Pseudo-drug under scrutiny, Georgia families’ court loss, big guns fight conspiracies, and more
07 Mar 2023
Posted by Andrew Kantor
Georgia families lose in lawsuit
A group of Georgia families hurt by opioid addiction lost their lawsuit against drug distributors Cardinal Health, McKesson Corp, and JM Smith. They had tried to use Georgia’s law designed to fight street-drug dealers against the drug distributors.
This was the first opioid lawsuit brought by individuals as opposed to municipalities.
Unlike those lawsuits, which accused companies of creating a public nuisance by failing to stem the flow of illegal opioids, the Georgia plaintiffs brought their claims under the state’s Drug Dealer Liability Act, which allows people injured by illegal drug use to sue dealers.
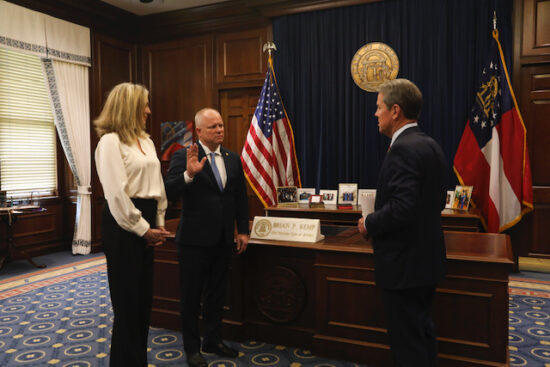
Farmer sworn in
A big GPhA congratulations to our past president Michael Farmer on his recent appointment to the Georgia Board of Pharmacy. Here’s a picture taken at the swearing-in ceremony:
A statin alternative
Patients who can’t take statins might have an option: bempedoic acid. It’s already used along with statins to reduce LDL cholesterol, but a new study out of the Cleveland Clinic found that, like Hamburger Helper, it works pretty well on its own.
Patients who received the bempedoic acid saw their LDL cholesterol drop by an average of 29.2 points by the end of the six-month trial.
After a 40-month follow up period, patients who had received the bempedoic acid saw a 19% reduction in the risk of needing cardiac revascularization and saw a 23% reduction in the risk of heart attack.
Most importantly, the patients didn’t have the muscle-pain issues that some statin users had.
It still doesn’t work
Why is phenylephrine still on the market? It was supposed to be a substitution for pseudoephedrine — one that could be bought without the ‘please don’t make meth’ hassle. Problem: As far back as 2006 it was found to be ineffective. (We wrote about that a year ago, in fact.)
But now it’s going beyond scientific papers; the FDA’s Nonprescription Drugs Advisory Committee “will weigh whether the agency should revoke oral phenylephrine’s classification as ‘Generally Recognized as Safe and Effective’ because it may be ineffective.”
Said one of the professors petitioning the FDA to un-approve phenylephrine:
“Let me be clear, oral phenylephrine is not a safety risk. It just doesn’t work.”
Or, as one 2022 article in Science put it, “The only reason it’s sold is to have some alternative to offer consumers, even if it’s a worthless one.”
But wait. There is a form of phenylephrine that might work: a nasal spray. That’s because it’s not destroyed by the digestive system the way the oral version is.
Med groups become misinfo warriors
A whole heck of a lot of medical groups — we won’t bother to list all 50, but it includes the AMA, the American Association of Colleges of Pharmacy, and the National Pharmaceutical Association — is tired of all the health misinformation out there (“gargle bleach,” “use dewormer,” “vaccines are dangerous,” and so on). They’ve banded together as the Coalition for Trust in Health & Science to fight that fake health news.
[A]ll member organizations will work towards ensuring that all patients can “have equitable access to and confidence in the accurate, understandable and relevant information necessary to make personally appropriate health decisions.”
First steps: “developing practical ways the coalition’s member organizations can work together to better disseminate reliable medical information and educate the public.”
Antipsychotics to boost antidepressants
Adding Abilify to an antidepressant for older people — those who aren’t responding to treatment — might be a good idea, at least according to Washington University psychiatric researchers.
When an antidepressant doesn’t work, the typical response is to try another … and another, hoping to find one that works. But the WU folks found…
Augmenting an antidepressant with aripiprazole helped 30% of patients with treatment-resistant depression, compared to only 20% who were switched to another solo antidepressant, results of the study show.
Caveats: Aripiprazole has behavioral side effects to watch for, like compulsive shopping.
And there may be some risk. A 2020 study found that, for adults diagnosed with depression who augment with a newer antipsychotic medication instead of a second antidepressant are at increased risk of dying — “augmentation with a newer antipsychotic was associated with a 45% relative increase in mortality risk,” the authors wrote.
Covid rebound is common
People who catch Covid sometimes rebound — i.e., get a repeat of symptoms a few days or weeks after they’re cured. A small study out of the Scripps Research Institute found that it happens whether or not they’re treated with Paxlovid (although it happens a little more often in those who were treated).
[T]he disappearance and then return of evidence of the virus on antigen tests and in self-reported COVID-19 symptoms occurred in 9.3% and 7.0% of patients who opted not to take antiviral treatment, and in 14.2% and 18.9% of those who opted for Paxlovid.
(While 9.3% vs 14.2% might seem like a big difference, they pointed out that in such a small study it was statistically insignificant.)
Short Takes
ICYMI: 20,000 exposed to measles
An unvaccinated person caught measles overseas and then attended a religious gathering — one with more than 20,000 people from around the world — in Kentucky. Hopefully everyone there was vaccinated. If not, we’ll probably be hearing about an outbreak soon enough.
Covid cases, deaths continue to decline
The US is down to an average of about 32,374 cases per week (i.e., 4,600 per day); Georgia is seeing an average of about 567 new cases a day (more than 600 are currently hospitalized), and the numbers continue to drop.
That said, 95 Georgians a week are still dying from Covid — more than 42,000 have died since the pandemic began.


