Why planes are safe, an app to detect strokes, Georgia needs flu shots, and more
24 Oct 2020
Posted by Andrew Kantor
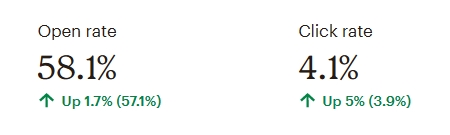
Looks like you’ve got some work to do
Georgia has the country’s sixth worst flu vaccination rate, at least over the last three years. Even Texas is ranked higher. (It’s #10.) So, you know, get those “Flu Shot Here” signs out, make a pitch to the local radio station for a PSA, or do whatever it takes. It would be nice to avoid a “twindemic” … if for no other reason than I hate that word.
Perspective: An average of 42.6% of Georgians have gotten vaccinated each year — not great, not terrible. States rank from 57.1% (Rhode Island) to 40.3% (Florida).
Pharmacists, help yourselves

You’re not alone.
This American Pharmacists Month, your colleagues need YOU. While pharmacists care for patients so beautifully, sometimes it’s hard for pharmacists to take care of themselves, isn’t it? That’s why our mission to advance healthcare includes PharmWell, a program to help Georgia pharmacists stay mentally healthy. The program addresses burnout, drug misuse, depression, and suicide.
Visit GPhA.org/foundation to make a donation or to see the programs PharmWell offers.
Why does lack of oxygen damage the brain?
It’s common knowledge (and common sense) that bad things happen to your brain when it doesn’t get enough oxygen. Just ask a SCUBA diver — but be sure to speak slowly and use small words.
But why does that happen? The answer could help treat people suffering from hypoxia (including, of course, hypoxia from Covid-19).
The nickel tour: Hypoxia triggers “hypoxia-inducible factors” (HIFs) — proteins that instruct cells to cut oxygen consumption. But it turns out those HIFs also activate other genes that can block formation of oligodendrocytes: in other words, they can cause brain damage (or lack of brain repair).
The cool news: Researchers at Case Western Reserve University say they’ve found a way to suppress that negative effect of HIFs while keeping the beneficial ones. That’s the news story, click here for the paper in Cell Stem Cell.
Good Covid news
The death rate is going down as we learn how to fight the virus.
The study, which was of a single health system, finds that mortality has dropped among hospitalized patients by 18 percentage points since the pandemic began. Patients in the study had a 25.6% chance of dying at the start of the pandemic; they now have a 7.6% chance.
The bad news: That 7.6% chance of death is still frighteningly high — much higher than the flu, for example. And the post-infection heart, lung, and brain damage will cause long-term problems for a lot of people.
More good Covid news
Airplanes, thanks to their disinfectant protocols, are virtually virus-free. So as long as people wear masks, it’s reasonably safe to fly. You’ll take your chances in the cab ride over, though.
Deep cleaning aircraft between flights is one of many tactics the airline industry is using to try to restore public confidence in flying during the pandemic. The researchers say their study proves there is virtually no risk of transmission from touching objects including armrests, tray tables, overhead bins or lavatory handles on a plane.
That’s enough — now the bad news: shortages
Even with compounders filling the gaps, a lot of drugs used to treat Covid patients are in short supply. And with winter coming it’s going to get worse.
Across the U.S. and Europe, 29 out of 40 drugs used to combat the coronavirus are currently in short supply. And those shortages are expected to grow even worse as the number of Covid-19 cases and hospitalizations surge in the coming winter months.
What’s in short supply? Here’s one of the more recent lists.
And a little more bad news: Convalescent plasma strikes out
The other day we learned that remdesivir doesn’t help severely ill Covid patients (although it’s just been approved by FDA for treating the virus). Today we find that one of the other treatment hopefuls, blood plasma transfusions from recovered patients, also showed little or no benefit.
But others say it’s too early to dismiss it, because the study wasn’t deep or comprehensive enough. And both it and remdesivir do work to some extent for people with milder cases.
Pocket stroke identifier
Yesterday we told you how a computer can detect Alzheimer’s from a person’s writing. Now comes Penn State, with a smartphone app that can diagnose a stroke. It’s 79 percent accurate — as good as an ER doc with a CT scan.
How? Having learned from actual stroke victims, the app analyzes facial motion and speech patterns “to identify abnormalities in a patient’s face or voice, such as a drooping cheek or slurred speech.”
The Long Read: What makes SARS-CoV-19 so virulent?
Many coronaviruses are good at causing damage, but this one spreads a lot more easily. Apparently SARS-CoV-19 got a few genes from some particular nasty friends.
“Compared to its older relative, the new coronavirus had acquired an ‘extra piece’ on its surface proteins, which is also found in the spikes of many devastating human viruses, including Ebola, HIV, and highly pathogenic strains of avian influenza, among others.”