Poop tests, pricey Alzheimer’s drug (take 2), drug-pricing study debunked (Buzz-style), and more
29 Sep 2022
Posted by Andrew Kantor
Successful test, pricey drug for Alzheimer’s
A new drug, Eisai and Biogen’s lecanemab, was successful in a clinical trial, showing that it could slow the rate of patients’ cognitive decline from Alzheimer’s by 27%.
But, unlike Biogen’s last Alzheimer’s drug, Aduhelm, the lecanemab trial shows the drug does improve health outcomes (and the trial met the CMS diversity criteria). That means its approval would probably not have the controversy that Aduhelm’s did.
It also means that Eisai/Biogen could charge whatever it wanted, knowing that Medicare would have to pay it (remember, no price negotiating allowed). Eisai has said it values the drug at $10,400 to $38,053 per patient per year*.
Seniors who just learned their premiums were going down for 2023 might be in for a shock next year.
* About 6.5 million Americans over 65 with Alzheimer’s (source) x $10,400 per year = $67.6 billion a year
CDC relaxes healthcare-facility masking guidelines
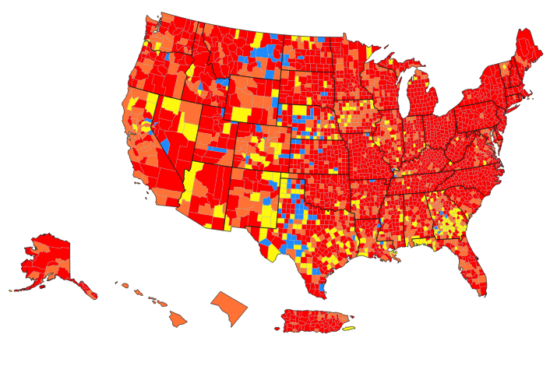
In areas where Covid isn’t spreading as fast — that’s a little more than a quarter of US counties — the CDC says staff at healthcare facilities can remove their masks when not working with patients, i.e., “when they are in well-defined areas that are restricted from patient access (e.g., staff meeting rooms).”
The good news: A bunch of Georgia counties fall into that 25%. (Click here for the interactive map.)
A fasting Alzheimer’s treatment?
Mice with Alzheimer’s can improve their cognition by changing to a fasting-mimicking diet — one “high in unsaturated fats and low in overall calories, protein, and carbohydrates” (basically providing only necessary nutrients for survival).
Mice on that diet, USC gerontologists found, “appeared to reduce inflammation and delay cognitive decline.” The researchers are also testing the diet on humans — right now just to make sure it’s safe.
Covid and point-of-care testing
An interesting outgrowth of the pandemic: more interest in at-home, point-of-care tests by both consumers and healthcare providers.
As one UMass researcher put it:
“Point of care was really a backwater for a long time. Now, having the Covid experience, everybody knows what an at-home test is and the benefits of being able to test themselves.”
We’ve gone from needing PoC tests because of Covid to wanting them “because health care is becoming more decentralized.”
Speaking of home testing…
Some people just aren’t good at doing those those colonoscopy alternatives — the fecal immunochemical tests (FITs) like ColoGuard that require patients to, um, collect a sample at home.
Specifically (say University of Iowa medical researchers), having less education, showing cognitive impairment, or — and there is no explanation for this — being female, are all associated with collection errors.
As much fun as it may be to speculate on the nature of these “errors,” most are actually clerical: waiting too long to collect a sample (so the test expires) or not labeling the sample correctly (e.g., leaving off the date).
Shameless plug
GPhA is offering the “NASPA Pharmacy-based Point-of-Care Test & Treat Certificate Program” on Sunday, October 2 from 8:30 am – 12:30 pm, at the GPhA classroom in Sandy Springs. There’s still (limited) space, so check it out at GPhA.org/pointofcare.
The full program — classroom and home study — is worth a whopping 20 hours of CPE!
Cool! We get to (sort of) debunk a med-pricing study
“Similar medications cost more for humans compared to pets” say medical researchers from the US and Canada.
They looked at 120 meds available for both humans and pets, and concluded that the discounted cash price for humans (from Costco) was higher than that for pets (based on a Google search) for 64% of them.
Sometimes, they said, humans without insurance paid 10 times more for the same meds, even with available discounts. Yikes!
But a quick and dirty GPhA Buzz check of cash prices* found at least some of those claims to be exaggerated.
- Lisinopril. The paper claims more than a 5-to-1 human/animal price difference. Buzz found it at 5 cents a tablet for pets and 12 cents a tablet for humans — only 2.4-to-1.
- Prednisolone. The paper claims it was almost 10 times more expensive for humans; we found it cost 21 cents a tablet (4mg) for humans, and 27 cents a tablet (5mg) for pets — hardly at 10:1 price ratio.
- Cyclobenzaprine. The paper claims humans pay 8 times as much. We found that 5mg cost 7.3 cents a pill for humans, and 5.9 cents a pill for dogs — again, hardly an 8-to-1 difference.
- Good ol’ doxycycline. The paper claims it’s more expensive for humans, but we found 100mg was 42 cents a tablet for dogs and 23 cents each for humans.
Big caveat: Veterinary-grade and human-grade meds can be of different quality, something the paper calls out. And, of course, most humans have insurance to help pay — something pharmaceutical companies are well aware of.
Still, using the same methods they did, we found vastly different results.
* At an unnamed national drug store compared to those at national pet-med chains
Covid this and that
Binge-drinking women are more susceptible
Ladies, listen up. Fun fact out of Rutgers: Women from 25–28 who have more than four drinks at a sitting “had the highest self-reported prevalence of COVID-19 infection.”
Cannabis use, ‘light’ drinking, smoking, or vaping — they didn’t have as much of an effect. But binge drinking made a difference (possibly because that means being “less vigilant in using preventive behaviors”).
It’s coming … whatever it is
Swiss researchers studying the evolution of SARS-CoV-2, are seeing it get better and better at skirting human immunity. And that, they say, means the future has plenty of Covid. Whether that means more hospitalizations and death … that’s impossible to say.
“We can say with certainty that something is coming. Probably multiple things are coming.”
J&J christens spinoff
Johnson & Johnson has named its consumer health spinoff “Kenvue.” It’s a combination of ken (the Scottish word for “know”), and vue (which sounds like “view”).
“You know it when you see it”



