Why yellow snow is yellow, resurrecting insulin cells, a vaccine for acne, and more
09 Jan 2024
Posted by Andrew Kantor
Acne vax?
If you have a mouse with acne, you know how embarrassing it is for the little guy. The good news is that UC San Diego researchers have created a vaccine that reduces the inflammation of mouse acne, allowing Mickey and Minnie to feel a lot less self-conscious on prom night.
We all have the Cutibacterium acnes bacteria on our faces, and it all produces an enzyme called hyaluronidase. While the friendly version of C. acnes produces hyaluronidase A, its evil, acne-causing cousin produces hyaluronidase B, and it’s HylB that causes inflammation.
So the UCSD folks developed a vaccine that helps mice’s bodies neutralize just that HylB, while leaving the “good” bacteria intact.
“[W]e can now have more directed and effective anti-acne therapies while preserving the healthy skin microbiome, and that is a significant advancement in acne therapy.”
STOP, take a moment, and nominate a pharmacy pro for a GPhA award
Who’s the best pharmacist you ever saw? How about technician? Or a student deserving recognition?
You only have until January 19 to tell us — to nominate them for one, two, or more 2024 GPhA awards that’ll be presented at the 2024 Georgia Pharmacy Convention on Amelia Island.
If you think, “No way he’ll win,” don’t be so sure — let the awards committee decide! It takes just a few minutes to describe why someone is deserving, and you (and they!) might be surprised.
Head over to GPhA.org/awards and tell us about someone special!
Want a little AI help writing something?
Head over to chat.openai.com and create a free account (it takes seconds). Then try this prompt for ChatGPT:
I want to nominate someone for a pharmacy award called the [award name] given by the Georgia Pharmacy Association. Please help me write a 300-word explanation of why they deserve it. Here is the description of the award: [paste description from GPhA.org/awards here].
The person is [name] and they’re a [title at pharmacy or school]. Here are a few phrases I would use to describe them:
[Type in a few sentences]
Then let the AI do the work — just be sure to read over the response and make any edits. You’re welcome!
Respiratory virus updates
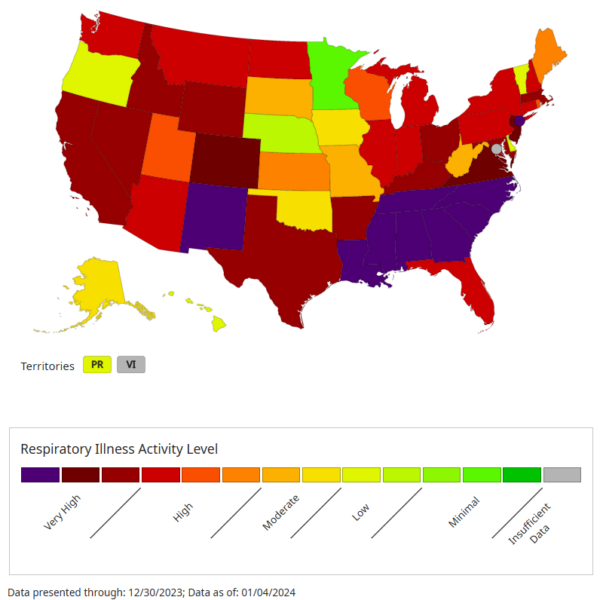
Georgia among hardest hit
Georgia’s flu levels are “very high” according to the DPH, and more than 1 of 10 doctor visits is now for a respiratory problem. It was only about 7.6% last week, and it’s also higher than at the same time in the last three Januaries.
Covid hospitalizations are also up (but not as bad as the last couple of years), and continuing to rise. The only bit of good news is that RSV cases are declining. Yay.
Covid vax data
The latest data on the latest Covid vaccines show that they’re about 71% effective in keeping older people (60+) out of hospital. That figure comes out of the Netherlands, but — aside from their odd language — Dutch people are very similar to Americans.
Interesting tidbit: This is actually a bit better than the last round of vaccines, which were only about 64% effective against hospitalization.
Elsewhere: Masks are back
Some hospitals in California, Illinois, Massachusetts, North Carolina, Pennsylvania, Washington and Wisconsin have reinstated face-masking requirements in light of the surge of respiratory illnesses. Which makes so much sense it shouldn’t be news, but here we are.
The requirements vary — e.g., some require them for all patients, visitors, and staff, while others only require them in certain situations, like when interacting with patients.
As one health official put it, it’s not just about the patients:
“What we don’t want is staffing shortages, right? When we saw the omicron wave in 2022, the biggest issues were not only people getting sick, but that we had a lot of frontline health workers, they were out with Covid.”
Interesting tidbit: None of those states are among those with the highest level of respiratory virus activity:
One Paxlovid question answered
Paxlovid — when taken quickly — can stop Covid-19 from getting worse, but it has limitations. For one, it can actually increase the risk of “Covid rebound” (we wrote about this in November). Now UC San Francisco researchers found that it doesn’t reduce the risk of long Covid.
So Paxlovid is good for one thing: Keeping people from getting really sick or being hospitalized.
Beta cell resurrection
When the immune system attacks pancreatic beta cells it leads to type 1 diabetes; the injured or dead cells can’t produce insulin. One research path focuses on replacing those dead cells or growing new ones.
But what if they weren’t dead dead, but only mostly dead? Could they be brought back to life?
Why yes, yes they could, at least according to Aussie researchers. They found a technique for “regenerating damaged pancreatic cells so they can produce insulin and functionally respond to blood glucose levels.”
Yep, they brought the beta cells back to life. In fact their technique — which uses two existing EZH2 inhibitors (cancer treatments) — can “reprogram” pancreatic cells so they return to their progenitor state. It’s less like bringing grandpa back to life, and more like making him a kid again. And it worked:
After 48 hours of stimulation with the drugs, the reprogrammed cells produced and secreted insulin in response to a physiological glucose challenge.
Although they tested this on humans, it’s still in the preclinical stage. They’re hoping it can become the first treatment for type 1 diabetes that actually treats the disease itself rather than just the symptoms.
You can sleep easy now
Like most people, you’ve probably laid in bed wondering “Why is pee yellow?” Fun fact: No one knew … till now.
A shout out to molecular biologists at the University of Maryland who took the time to figure it out. In short:
Red blood cells die, releasing an orange pigment called bilirubin, which ends up in the gut. There it’s broken down into urobilinogen, which is colorless. And then the magic happens: “Urobilinogen then spontaneously degrades into a molecule called urobilin,” which happens to be “buttery yellow*.”
They hope this discovery not only makes for fun last items in newsletters, but might open avenues of research into conditions like jaundice.
“Our team is excited to be able to explain it,” said the lead researcher, who is undoubtedly a hit at parties.
* The most disturbing use of “buttery” we’ve ever heard.


