What whisky cures, good news for Swedes, swappin’ Reybolds, and more
21 Sep 2021
Posted by Andrew Kantor
Sleep more, snack better
If you don’t get at least, say, seven hours of sleep a night, you’re more likely to make “poorer snacking choices,” according to researchers at an Ohio State University. (It’s based on data from 19,650 U.S. from 2007 to 2018, so this isn’t a small study.)
Compared to participants who slept seven or more hours a night, those who did not meet sleep recommendations were more likely to eat a morning snack and less likely to eat an afternoon snack, and ate higher quantities of snacks with more calories and less nutritional value.
Heck, you don’t even have to sleep — just be in bed. “Even if you’re in bed and trying to fall asleep, at least you’re not in the kitchen eating.”
One Reybold out, one Reybold in
Melissa Reybold was named GPhA’s new vice president of public policy, following in the footsteps of her husband, Greg. Melissa isn’t new to this at all — she’s been working as a GPhA member-service representative since 2013, and that’s the latest in a long line of pharmacy careers since college, from pharmacy technician to trainer to supervisor to sales rep.
“Having spent many years visiting community pharmacies and seeing the struggles they face due to PBM abuses, as well as the role pharmacists can play in patient outcomes, I’m excited to take those experiences and continue GPhA’s hard work in shaping policy in Georgia,” she said.
Looming doom of flu
Flu season is coming to Georgia, but what does that mean? Welp, no one knows. As Georgia Public Radio reports, it’s a wildcard.
The worry is that, with hospitals filled to bursting and anti-vaccine sentiment high in the state (Georgia is ranked #44 in Covid vaccinations in the country, and was #49 in flu shots last year), it could push the state into a serious crisis.
“When we have this number of COVID inpatients on top of our regular patient population, the beds and the staff are just not there, so we’re already running into issues where people are experiencing extremely long wait times, ambulances are having to wait a long time to get patients into the hospital because we just don’t have the space and staff. When you add a flu surge to that, it pushes our inpatient numbers way beyond capacity.”
Bonus: The story features GPhA Region 3 President Nikki Bryant, owner of Adams Family Pharmacy in Preston. Hi, Nikki!
Take a break
Sure, the boss might appreciate your long hours, or maybe you’re just the kind of person who gets really, really a job. Kudos to you … but (finds a study out of the University of South Australia), getting too immersed is not a path you want to go down.
“Overly engaged workers might tend to become workaholics ignoring early signals of depressed mood, continue working and develop major depressive disorders.”
What went around comes around
From whisky to quinine, “predigested beef fluid” to calcium lactate — during the 1918 flu, all sort of “cures” were being peddled for preventing or treating the disease. And it wasn’t just Cousin Jimmy who came up with it — doctors, nurses, even food companies all had treatments.
Preventative: A small daily dose of quinine. Gargling with whisky when in contact with infection.
Curative: Large doses of castor oil. Quinine and whisky. Every inducement to perspiration. Gargling with whisky, unceasing administration of small quantities of liquid nourishment as of great variety as could be obtained. In cases of great prostration where there was difficulty in retaining food, each teaspoonful of nourishment was followed by a teaspoonful of cold water. Drops of whisky were frequently inserted in each nostril.
Thankfully, we know better today.
Yeah, that
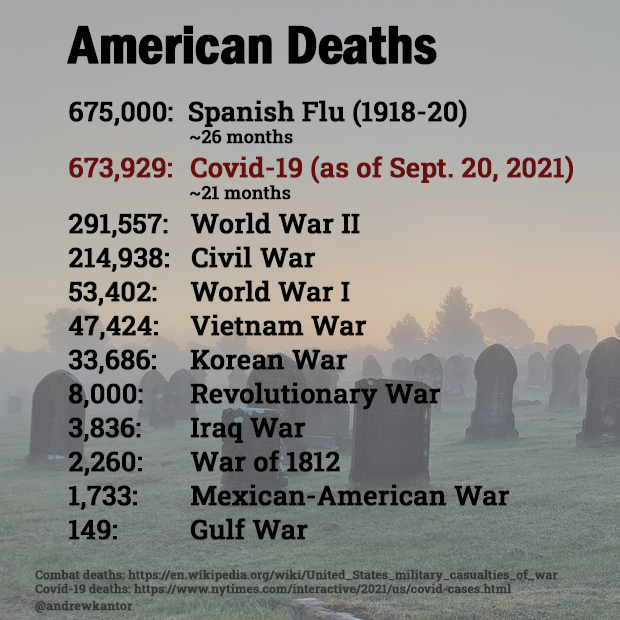
Covid-19 is about to become the deadliest disease in U.S. history.
ICYMI: Booster notes
For the young: Pfizer says it’s Covid-19 is safe and effective for kids 5-11 (at one-third the adult dose). The company is waiting for peer review of the testing, and will seek emergency-use authorization for the vaccine for kids. At the moment, 12-15-year-olds are getting the vaccine under an EUA.
For the older: An FDA committee unanimously agreed that the agency allow booster shots to people 65 and older, or those at high risk from Covid. The FDA usually — but not always — follows the committee’s recommendation.
But when to get that booster? It’s not so simple, and “immediately” probably isn’t the answer.
Delivered too early, another dose of the vaccine could end up “restarting something that was already working,” [Washington University immunologist] Ali Ellebedy said. Ellebedy recommended delaying any booster shots by at least six months from your initial course of vaccination. Eight months is better; even a year would be fine.
On the other hand…
There’s legitimate debate about whether we should be talking about third shots when so much of the world hasn’t had a first one. But as Johns Hopkins University’s Steven Salzberg argues, “Of Course We Should All Get Boosters” — because the alternative is throwing them away.
At the moment, the U.S. is wasting millions of shots per month, most of them in retail pharmacies that aren’t using their full supply. The vaccines expire quickly, and it’s simply impossible to manage the supply so that all doses are used. At a minimum, we could offer the extra doses (at the end of each day, say) as 3rd shots to anyone who wants them. The alternative is to throw them away.
And just as important, he says, is not playing down the need for boosters. That, he suggests, will be twisted by anti-vaxxers to claim that boosters don’t work at all.
Captain Obvious clips his coupons
“Suicides among Swedish men decreased after Viagra became more affordable,” based on data from 2005 through 2014 analyzed by University of California public health researchers.


