Nightmares and Parkinson’s, first convention photos, a gel for heart repair, and more
10 Jun 2022
Posted by Andrew Kantor
Reach for the sky
Pharma companies are setting the prices of their new drugs higher and higher. From 2008 through 2020, the average launch price of new drugs increased by more than 20% per year.
Meanwhile, the number of super-expensive drugs (costing more than $150,000 per year) increased by 9% from 2008 to 2013 … but 47% in 2020–21.
And despite what the drug makers say, the researchers (from Brigham and Women’s Hospital) found that patients are paying.
“[P]atients are not benefiting from [drug manufacturer] rebates and one in four report that out-of-pocket costs prevent them from taking their prescription drugs as prescribed.”
Convention opens!
The Georgia Pharmacy Convention opened yesterday with a full slate of sessions and events, dozens upon dozens of excited pharmacists, technicians, and students, and an address by Governor Kemp:

Photo: Catherine Daniel
By tradition, one seat in each session is left vacant for Elijah:

Photo: Catherine Daniel
Wildlife is abundant, as always:

Photos: William Huang
The Final Five from Thursday’s Draw Down voted to split the pot … and then donated it to the Georgia Pharmacy Foundation:

Photo: Teresa Tatum
Does shingles increase the risk of dementia?
No. In fact, the opposite is more likely. Looking at the records of 1.5 million older Danes*, researchers from Aarhus University “found that people with shingles had a 7% lower risk of dementia than people who did not have shingles.”
* Shifty, almost certainly
Unexpected Alzheimer’s danger
If you give a mouse a cookie, he might get fat. And if you give a mouse rapamycin, it might increase the amount of beta-amyloid protein plaque in his brain. That is not good.
University of Texas researchers expected to see the immunosuppressant (aka sirolimus) to reduce those plaques because there was evidence that it improved learning and memory. Instead, the opposite was true: Rapamycin reduced the amount of a protein called Trem2, which enables microglia to clear out the plaque. Less Trem2, more beta-amyloids — the hallmark of Alzheimer’s.
The good news is that the same research also found a way to increase Trem2 levels and clear out more plaque, but that research is just beginning.
And then there were four
An FDA panel has given its thumbs-up to Novavax’s non-mRNA Covid-19 vaccine for people 18 and over. If it gets approval from the FDA itself and the CDC, it would be the fourth approved vaccine in the U.S. The marketing tactic: It’s based on technology similar to the flu shot, so it can’t contain Bill Gates’s 5G-activated microchips.
It’s 90% effective against infection, and 100% effective against serious disease — how long the protection lasts isn’t known yet.
Building back the heart
After a heart attack, the heart doesn’t regenerate without outside assistance. One treatment is to inject it with cells that can (in theory) help rebuild it. But we say “in theory” because only a tiny percentage of those cells actually stick.
Enter researchers from Britain’s University of Manchester, who have found a way to make a lot more of those cells stay in place and do repair work. They’ve created a gel that can be injected directly into the beating heart; it acts as a scaffold for new tissue to grow on.
The result, they hope, could be a way to prevent heart attacks from becoming heart failure.
Better peptide delivery
University of Michigan pharmaceutical engineers have developed a new, less-expensive way to deliver time-release peptides. It works with more drugs, and it can reduce the time between injections.
Microencapsulation with a polymer — turning some injectable drugs into millions of tiny time-release capsules — isn’t new. But using it for some peptides is tough (i.e., expensive). But the U of M team has found a new way to encase drugs that’s easier and cheaper, works with more meds, and can release the payload over the course of almost two months.
“Give me the big science words!” I hear you say. No problem:
[The team] discovered that if they made the polymer first and equilibrated the peptide with the polymer microspheres in water under certain conditions, they could achieve a very similar result as the conventional organic-solvent based method of drug encapsulation.
Perchance to dream
Someone who starts having frequent bad dreams might be developing Parkinson’s.
Okay, that was the scary headline — lots of bad dreams means your risk of Parkinson’s is twice as high as people who don’t have bad dreams, according to British neurology researchers.
But the reality isn’t quite so bad. Yeah, “twice as high” is accurate, but it’s such a small number: 4.3% of people with bad dreams developed Parkinson’s, compared to 2.something percent of others.
So the takeaway is along the lines of, “If I suddenly start having a lot of bad dreams and have Parkinson’s in my family, maybe I should worry. Or maybe I should just take a break from the news.”
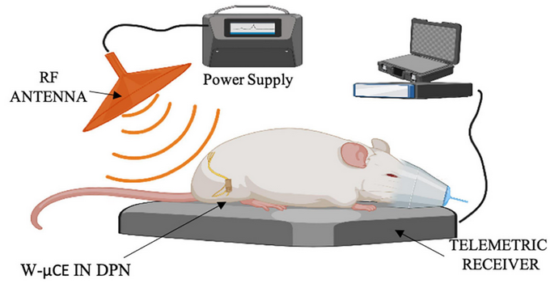
When drugs don’t work, bring in the electricity
Why take blood pressure meds when you can have an implanted nerve stimulator that zaps your body into compliance?
Biomedical engineers at the University of Houston have developed an implantable wireless device that stimulates the peroneal nerve, which “elicits an acute reduction in blood pressure.” And not a small reduction, either: “[S]ystolic blood pressure can be lowered 10% in one hour and 16% two hours after nerve stimulation.”
What’s next?
Further research is necessary to investigate whether BP regulation can be achieved chronically and whether continuous activation of the [deep peroneal nerve] is needed to maintain the beneficial effects of this bioelectronic treatment.
It’s either a science experiment or something from the next “50 Shades of Gray.”
Does apple cider vinegar help with weight loss?
No*. Shockingly, the stories on Facebook aren’t based on anything but wishful thinking.
* Or at best ‘probably not’.
It’s always something
Who do you think will complain about this year’s convention T-shirt more — flat-Earthers, or people who know that Ireland (and Iceland) exist?


