Night-shift dining advice, stressful drunkenness, antibiotic reviver, and more!
15 Dec 2021
Posted by Andrew Kantor
Who’s drinking when
You walk into a bar, and you’re stressed. If you’re a woman, there’s a greater chance you’ll drink to excess than if you’re a man. (Don’t look at me — this comes from Arizona State University, where they literally set up a laboratory “designed to simulate a bar, complete with a bartender, bar stools and lively conversations.”)
But wait! If you’ve already been drinking and then get stressed, your gender doesn’t matter — guys and gals have an equal chance of getting plastered.
“That women just needed the stress but men needed the push of already having alcohol on board shows how important this type of research is. The outcomes from alcohol use are not the same for men and women, and we cannot keep using models that were developed in men to help women.”
And the Swiss cried out, “No hiding place”
Some infections — notably salmonella — can come back even after being treated with antibiotics, and it’s not because they’re resistant. They just hide. But where?
Those industrious Swiss figured it out, searching with a fancy scanning technique* to create a slice-by-slice 3-D view of tissue. And wouldn’t you know it, the little buggers were hiding (as the University of Basel researchers put it) ”in the Police Headquarters.”
Most salmonella bacteria live in the ‘red pulp’ region of the spleen. The spleen’s white pulp triggers an immune response, and the bacteria are wiped out. Except for the ones that are hiding in the white pulp.
The white pulp thus becomes the major home of surviving Salmonella. “It’s ironic, that pathogens hide in the body exactly where they should be caught as the culprit and an effective defense against them should be activated.”
The problem is that the body doesn’t have enough neutrophils in the white pulp to work with the antibiotics. Swiss solution (being tested): Add immune therapy to the antibiotics. Testing is ongoing.
* Serial two-photon tomography, as you probably guessed
Requisite Covid-19 quickies
You take the good, you take the bad: Another study has found that the omicron variant is more resistant to vaccines, but also causes less-severe illness. But … that was with just two doses of the Pfizer vaccine, and doesn’t consider boosters.
At least the pill works: Pfizer released the results of tests on its Covid-treatment pill (Paxlovid). It’s 89% effective at preventing hospitalization and death if taken within three days of showing symptoms. Bonus: CEO Albert Bourla used the phrase “game-changer.”
About those symptoms: Only about 40% of people who get Covid-19 actually show them.
What’s Old Is New: Breast Cancer edition
A drug developed for diabetes, with the memorable name “PF05175157*,” may be a treatment for breast cancer. Simply put, Yale medical researchers found that PF05175157 can block an enzyme that breast cancer cells need to survive.
“We are currently testing this drug in combination with other approved breast cancer drugs to see if it could improve their activity, with the hope to bring the most promising combinations to the clinic to help patients with breast cancer.”
* The 7s are silent
Diabetes on the night shift
Working the night shift, it seems, increases diabetes risk. Why? Sleep researchers at Brigham and Women’s Hospital figured it out — and a simple solution.
It’s bad enough sleeping during the day and working at night, but eating at night messes with your circadian rhythm even more. Their solution: Eat during the day.
Our data indicate that a [daytime meal], with meals allocated to the habitual daytime rather than to the nighttime, can maintain internal circadian alignment and prevent the adverse effects of simulated night shift work on glucose tolerance and pancreatic cell function.
A step toward a Parkinson’s treatment
When a protein called alpha-synuclein (αS) misfolds, you get diseases like Parkinson’s and Lewy-body dementia*. Some peptides can prevent that misfolding, but it’s hit-or-miss.
British biochemists, though, made a breakthrough. First, they found the one peptide (4554W) out of almost 210,000 that had the best results “inhibiting αS from aggregating into toxic disease forms.” Then, because humans love to do Nature one better, they tweaked this one peptide to make it better, stronger, faster.
The new version of the molecule — 4654W(N6A) — contains two modifications to the parental amino-acid sequence and has proven to be significantly more effective than its predecessor at reducing αS misfolding, aggregation and toxicity.
It’s not a treatment, of course, but it’s potentially a big step.
* Horrifically oversimplified, I know.
Resistance victory
It’s bad news when carbapenems — the serious, last-resort antibiotics — don’t work. (Hence the word “last.”) But European researchers from a bunch of countries may have found a way to get them working again.
Bacteria learned to resist carbapenems by producing enzymes called MBLs that break down the drugs. So in the age-old tradition of an arms race, those biologists found a solution: They created a new type of enzyme blocker. It imitates the antibiotic, tricking those enzymes into binding with it, rather than with the antibiotic.
The potential new drugs in combination with carbapenems were found to be 5 times more potent at treating severe bacterial infections than carbapenems alone, and at a less concentrated dose.
That time to go green
“Living in greener areas may be beneficial against PMS symptoms.”
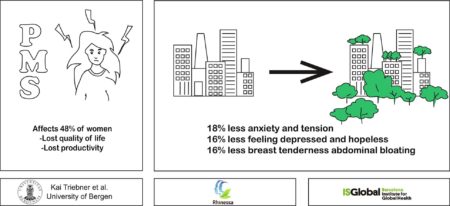
This is the actual illustration the researchers provided.


