Immortal Israeli roundworms, OTC alternative, insulin’s cancer risk, and more
02 Aug 2022
Posted by Andrew Kantor
Unexpected insulin danger
Diabetics taking higher doses of insulin have a higher rate of cancer, especially if they’re insulin-resistant. Yeah, read that again. The findings, out of Ohio University, are based on health records of 1,300 patients over 28 years, so the increase can take a long time to appear. (And the it’s further muddied by the idea that having diabetes itself might raise the risk of cancer.)
Of note is that insulin-resistance. The epidemiologists who ran the study suggest that, to mitigate cancer risk, “improving insulin sensitivity may be preferred than simply increasing the insulin dose.”
Hutton is waiting
Is it time to renew your workers’ compensation or business liability insurance? Talk to Hutton Madden first: (404) 375-7209 or hutton.madden@phmic.com.
U.S. hits a positive milestone
The U.S. hit a new low for the number of uninsured people — only about 8 percent of Americans are now without some kind of medical coverage according to the latest CDC data (PDF). This is the lowest level in … well, in the modern, employee-based-healthcare era.
The bad news: A lot of people will be unable to afford coverage when this calendar year ends, because that will also end pandemic-related measures to help people pay for insurance. The good news is that Congress might vote to keep them in place, along with support for people in states that haven’t yet expanded Medicaid coverage.
A different anti-smoking tool?
For quite a while (i.e., more than 50 years), Asians and Eastern Europeans have been using cytisine as drug to help quit smoking; it’s a partial agonist against nicotinic acetylcholine receptors*, like Chantix (aka varenicline), but it’s “natural” in the sense that it’s a plant alkaloid.
Canada only just approved it a few years ago, but in most of the Western world it’s eclipsed by Chantix — in fact, my spell-checker recognizes varenicline but not cytisine. Why is that?
For one, previous studies found that while cytisine is better than placebo, it’s not quite as good as varenicline. For two, varenicline makes some companies a lot of money. But varenicline has issues (suicidal behavior, anyone?) so in 2018 the FDA approved a study of cytisine on our freedom-blessed shores.
So, does it work? The result is an rock-solid, unequivocal “It seems to, yeah”: “At the 12-month follow-up, the quit rate was 32.1% in the intervention arm and 7.3% in the control arm.”
One interesting note: The researchers who conducted the previous study suggest that “populations more accepting of ‘natural’ products would respond better to cytisine than to varenicline.”
* I think I got that grammar right.
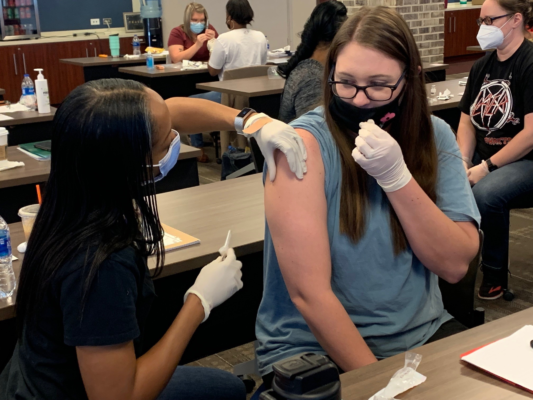
Techs: Get that immunization training!
It’s just three weeks away — GPhA’s Immunization Delivery Training for Pharmacy Technicians! In half a day — 3 hours at home, 3 hours in the classroom — you’ll score yourself 6.0 hours of CE, and be able to tell your boss that you are 100% ready to give immunizations.
With the coming Covid surge, monkeypox, and whatever else is on the schedule, you want to be ready. And GPhA will make sure you are.
Sign up now for the live training on Saturday, August 20 in Sandy Springs. Space is limited, so don’t wait! Click here for all the details and to register!
Did Israelis find the key to immortality?
If you have a roundworm (C. elegans) that you want to live forever, what’s the trick? One way: Improve its mitophagy — the mechanism for replacing worn-out mitochondria*. That mechanism, though, wears out with age, leading to a lot of dead mitochondria lying about, and thus unhealthy cells.
But now Israeli researchers say they’ve found a way to keep the mitophagy going strong, using molecules they created (“distinct designer diamines”) that …
… promote mitophagy, and thereby enhance healthspan in C. elegans and protect human cells against oxidative damage.
Naturally, they’ve already formed a company to try to turn the discovery into an actual drug. Eventually.
* All together now: “The powerhouse of the cell.”
Today’s potential Alzheimer’s cause
Could it be a “one-two punch” from the varicella zoster virus (VZV) ‘waking up’ the herpes simplex virus (HSV-1)?
Both viruses were known to maybe kinda sorta have a connection with Alzheimer’s, but now a collaboration between researchers at Oxford and Tufts universities found that individually they aren’t a danger but …
… exposing brain cells harboring dormant HSV-1 to VZV led to a reactivation of the herpesvirus and a cascade of the toxic plaques known to be signs of Alzheimer’s.
The fact that VZV can reactivate the herpes virus doesn’t mean that other viruses can’t do the same. The critical bit of info, they feel, is that reactivating dormant HSV-1 might be a trigger for Alzheimer’s disease, and that needs to be explored.
Between the rack and your counter space
Not many drugs have gone from prescription to over-the-counter lately, and here’s an interesting reason: The U.S. doesn’t have much of an “behind-the-counter” alternative, where customers must ask for a medication and (in theory) get advice or consultation with a pharmacist.
That might be changing, as the FDA considers a new rule called “Additional Condition for Nonprescription Use.” (Then again, the idea has been around for at least a decade, so don’t hold your breath.)
If the rule is approved, though, it could open the gateway to a lot more no-prescription-needed drugs, giving the FDA a way to split the difference when it comes to meds that seem almost safe enough to be on the rack, but not quite.
What’s the right amount of exercise to live longest?
The answer will keep changing as new studies come out, but the latest — courtesy of the American Heart Association, and based on “An analysis of physical activity and medical records for more than 100,000 people over 30 years” — says the answer is [insert drumroll here] …
… at least 300 minutes of moderate physical activity per week, or 150 minutes of vigorous activity.
“What?” you say, “That’s not what the headline reads.” True — the headline is the current guideline. What the story says is that there’s an increased benefit for doing two to four times that.
The reduction [in mortality] was 21-23% for people who engaged in two to four times the recommended amount of vigorous physical activity, and 26-31% for people who engaged in two to four times the recommended amount of moderate physical activity each week.



