Long Covid is sexist, second Covid is worse, the standing-on-one-leg test, and more
22 Jun 2022
Posted by Andrew Kantor
Are you likely to die within 10 years?
Stand on one leg. Go ahead — do it. Now hold it for 10 seconds. If you can’t, an international group of researchers has bad news for you:
An inability to stand on one leg for 10 seconds in middle to later life is linked to a near doubling in the risk of death from any cause within the next 10 years.
Empagliflozin and kidney stones: That’s funny
The most exciting phrase to hear in science, the one that heralds new discoveries, is not “Eureka!” but “That’s funny …” — Isaac Asimov
“Patients with type 2 diabetes who received empagliflozin were almost 40% less likely to have a kidney stone than patients who received placebo” — that’s what a Yale endocrinology researcher discovered after analyzing the data from 15,000 empagliflozin-receiving patients.
(Note: The article is just 900 words detailing how the data were collected.)
Covid quickies
Sexism in long Covid
Women are more likely to suffer from long Covid than men “and will experience substantially different symptoms.”
[F]emale patients were far more likely to experience mood disorders such as depression, ear, nose, and throat symptoms, musculoskeletal pain, and respiratory symptoms. Male patients, on the other hand, were more likely to suffer from renal disorders—those that affect the kidneys.
Once more, with worse feeling
You might think your second (blech) Covid infection would be milder than the first, what with your immune system better trained. But you’d be wrong. Researchers in St. Louis found the opposite is true, based on records from the VA database.
[C]ompared to people with first infection, people with reinfection exhibited increased risks of all-cause mortality, hospitalization, and several pre-specified outcomes.
And lest you think vaccination status matters*: “The risks were evident in subgroups including those who were unvaccinated, had 1 shot, or 2 or more shots prior to the second infection.”
* It does matter — it can keep you from getting sick in the first place. But if you’re unlucky enough to have two breakthroughs … ugh.
Too little (but not too late)
Some people who took Paxlovid were getting ‘rebound’ symptoms — there were plenty of anecdotes, although no solid proof yet. But UC San Diego infectious disease specialists think they know why it happens: The dose was too low.
[N]ot enough of the drug was getting to infected cells to stop all viral replication. They suggested this may be due to the drug being metabolized more quickly in some individuals or that the drug needs to be delivered over a longer treatment duration.
One-scan Alzheimer’s test
In case you haven’t noticed, artificial intelligence/machine learning is becoming a Very Big Deal in medicine. Computers see relationships we mere humans would miss.
Thus, thanks to well-trained AI, British researchers can diagnose Alzheimer’s with a single MRI, as opposed to the battery of tests currently done.
The researchers […] divided the brain into 115 regions and allocated 660 different features, such as size, shape, and texture, to assess each region. They then trained the algorithm to identify where changes to these features could accurately predict the existence of Alzheimer’s disease.
We meat-heads wouldn’t recognize that ‘smaller this + oval that + smoother the other thing’ means a chance of dementia, but the computer does — with 98 percent accuracy. And it can do it much sooner in the disease’s progression.
Captain Obvious can see clearly now
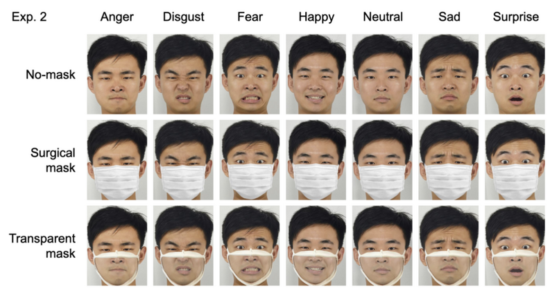
“Compared to a surgical face mask, it is most likely that […] transparent masks would allow for the better perception of facial expressions.”
Helpful image:
ICYMI: $3.6 billion here, $3.6 billion there — pretty soon you’re talking real money
If Medicare had bought its generic drugs from Mark Cuban’s Cost Plus Drug Company, rather than from drug makers, it could have saved $3.6 billion … just in 2020.
[T]he lower drug prices from a direct-to-consumer model highlight the inefficiencies in the current generic pharmaceutical distribution and reimbursement system composed of wholesalers, middlemen called pharmacy benefit managers, pharmacies and insurers.
Cannabis lowers insurance rates
If you want to know the actual effect of something on driving, where do you look? The insurance companies, of course. And that’s just what researchers at Temple University and the University of Arkansas did.
They actually examined insurance premiums in areas where marijuana was legalized; higher accidents would lead to higher premiums. In fact, they said, “We find that the legalization of medical cannabis leads to a decrease in auto insurance premiums on average of $22 per policy per year.”
Additionally, the team found that areas with relatively high drunk driving rates prior to the legalization of medical cannabis experienced large declines in their premiums following legalization. They estimate that policyholders in the states which legalized weed saved around $500 million in premiums.


