? The details are at GPhA.org/awards, but here’s the list: All these nominations come from you, our members. That’s what gives them meaning. And it starts now. Visit our awards page at GPhA.org/awards for more information on award criteria, and to make your nominations. Remember: The deadline for submissions is TODAY, January 15, 2025. The insurance company is suing Novartis, Pfizer, Teva Pharmaceutical, and others (Actavis, Dr. Reddy’s, Glenmark, Sandoz, and more) claiming they “conspired to overcharge the insurer, consumers, and the federal government for generic drugs.” The complaint, filed Dec. 31, claims the drugmakers communicated secretly at trade conferences or through phone calls, beginning in 2012, to determine the market share, prices and bids of certain drugs. If communication was in writing, they destroyed the evidence, Aetna claimed. This suit is in addition to similar action filed by states (some of which have been settled), as well as Department of Justice and congressional investigations. In a second report on PBMs, the Federal Trade Commission found that — shockingly — the companies have been marking up the prices of medications at their own pharmacies, costing patients and taxpayers millions … if not billions. From 2017 to 2022, the companies — UnitedHealth Group’s Optum, CVS Health’s CVS Caremark and Cigna’s Express Scripts — marked up prices at their pharmacies by hundreds or thousands of percent, netting them $7.3 billion* in revenue in excess of the acquisition costs of the drugs. The FTC is already suing PBMs over steering diabetes patients to higher-priced drugs; this adds fuel to the fire. * “Probably an underestimate,” said an FTC spokesperson Where marijuana is legal, patients fill fewer prescriptions for benzodiazepines. They also fill slightly more prescriptions for antipsychotics and antidepressants, while neither barbiturates nor sleep meds are affected. All this comes out of research from Georgia Tech policy wonks based on prescription data. And note: The numbers they looked at were for prescription fills, not prescriptions written, suggesting that the diagnoses were there but patients decided to self-medicate. Does pot work as well as prescription meds? They don’t know: “Our research does not clarify whether the changes in dispensing patterns led to measurable changes in patient outcomes.” Did you know that the International Committee on Taxonomy of Viruses has renamed just about every virus you’re likely to encounter? We’re not just talking about calling monkeypox “mpox.” We’re talking wholesale renaming. HIV-1 would henceforth be known as Lentivirus humimdef1. SARs-CoV-2, the virus that causes Covid, would be known as Betacoronavirus pandemicum. Ebola was now Orthoebolavirus zairense. This has actually been going on quietly over the past four years, and it wasn’t a big deal until December, when the US National Library of Medicine said it would update its gene and virus databases to use the new names. Cue the uproar, even though virologists have been living with a mess of unconnected names for years. The good news is that everyone can still use the common name: “Researchers […] can keep using HIV in papers the same way researchers use “mouse” and not mus musculus.” And the better news is that they now have something to argue about on social media. In a surprising move, the FDA is proposing that any new anti-obesity drugs show at least a 5% weight loss over a year in order to be considered for approval. The agency rarely sets a standard like that — the market usually takes care of it. Heck, that might even be the case here. That’s a low bar compared with the 15% to 20% weight loss at one year that Eli Lilly and Novo Nordisk have already reported with their approved weight loss drugs […] Any competing products would likely have to come close to or beat that benchmark to have a commercial chance. This is draft guidance, meaning it first has to go through the whole approval rigmarole, and even if approve it’s not binding — just a strong suggestion. If you know what we mean. My little local paper runs a section called “Looking Back,” with news from 100 years ago: Good thing times have changed — we’ve made such progress in the last 100 years. Imagine reading about people getting measles, chicken pox, mumps, diphtheria, or whooping cough today. Oh, wait. If you’re like most people, you drink a lot of elderberry juice — with breakfast, as part of a cocktail, and at holiday celebrations. Good news: It can help with weight management and overall metabolic health. Researchers at Washington State University found that drinking elderberry juice seems to improve metabolism and help the body burn fat, and that leads to both lower blood sugar and lower insulin levels. Oh, and it also improved subjects’ gut biomes. “Elderberry,” said the lead researcher, “is an underappreciated berry.”Aetna suing drug makers, FTC bashing PBMs, committee renaming viruses, and more!
Scam alert
TODAY is the deadline for GPhA awards nominations
Aetna sues drugmakers
PBMs (still) behaving badly
Does pot beat benzos?
Ebola, by any other name…
You must be this effective to join the weight-loss club
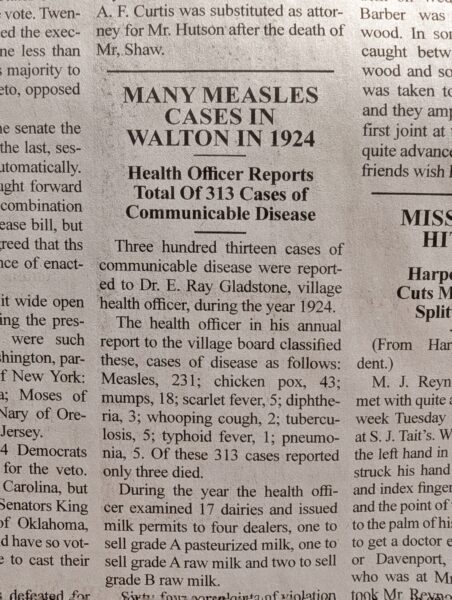
How far we’ve come
Your father smelt of better metabolism
January 08, 2025 ✒ Andrew Kantor
Regardless of what you think of his time as president, Jimmy Carter was one of the few truly good people to hold the post — something that was made more obvious once he left office. A national day of mourning is more than just a formality for a fallen leader. In this case it’s well earned. Here’s hoping President Carter enjoys his time with Mr. Rogers and Charles Schulz. Ritalin can make you a better driver. For reals, according to Australian researchers. If a person has ADHD, this is apparently a given — “For a medicated person with ADHD, driving without it can feel a bit like driving without their glasses*.” But what about the rest of people? That’s what Aussies wanted to find out. They collected 25 healthy people who fit that description and gave them either 10 mg of methylphenidate or a placebo, then put them in driving simulators. “Methylphenidate significantly improved driving performance by reducing lane weaving and speed variation, particularly in the latter half of the drive,” the authors report. Importantly, they note that subjects were given a low dose. People who get Ritalin from the kid who mows their lawn often take higher doses, but that can lead to “a ‘tunnel vision’ effect […] that could limit a driver’s ability to respond to sudden or unexpected obstacles.” * As someone with ADHD who takes methylphenidate, I can report that this is just silly. Within a month of each other, two independent pharmacies in the Habersham area — Crossroads Pharmacy and Habersham Drug — have closed their doors thanks, the owners say, to the reality of a pharmacy market controlled by PBMs. Sure, you probably heard about the Change Healthcare data breach that affected 100 million people and caused a lot of headaches. And you may have heard about the Kaiser Foundation Health Plan’s breach affecting 13.4 million people. But those are just the two largest in 2024. In fact, there were a lot more; HHS reports a total of “677 major health data breaches affecting more than 182.4 million people” as of late December. Here are just the 10 biggest: As of Dec. 20, some 6,584 major health data breaches affecting more than 746.6 million people had been posted on the HHS OCR website since September 2009. That’s about the equivalent of every American having their PHI compromised at least twice in a major health data breach. The HHS Office for Civil Rights is proposing a new rule that would require businesses and other entities covered by HIPAA to strengthen their cybersecurity measures. In general, it would require more testing, written assessments, “and vulnerability scanning at least every six months and penetration testing at least once every 12 months.” The US spent $4.9 trillion on healthcare in 2023, according to the numbers crunched by CMS’s Office of the Actuary. That includes what private insurers paid, what the government paid, and what individuals paid. It’s 7.5% above 2022, and GLP-1 drugs were only just getting started. Zepbound is expected to lead the GLP-1 juggernaut in 2025, which alone is expected to add a full percentage point to the cost of insurance premiums. And that’s just the start: These GLP-1 drugs are adding to general healthcare inflation that is projected to increase employer-sponsored health insurance coverage by 9%, eclipsing $16,000 per employee in 2025. Pfizer and PhRMA (the pharma industry trade group) are among the businesses donating a heck of a lot of money to the Trump inauguration and political agenda. [S]everal industry leaders — including Pfizer’s CEO Bourla — have been cozying up to Trump personally as they attempt to navigate potential changes to the healthcare landscape under his incoming administration. Telehealth company Hims has donated $1 million, saying, “[W]e stand with leaders and advocates who are committed to improving America’s broken healthcare system.” In an effort at one-upmanship, after meeting with Trump at Mar-A-Lago, Pfizer pledged to christen its headquarters with Trump’s name and erect a statue in his honor, while PhRMA offered to have its members rename the days of the week for Trump’s family. “We expect to hear back from the incoming administration on Ericsday,” said board chair Daniel O’Day Admit it: For a moment — just a moment — you thought that last part could be true. It’s January, which means it’s time for drugmakers to raise their prices more than the rate of inflation … at least in the US. Inflation here is about 2.75%, but manufacturers are raising the list prices of at least 250 meds by a median of 4.5% this January. There’s some good news: That’s about half of how much they used to raise them, and it’s (so far) about the same as last year. Oh, that 2.75% is only for existing drugs. New drugs tend to be a lot more expensive. In 2024, for example, the price of debut drugs was 35% higher than in 2023. As always, prices for brand-name drugs in the US are the highest in the world. Price hikes are needed for executive bonuses, to fund stock buybacks, and to pay for marketing. On the other hand, prices for generic drugs are among the lowest, so … yay? In Canada, the teenager who was in critical condition with H5N1 flu in British Columbia has made a recovery — possibly a full recovery. Her discharge info isn’t being shared, but her diagnosis and treatment is: “She had respiratory failure, pneumonia in the left lower lobe, acute kidney injury, thrombocytopenia, and leukopenia.” Her treatment included oseltamivir (Tamiflu), but she still required intubation. Then she was given amantadine (Gocovri) followed by baloxavir, along with 3 days of daily plasma exchange among other treatments — you can read the details here. You are permitted to say “Yikes.” But again, she’s recovered and been discharged. The news wasn’t as good for the patient in Louisiana, whose death was announced Monday. Unlike the Canadian teen, the Louisiana patient “was over the age of 65 and was reported to have underlying medical conditions.” Side note: The Louisiana patient contracted the bird flu after exposure to “a non-commercial backyard flock,” which might refer to backyard poultry. The Canadian teen? Health officials still don’t know where she contracted it. The widespread use of GLP-1 drugs was supposed to save money in the long run by reducing spending on a host of other medical conditions, from diabetes to kidney issues to knee replacements. But two years into the boom, we’re not seeing it. Both PBM Prime Therapeutics and the Congressional Budget Office say “there does not appear to be any direct empirical evidence pointing to a medical cost offset.” At least not yet. You might connect to the Internet at 40, 50, or 100 Mbps (aka 100 million bits per second), but your brain? Not so fast. According to CalTech researchers, your 7 lbs of meat is processing information at a rate of — wait for it — 10 bits per second. Not megabits — bits. [insert joke about your favorite politician here] That said… [O]ur bodies’ sensory systems gather data about our environments at a rate of a billion bits per second, which is 100 million times faster than our thought processes. In other words, we’re 10-bit brains in a gigabit world.Better driving with Ritalin; your slow, slow brain; 2025 price hikes, and more
One of a few good men
Driving stimulation
Two more pharmacies close
Hackers gonna hack
On that note…
I can’t wait to see the 2024 numbers
In fact…
They’re not bribes, they’re pledges of support
It’s time to rise!
Bird flu follow-up
Short takes
Waiting for the savings
Thinking, Slow and Slow
December 28, 2024 ✒ Andrew Kantor
The FDA has approved a generic version of liraglutide (Novo Nordisk calls it “Victoza”) as a daily injectable for people with type 2 diabetes, making it the first generic GLP-1 agonist. Sure, liraglutide is a bit older (and a little less effective) than semaglutide or tirzepatide, and it requires a daily injection instead of a weekly one, but the approval still marks a big breakthrough for patients looking to lose wei— um, for patients looking to control their diabetes. With tirzepatide supposedly out of shortage (and semaglutide possibly coming out of shortage soon), a lot of GLP-1 patients are about to see their costs skyrocket. But they might be willing to deal with a daily shot for a fraction of the price. In the interest of completeness: Yes, there is already an “authorized generic” version of liraglutide from Teva, but it only sells at a 14% discount from the brand-name drug. This is a little scary: Northwest Naturals is recalling its Feline Turkey Recipe frozen pet food. It’s already killed at least one cat because the food contained H5N1 bird flu. Not only can cats get H5N1 via food, but health officials know they can transmit it to humans. And then there’s the issue of how the virus got into the food in the first place…. Remember that first serious case in the US — the one in Louisiana? The CDC tested the flu strain involved and found that “the virus likely mutated in the patient to become potentially more transmissible to humans.” Yay. To treat opioid dependence, there’s methadone and buprenorphine. But what about meth or other amphetamine dependence? There’s nothing. Or is there? Australian researchers say they’ve found a drug that can reduce meth addicts’ need for a hit — and better still, it’s an existing, approved medication: lisdexamfetamine, aka Vyvanse. A 15-week study of 164 adults found that yep, taking the ADHD med reduced patients’ self-reported meth use. Overall, the participants who received lisdexamfetamine reported 8.8 fewer days of methamphetamine use on average during the maintenance phase than the placebo group. The treatment group also reported 2.9 times higher rates of treatment effectiveness and 3.8 times higher treatment satisfaction. As always, more research is needed; the trial was small. Still, with Vyvanse already approved, it could be a much shorter road to using it to wean people off the hard stuff. “Are antibiotics linked to dementia?” No. (At least among healthy adults.) As baby-powder manufacturers move away from talc to corn starch, the FDA is proposing a standardized test for any products still containing talc to ensure they don’t contain asbestos. No one has determined what a safe level of exposure is, and of course the FDA doesn’t regulate what’s in cosmetics. The rule would require [insert science here] testing, and… If the manufacturer fails to comply with testing and record-keeping requirements, the proposed rule allows the FDA to declare that product as adulterated under the Federal Food, Drug, and Cosmetic Act.Deadly cat food, generic GLP-1 approved, antibiotics are safe, and more
First generic GLP-1
Bird flu in cat food
Speaking of bird flu…
A drug for meth abuse
Saving you a click
Closing the barn door
December 26, 2024 ✒ Andrew Kantor
Georgia is one of the states being hit hardest by the holiday flu surge, which could mean it’s gonna get worse after all that mistletoe snogging. And by “surge,” health officials mean cases have doubled in the past week — or, as one Roswell doc put it, “exploded.” All these adjectives mean it might be time to think about those pesky masks again*…. * Kidding, of course. Freedom! In case you’re interested in how flu strains get their names — both the H and N parts (e.g., H5N1) and their full names (e.g., A/Sydney/05/97 (H3N2)), Forbes has you covered in excruciating detail. Whooping cough, aka pertussis, has been rising like a [insert inappropriate metaphor here] and now cases are at the highest level in a decade. And it’s Not. Slowing. Down. This year cases are 6 times higher than last year. Yeesh. It’s quite contagious, and symptoms range from the mild (not even knowing you have it) to bad enough that you break ribs from coughing. And it can last for months. Scientists are working to create a vaccine so people can be protec— wait, what’s that? It’s entirely preventable with a vaccine that’s been around since 1949? But vaccination rates have fallen to the point where herd immunity is compromised? Really big. Based on a report from Truveta, which gleans data from medical records, during 2024 GLP-1 agonists made up 5% of all prescriptions in the US. Yep, “As of September, one of every 20 prescriptions written for adults was for one of these drugs.” Atogepant was already approved to prevent migraines, but it also seems to stop them in their tracks, according to a study out of Albert Einstein College of Medicine. In the study, people taking the drug atogepant were less likely to have a migraine on the first day of taking the drug compared to those taking a placebo. They also had fewer migraines per week during each of the first four weeks of the study and fewer migraines during the study overall than those taking a placebo. It’s a big deal because it means that, rather than try one drug after another and hope it works, patients pretty much know immediately. And if it does, they’ve got something that works both long term (atogepant is a monthly injection) and immediately. We all know the FDA is planning to remove phenylephrine from the shelves because it doesn’t work. Now a bunch of Australians have filed a class-action suit against Johnson & Johnson, claiming the company knew phenylephrine was ineffective but still marketed products — Benadryl and Sudafed, notably — as a decongestant. “Johnson & Johnson has manufactured and marketed a medication that decades of evidence have shown doesn’t work as claimed, relying on outdated, fallible studies to sell the Australian public products that don’t do what they claim on the packet.” Wondering exactly how CMS and drug makers negotiated the prices of the first 10 drugs subject to negotiation? Wonder no more. CMS has made available the details of the process for each of them, and the explanation of how it determined the final price Medicare was willing to pay. They’re all on this page, but if you’d like a sample, here’s the PDF for Eliquis. Good night!GLP-1s dominate the market, flu clobbers Georgia, Aussies are angry at J&J, and more
Send in the flu (it’s already here)
Decoding the flu
Speaking of illness surges…
How big are GLP-1s?
Migraine med is better than expected
Aussies sue J&J
A little light bedtime reading
December 24, 2024 ✒ Andrew Kantor
Georgia’s Buddy Carter has been tapped to chair the House Energy and Commerce Subcommittee on Health, where he promises to be “in lockstep with President Trump… … to tackle our nation’s chronic disease epidemic, increase price transparency, incentivize competition, combat harmful health care consolidation, fight the scourge of fentanyl, and build a health care system that puts patients before profits.” Every year the flu vaccine turns out to be somewhere from 20% to 80% effective. That’s not because health officials got the strains wrong. It’s because most people will develop antibodies to just one of the three or four strains in the vaccine. If it happens to be the wrong one for that year … tough cookies. But now Stanford scientists think they A) know why this is the case, and 2) figured a way around it — a way to make patients produce antibodies to all the strains. The why is simple: Genetics. (It’s not, as they thought, a matter of what subtype hits the immune system first.) Not a lot to be done about that; each person’s B cells just happen to be primed differently. The how: Instead of four separate antigens in a vaccine, they make one big one that contains all four of that year’s hemagglutinin varieties. Thus the immune system’s B cells only have to target one of the four: [A]ny B cell that recognizes and begins ingesting one or another of the vaccine’s four hemagglutinin types ends up wolfing down the entire matrix and displaying bits of all four antigens on its surface, persuading the immune system to react to all of them despite its predisposition not to. […] This, in turn, makes helper T cells much more likely to stumble on a sample from the antigen they love to hate. There’s more to it than that, of course, but this item is pretty long already. Read the article for the details, and be ready when the tech makes it out of the lab. Well that’s a surprise: A 44-year study of 5,000 men found that those who used cannabis had less of a cognitive decline than those who didn’t use it. Specifically, “Cannabis users experienced 1.3 IQ points less decline over 44 years compared to nonusers.” Those shifty Danes at the University of Copenhagen found it even held true if they started using it before they turned 18, and it didn’t matter how frequently they used it. Apparently, despite anything you might have heard, only one type of drug (well, maybe two) works to treat ADHD in the short term: stimulants (“and to a lesser degree the norepinephrine reuptake inhibitor atomoxetine”). That’s based on a network meta-analysis by British researchers of 100 clinical trials including almost 5,000 adults, and it takes into account both clinician- and patient-reported outcomes. Non-pharma treatments? Ineffective. The bad news: Stimulants helped with ADHD’s emotional dysregulation, but not its other symptoms (e.g., executive function, like being organized and meeting deadlines), so “they fail to improve broader outcomes like quality of life.” In other words, kids on stimulants had better focus, but didn’t necessarily do any better at school. So the Brits conclude that “adult ADHD most likely requires a more holistic approach to address broader challenges that impact an individual’s quality of life.” The experimental cancer drug dostarlimab (GSK calls the PD-1-blocking antibody “Jemperli”) did what can only be called an astounding job in its trials: It “completely eradicated rectal cancer tumors without the need for surgery, radiation treatment, or chemotherapy.” Yep, it was 100% effective — that’s why it was given Breakthrough Therapy Designation status from the FDA this week, meaning it’ll be fast-tracked so patients can have access to it sooner. GSK hopes to have it available within 3 years. It’s been 30 years, but the FDA just redefined its official designation of “healthy” food, and will soon have a spiffy graphic that food makers can put on their products. What’s “healthy”? Per the agency, the food must… Out: “fortified white bread, highly sweetened yogurt, and highly sweetened cereal” In: avocados, nuts and seeds, higher fat fish, olive oil, and water Companies can start using the designation now as long as they pinkie-promise that their food will meet the requirements by 2028. A new British study found that vegetarians who ate plant-based meat alternatives (looking at you, Beyond Burger) “had a 42% increased risk of depression compared to vegetarians who refrained from PBMAs.”Pot can improve your brain, the only effective ADHD treatment, Buddy Carter gets an upgrade, and more
Carter to head health subcommittee
Improving the flu vaccine
Shaggy’s gonna be the smart one
There’s only one ADHD treatment
Cancer drug scores 100% in trial
“Healthy” food: Water in, Froot Loops out
Speaking of healthy eating….
December 21, 2024 ✒ Andrew Kantor
Great news: Mounjaro and Zepbound are now officially officially out of shortage, as the FDA has confirmed — based on data from Eli Lilly — that there’s plenty to go around. And what of all the evidence that tirzepatide isn’t available? Well, that only comes from pharmacists and patients, and Lilly promises that’s not true. Wrote the FDA: We conclude that this information does not undermine or outweigh the evidence demonstrating that Lilly’s supply is currently meeting or exceeding demand and that, based on our best judgment, it will meet or exceed projected demand. Compounding pharmacies will have 60 days to stop dispensing tirzepatide injections, and outsourcing facilities (i.e., 503Bs) will have 90 days to stop. Tell your patients: You’ve got Mounjaro and Zepbound back in stock! The agency filed a civil complaint against the pharma giant, alleging CVS “Knowingly Dispensed Controlled Substances in Violation of the Controlled Substances Act and the False Claims Act.” What’s it claiming the pharmacy giant did? In no particular order: The complaint alleges that CVS’s violations resulted from corporate-mandated performance metrics, incentive compensation, and staffing policies that prioritized corporate profits over patient safety. CVS set staffing levels far too low for pharmacists to both meet their performance metrics and comply with their legal obligations. The above link goes to the DoJ press release; click here for a news article if you prefer. Know a PharmDawg who has “advanced conversations around inclusive excellence”? Then there’s good news for you (and for them): Nominations are being accepted for the 2025 William T. Robie III Inclusive Excellence Award, which is given to just such a person. The award was established to honor the college’s first African American student and graduate, William Robie of the class of 1970. So nominate a deserving PharmDawg today! The award will be presented at the 2025 William T. Robie III Inclusive Excellence Lecture on Thurs., Feb. 6, at 12:30 pm. Once again we flip the Coin of Knowledge™ to see whether moderate drinking is better than not drinking at all. And this time the answer is … yes, it’s better! At least according to a review by the folks at the National Academies of Science, Engineering, and Medicine. Drinking a little, NASEM says, “was associated with a lower risk of nonfatal heart attacks and strokes, as well as a lower overall risk of death.” And although it ups your odds for breast and colorectal cancer, “no broader conclusion could be made for most other cancers.” We’ll see you at the next coin flip. … to Dr. Mandy Reece, who’s been upgraded from interim dean to really-and-for-true dean of the School of Pharmacy at PCOM Georgia. (She got her PharmD at Mercer, by the way.) High-five*, Doc! * Followed by some hand sanitizer — no offense, but it is flu season As more people are taking GLP-1 agonists to lose weight, it also means they’re going to their GPs more — and identifying other conditions they have. That’s leading to their getting the care they need for issues from sleep apnea to osteoarthritis. Health-data firm Truveta found, looking at medical records, that “first-time diagnoses of sleep apnea, cardiovascular disease, and type 2 diabetes” have all increased within a couple of weeks of starting on a GLP-1 drug. Even CPAP maker ResMed has seen its revenue jump 11% in its latest fiscal year, which it attributes to GLP-1 drugs. In addition to obesity-related conditions, some patients are being prescribed the drugs to lose weight and become eligible for services, including organ transplants, fertility treatments, or knee replacements, according to interviews with seven doctors and five other health experts. While this might result in higher costs in the short term, hopefully the long-term benefits will be significantly greater … provided, of course, patients can stay on the drugs. Louisiana, which already has one of the worst healthcare systems in the country, and where people are among the least healthy, is now forbidding state health workers from promoting flu, Covid, or mpox vaccines. Staffers were also told that it applies to every aspect of the health department’s work: Employees could not send out press releases, give interviews, hold vaccine events, give presentations or create social media posts encouraging the public to get the vaccines. You would think we’d have learned from Covid-19, but nope. All the warning signs are there, and there early, but read “How America Lost Control of the Bird Flu.” DoJ sues CVS, there’s Mounjaro on your shelf, latest drinking verdict, and more
Look who’s back
CVS unlawfully filled opioid scripts says DoJ
Attention PharmDawgs!
Today, moderate drinking is…
Congrats…
Another GLP-1 benefit: doctors visits
Elsewhere: Going all in
The Long Read: Fool Me Twice edition
December 19, 2024 ✒ Andrew Kantor
Why didn’t PBMs do more to stop the flow of opioids? Because, it turns out, they were paid by drug makers to make sure patients got as many painkillers as possible. For years, the benefit managers, or P.B.M.s, took payments from opioid manufacturers, including Purdue Pharma, in return for not restricting the flow of pills. As tens of thousands of Americans overdosed and died from prescription painkillers, the middlemen collected billions of dollars in payments. I could paste quote after quote, but it’s worth reading the whole story — the New York Times investigation that uncovered how PBMs conspired with drug companies to remove roadblocks to opioid prescriptions. The two groups raced to the ethical bottom of the barrel: Pharma companies threatened to reduce rebates to PBMs, and PBMs threatened to restrict prescriptions. Because the P.B.M.s often shared a portion of the rebates with the insurers and employers that hired them, these clients had a financial incentive not to impose restrictions. Purdue and the P.B.M.s sometimes reminded clients of this when they considered limiting access. The CDC has reported the first severe case of H5N1 bird flu in a human — a hospitalized Louisiana patient who had contact with backyard, not commercial, poultry. This is the 61st human case reported in the US, although there are probably a lot more going unreported. Our friends up north have already seen at least one severe case — a teenager who was hospitalized* in critical condition in British Columbia last month. (The Canadian government refuses to comment on his or her condition.) Feline danger: A new study says “that domestic cats could potentially prompt a public health crisis” because they can interact with both livestock and humans, and act as a “bridge” for the virus to become more transmissible to us. * Technically hospitalised The FDA has given Veozah (fezolinetant) — the drug used to treat hot flashes from menopause — a new boxed warning because of the risk of serious liver injury. We made this update after reviewing a postmarketing report of a patient with elevated liver blood test values and signs and symptoms of liver injury after taking the medicine for about 40 days. The agency also recommends increasing the frequency of liver blood testing, especially for the two months after a patient starts using it. Taxi and ambulance drivers seem to have lower rates of Alzheimer’s, although it’s unclear why this might be the case. Researchers from Mass General Brigham looked at the death certificates of about 9 million people whose occupation was listed, and they found that while overall Alzheimer’s was the cause of death for about 3.9% of people, only 1.03% of taxi drivers and 0.74% of ambulance drivers died from it — the lowest rates among any profession. If you saw that two types of high-stress drivers had lower rates of Alzheimer’s death, you would raise an eyebrow, too. But why is this the case? The thought is that it has to do with the use of the hippocampus for spatial reasoning, but the authors are clear, “We view these findings not as conclusive, but as hypothesis-generating.” The discredited study that claimed hydroxychloroquine could help treat Covid-19 has (finally) been withdrawn by the author and retracted by the journal that published it … but not before a lot of damage was done. The French Society of Pharmacology and Therapeutics said the paper constituted a clear example of scientific misconduct, which was marked by manipulation and bias to “falsely present” the drug as effective against COVID-19. […] “The promotion of the results led to the abusive prescription of hydroxychloroquine to millions of patients, leading to unwarranted risks to millions of people and potentially thousands of avoidable deaths.” You might have noticed that there seem to have been a lot of food-borne disease outbreaks and recalls. In fact, “Food and cosmetic recalls […] nearly doubled from 2012 to 2024.” What’s going on? It’s most likely a combination of factors, including people eating more processed foods, “increased globalization of food production,” and even some missed inspections. Within US states, there are about 3,000 different jurisdictions for food safety […] “And not everyone’s on the same page.” Experts publishing in the British Medical Journal warn that princesses depicted in Disney movies (and remakes and remakes and remakes) are facing a slew of health risks. As a scullery maid, Snow White, for example, finds “opportunities for social interaction are extremely limited,” increasing her risk of “cardiovascular disease, depression, anxiety, and all cause mortality.” Ditto for Jasmine: “[W]hile the Genie might sing ‘you ain’t never had a friend like me,’ the truth is that Jasmine has no friends at all.” Rapunzel’s uncut hair probably means permanent damage to her follicles, while Belle — well, “Close contact with the Beast exposes Belle to many potentially life threatening infectious diseases, such as brucellosis or rabies.” And Pocahontas? Ouch: Her cliff dive has an impressive falling time of nine seconds. Based on the falling time, we estimated the height of the cliff through simulations using coupled differential equations for height and velocity with quadratic drag. Assuming average female anthropomorphic measurements […] and standard environmental constants (drag coefficient of 1.0, gravitational acceleration of 9.81 m/s2, and air density of 1.2 kg/m3), the cliff height was estimated at 252 m. Studies on slamming dynamics of diving suggest that hand first dives from heights above merely 12 m could already be critical for clavicular compressions. He isn’t owned by Disney (yet), but Santa is facing his own health issues, as the director of Lancaster University’s Clinical Anatomy Learning Centre points out. Sure, all that body fat is good insulation, but a diet high in milk and cookies “increases the risk of developing obesity and chronic conditions such as heart disease, stroke, type 2 diabetes, osteoarthritis, and colorectal cancer.” And, he point out, “Santa’s flushed complexion is often viewed as an indication of his cheery nature — but red cheeks can also be a symptom of rosacea, a chronic skin condition.”Drivers without Alzheimer’s, first severe H5N1 case, princesses in peril, and more
The Long Read: The secret payments that made sure opioids kept flowing
Now do we worry?
New Veosah warning
Driving away Alzheimer’s?
A little late….
What’s with all the food recalls?
Perhaps taking science too far
Don’t forget Kringle
December 17, 2024 ✒ Andrew Kantor
We all know that too much acetaminophen can lead to liver issues, but at lower, less-frequent doses it’s great stuff. Well, that might not be true for people over 65. A new British study found that “repeated doses of paracetamol in people aged 65 and over can lead to an increased risk of peptic ulcers, heart failure, hypertension, and chronic kidney disease.” Caveat: Although it compared 180,000 acetaminophen ‘users’ with 400,000 ‘non-users,’ it was only based on prescription information — it didn’t take into account over-the-counter tylen— er, paracetamol use. So while there appears to be a connection, you know the drill: More research is needed. Instead of systemic SSRIs like we’re using today, what if the drugs were targeted at the gut? After all, “90% of our bodies’ serotonin is in the gut,” according to a cell biologist at NYU Grossman School of Medicine, and the vagus nerve connects it to the brain. That’s why she co-led a study to see what would happen if they increased the serotonin in mice’s guts, rather than their brains. They genetically engineered some mice to have more serotonin signaling there (“which mimicked an SSRI delivered selectively to the gut”), and, lo and behold, those mice were less anxious and depressed than their littermates. “[T]o see enhanced serotonin signaling in the gut epithelium produce such robust antidepressant and anxiety-relieving effects without noticeable side effects was surprising even to us.” Even better: A guts-only delivery system would be good for pregnant women. Some studies have shown that taking ‘systemic’ SSRIs during pregnancy can affect the child in ways you don’t want to. So next up: Finding a way to target SSRI delivery. Republicans in the US House of Representatives are looking into whether CVS Caremark threatened independent pharmacies if those pharmacies participated in pharmacy hubs not controlled by CVS. That would be violating anti-trust law, and laws are occasionally enforced against pharma companies. A bipartisan group of Georgia state house members — a committee looking at ways to deal with the opioid crisis — “is considering introducing legislation next year forcing insurance companies to cover the cost of alternatives to opioid pain medications.” I.e., they would have to “cover nonopioid pain management options the same way they do for opioids.” I guess it’s Econ 101: When drugs show more benefits, pharma companies raise the price because more people will be taking them. But sometimes, just sometimes, it seems pharma raises the price of drugs even when there’s no evidence of additional benefits. That’s according to the Institute for Clinical and Economic Review. When it comes to the 10 drugs whose price increases contributed most to a rise in U.S. medical spending in 2023 — half of those price hikes “were not supported by clinical evidence and drove costs higher by $815 million.” (And yes, those price hikes were way above the rate of inflation.) Johnson & Johnson’s cancer drug Darzalex was on the list of price increases not backed by clinical evidence for the second time this year. A 7.6% rise in the treatment’s list price added about $190 million to U.S. spending, according to the report. Perspective: If Ford raised the price of its F-150 truck — the most popular vehicle in the world — by 7.6% a year from its introduction in 1975, it would cost more than $145,000 today. * The base model sold for $4,002, or $23,233 in 2024 dollars Today’s antivirals are great, for sure, but like antibiotics they’re likely to become less effective over time. A way to prevent that (or at least delay it) is by creating an entirely new class of antivirals. That’s what researchers at Rockefeller University say they’ve done. They’ve developed an antiviral — well, a proof-of concept of one — that they say represents “a wholly new way to treat SARS-CoV-2 infections.” It might also tackle other viruses including Ebola, dengue, and poxes. In short, rather than disrupting a virus’s proteases as antivirals like Paxlovid do, this new type of drug targets methyltransferase. “Even in isolation, a virus would have trouble escaping this compound. But as a combined therapy along with a protease inhibitor — escape would be almost impossible.” It has the added benefit of only affecting the virus particles, not human methyltransferases, meaning side effects should be minimal. Next up: Testing it on other viruses and even some fungal infections. And they’re looking for a drug-industry partner to turn it into a human therapy. The latest folks to develop a microscopic drug-delivery robot are at Caltech. Medical engineers there created the usual: microrobots that can withstand the brutal inside of the body long enough to deliver their drug cargo to the target. In this case, they used a “printable” hardening hydrogel that includes magnetic nanoparticles allowing the microbot spheres to be steered to wherever in the body they’re needed*. They’ve tested their bots on mice (successfully), but it’ll be a while before they can do a human study. * That could be Star Trek technobabble. All they need to do is invert the tachyon field and reroute the beam through the main deflector. CVS under anti-trust investigation, SSRIs to the gut (not the brain), risky Tylenol, and more
Acetaminophen danger
A better SSRI target?
Drug politics
CVS anti-trust questions
Georgia considers requiring coverage of alternative pain meds
Unjustified price hikes (now there’s a shock)
A different kind of antiviral
Another drug microbot