Watch out for meat allergies, Georgia’s students do good, don’t fall for aspirin, and more
29 Jul 2023
Posted by Andrew Kantor
Georgia students represent in biz-plan competition
A big shout out to the team from the UGA College of Pharmacy — it was named one of the three finalists for NCPA’s 2023 business plan competition*. Again. Because these kids are just that good.
But wait: The Mercer College of Pharmacy team may not have gotten to the final three, but it was in the top 10, showing these folks that Georgia student pharmacists are ready to kick butt and take names … and they didn’t bring their notebooks.
The UGA folks — along with teams from the University of South Carolina and the University of Texas at Austin –
– will present their business plans in a live competition on Oct. 14, 2023, at the NCPA Annual Convention in Orlando. The winning team will be announced on Oct. 15 as part of the convention’s first General Session.
The Mercer CoP team of Samuel Smith, Kaitlyn Moss, and Natalie Novak (not pictured: the UGA team)
* The 2023 Good Neighbor Pharmacy NCPA Pruitt-Schutte Student Business Plan Competition (GNPNPSSBPC)
Tick-bit allergy goes undiagnosed
You may have seen the news that cases are on the rise of alpha-gal syndrome (AGS) — where a tick bite causes an allergy to meat. As many as 450,000 Americans may have this nightmare condition, the CDC says.
Making matters worse is that a lot of healthcare providers aren’t aware of AGS, so they don’t even think to test for it when a patient has, um, let’s call it “non-insignificant gastro-intestinal distress” after eating meat.
So if one of your patients complains about severe abdominal pain after eating at Taco Bell, don’t dismiss it as “You and everyone else.” You might suggest a test for AGS.
Quadpill for BP saves money, too
Way back in 2021 we told you how Aussie researchers found that taking smaller doses of four different blood pressure meds was more effective than trying one after the other.
Now a different group of Aussies crunched the numbers and found that a so-called quadpill was also cost-effective.
The research team modelled the costs and benefits of lifetime treatment, including estimates of costs of medications and of predicted cardiovascular events in both groups. They found a quadpill would likely be cost effective to the Australian health system within a range of scenarios and for different kinds of patients.
Another anti-OD drug goes OTC
The FDA has approved Harm Reduction Therapeutics’ RiVive for over-the-counter sale, making it the second opioid overdose reversal drug to go OTC after Narcan.
Harm Reduction said it anticipates that RiVive will be available early next year, primarily to harm-reduction organizations and state governments. The not-for-profit drugmaker said it would make at least 200,000 doses available for free.
A ‘conversation’ to treat chronic pain
Scientists know that one of the causes of chronic pain involves a sodium ion channel called NaV1.7. When that channel is opened too far and more sodium gets through, the pain is worse.
Old idea: Block the channel to stop the pain. That, unfortunately, hasn’t worked.
New idea out of NYU: Instead of targeting NaV1.7 directly, talk to its friend — a protein called CRMP2. It seems that CRMP2 “talks” to NaV1.7 and regulates it. Then they dug deeper and figured out just how the protein does that talking.
With that figured out, they created a simple peptide to send the same message to NaV1.7: “Shut up and stop causing pain.” And then they engineered a virus to deliver that peptide. And what do you know: pain-free mice.
Not just mice. They’ve tested the virus on other rodents and even primates (it worked), so human testing could be around the corner.
When low-dose aspirin causes more harm than good
The latest blow against low-dose aspirin (for people who don’t have cardiovascular issues) comes out of a US-Australian study of more than 19,000 adults. It seems that taking it can increase a patient’s risk of brain bleeding if they suffer a stroke or head trauma.
It’s a significant risk, too — we’re talking a “38% increase in intracranial bleeding” after a stroke or intracerebral hemorrhage, and without providing any benefit.
These findings suggest that low-dose aspirin may have no role for the primary prevention of stroke and that caution should be taken with use of aspirin in older persons prone to head trauma (eg, from falls).
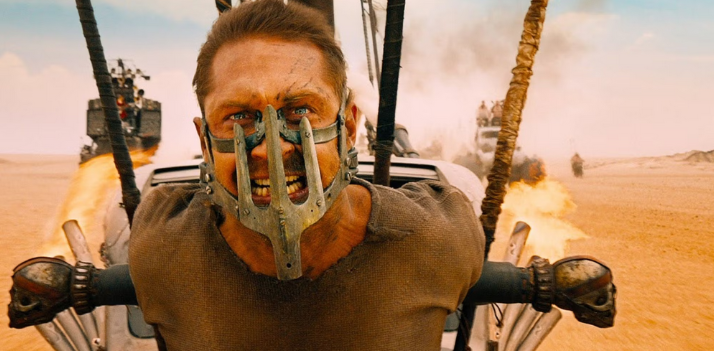
Not creepy at all
Apparently Duke researchers have watched “Mad Max: Fury Road” a few too many times. Their idea: Attaching the circulatory system of young mice to their elders, which turns out to “[slow] the aging process at the cellular level and lengthens the lifespan of the older animal by up to 10%.”
[A] team led by Duke Health researchers found that the longer the animals shared circulation, the longer the anti-aging benefits lasted once the two were no longer connected.