Fake flu cures, CDC’s strep worries, quick Alzheimer’s test, and more
29 Dec 2022
Posted by Andrew Kantor
Alzheimer’s risk shift
“The #1 Risk Factor For Alzheimer’s Disease May Not Be What You Think” — unless you think it’s obesity. Then it is what you think.
What’s interesting, though, is that the top risk has changed over the past decade. It used to be “physical inactivity, followed by depression and smoking,” but obesity has taken over the top spot and shifted the others down as people change their habits, e.g., smoking less, exercising more … but still eating unhealthily.
(There are other factors, too, including hearing loss, “low educational attainment,” and of course a family history.)
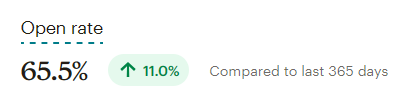
Our podcast experiment was a smashing success
After a poll showed a solid interest in a GPhA Buzz podcast, we debuted one a couple of weeks ago as a test. And after 11 episodes (and a bit of promotion here and in social media) we had zero interest. Literally — one person listened and no one subscribed.
Ah, well. That’s what experiments are for; nothing was lost beyond some time and the (small) cost of a better microphone stand. We get the message: Stick with text!
Even the insured have troubles
While the cost of healthcare is a huge problem for people without insurance, you might think that those with employer-sponsored healthcare are doing better. They’re certainly doing better, but they aren’t always doing well.
A new study out of NYU found that “In recent years, employer-sponsored health insurance has become less adequate in providing financial protection for all kinds of health care services.”
It’s especially true for women — “5.2% of women and 2.7% of men said prescription medications were unaffordable” — possibly due to a combination of lower wages and greater healthcare needs.
So keep this in mind when someone pulls out the GoodRx app, or asks for help with copay coupons or finding a cheaper med.
“People with health insurance coverage provided by employers generally think they are protected, but our findings show that health-related benefits have been eroding over time.”
Watch out for iGAS
The CDC is warning about signs of an uptick in cases of pediatric invasive group A streptococcal infections (iGAS).
Group A Streptococcus bacteria causes a range of infections, including acute pharyngitis (strep throat), scarlet fever, and other, more serious and life-threatening invasive infections.
Typically it appears in winter and early spring, but this year — for obvious reasons — the CDC would like to keep yet another respiratory infection at bay.
Elsewhere: Checking in with Ohio
The state is up to 82 infected children — including 32 in hospital — none of them fully vaccinated.
Oh, and 23 of the infected kids are under 1 year old, meaning they couldn’t yet get the vaccine. That means they were exposed to someone who was sick and not vaccinated. Anti-vaxxers, it seems, aren’t concerned if they infect others. As Forbes put it, “[D]deciding whether to get vaccinated is not simply a ‘personal choice’ as some adults may insist, but instead is an are-you-going-to-put-others-around-you-at-higher-risk? choice.”
So far, thankfully, no one has died. But, like Covid, there’s a risk of long-term effects of getting sick.
When long Covid isn’t long Covid
Covid-19, it seems, doesn’t like being over and done. Not only does it cause long Covid for a lot of folks, now there’s evidence that the virus also reactivates other, dormant viruses in patients leading to conditions like chronic fatigue syndrome. Especially chronic fatigue syndrome.
The idea is that, after Covid is gone, the body is left fighting off these newly-risen viruses — hence the fatigue part of chronic fatigue.
Keep in mind that there’s no clear definition of long Covid, and the wide variety of symptoms would make sense if “long Covid” was actually “old viruses come back to life.”
A blood test for Alzheimer’s
Until later stages, Alzheimer’s is a know-it-when-you-see-it condition until either an MRI or CT scan (or a lumbar puncture) can confirm the diagnosis. But now University of Pittsburgh researchers say they have a reliable blood test that can diagnose Alzheimer’s earlier.
They tested it in 600 patients at various stages of Alzheimer’s and found that levels of the protein correlated well with levels of tau in the [cerebrospinal fluid], and could reliably distinguish Alzheimer’s from other neurodegenerative diseases.
This is important not only for patient treatment, it make other kinds of clinical trials more reliable simply by knowing who has Alzheimer’s. First things first, though: Testing the test in more and varied patients.
FDA warns about flu “cures”
There’s no cure for the flu, and the FDA wants to remind people of that. Translation: Products that promise to cure the flu are, well, lying. The best we have is Tamiflu, which can reduce the duration, but that’s it — herbs, homeopathic products (i.e., water), nasal sprays, chakra aligners, sacrificial rites … no, they don’t work.
Fraudulent products also include some herbal teas, certain air filters and light therapies that claim to prevent or cure the flu, or treat symptoms, such as fever, muscle aches, and congestion.
That’s not to say these products are inherently bad, just that claims of treating the flu gives you an idea of how much you can trust them.