Who should drink carbon monoxide, the combo that fattens kids, tough love for opioid prescribers, and more
18 Jan 2024
Posted by Andrew Kantor
How to cut opioid prescribing
Here’s one way to nudge doctors to be careful how they prescribe opioids: Send them a letter every time one of their patients dies from an opioid overdose, and — and this is important — include “a plan for what to do during subsequent patient visits.”
USC researchers already knew that a letter informing prescribers about the death of a patient was effective in cutting prescriptions, but now they found it’s even better to give some advice, too. (Kind of like telling a child, “Don’t give the new puppy a chocolate bar. Give him a dog cookie instead.”)
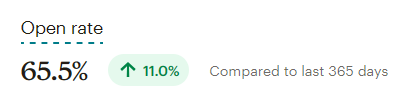
Compared to just a notification…
… physicians who received notifications with additional planning guidance reduced prescriptions of opioids by nearly 13%. They also reduced prescriptions of the anxiety medications benzodiazepines by more than 8%.
(Side note: You know you can trust the research because the lead author is Doctor Doctor.)
Speaking of opioid use…
Medical University of South Carolina medical researchers found that giving spinal surgery patients a dose of N-acetylcysteine (NAC) during surgery reduced their need for post-surgery opioids.
In the 48 hours after surgery, patients who were administered NAC via IV infusion received 19% fewer opioid doses on average than patients who received saline.
They had less pain, too, and waited longer to request pain meds. Side note: Some early studies have shown the NAC can keep heroin addicts from relapsing. “Can we stop giving opiates completely?” asked the lead researcher. “Likely not. Can we decrease the amount patients need? We should try.”
Gabapentinoids and COPD don’t mix
If you have patients with COPD, they shouldn’t be taking gabapentinoids. Drugs like gabapentin and pregabalin already have a warning about the potential for severe breathing difficulties, but there wasn’t a study on the effects on patients with COPD.
Now there is.
Researchers at Canada’s McGill University combed through the patient data of more than 13,500 patients with COPD and found that gabapentinoid use was associated with almost a 40% increase in “severe COPD exacerbation.” Notably, problems surfaced on average about 6 months after beginning gabapentinoid treatment, so the association might not come to mind.
Last chance to submit a nomination!
This coming Friday, January 19, is the deadline for submitting nominations for the 2024 Georgia Pharmacy Association Awards.

You have two days to tell us who’s the best pharmacist, technician, or student you’ve ever met. Nominate someone for one, two, or more awards that’ll be presented at the convention on Amelia Island.
You haven’t waited too long … yet. It takes just a few minutes to describe why someone is deserving, so please take a few minutes and tell us about that awesome pharmacy pro!
Unexpected cancer-drug booster
University of Iowa biomedical engineers found a surprising thing: Smokers did better on autophagy-inhibitor cancer treatment than non-smokers did. Huh.
What was one difference between the two? Carbon monoxide; smokers have a lot more of it in their systems. “[T]his suggested that elevated carbon monoxide might improve the effectiveness of autophagy inhibitors.”
So how can they deliver carbon monoxide to test their idea? Sticking mice into an exhaust pipe from a ’72 VW Beetle is one way, but a cooler idea is to concoct a drinkable, gas-entrapping foam where the trapped gas is carbon monoxide. (They went with plan B.)
When mice with pancreatic and prostate cancers were fed the carbon monoxide foam and simultaneously treated with an autophagy inhibitor, tumor growth and progression was significantly reduced in the animals.
It also worked on human cancer cells in the lab, so maybe “safe, therapeutic levels of CO” can be given to patients taking autophagy inhibitors — via a foam or a few hours on I-85.
Quickie flu update
Flu activity dropped a bit for the first time in a while, according to the CDC. It might be a one-week blip or — hopefully — a sign that the season is finally fading.
Kids are all about weight loss (and that’s bad)
The disturbing news: 13% of kids (especially girls) have tried a nonprescription drug or supplement for weight loss, and the percentage has been going up over the years.
The kids have been using whatever they can — diet pills, laxatives, and diuretics, none of which is good for them (unless, you know, they actually need them). “Not good for them” meaning that using these products actually leads to “low self-esteem, depression, poor nutritional intake, and substance use.”
Do we need to explain why they’re doing this? Fine. It’s a combination, say the Aussie researchers who did the study, of …
”. . . low self-esteem, parental influence to lose weight or parental dissatisfaction with weight, self-body dissatisfaction, peer groups who value thinness, and media or social media influences promoting unrealistic beauty standards.”
Oh, social media, what haven’t you done for us?
Guts, bacteria, fats, and kids
Antibiotics, it seems, can lead to little kids turning into, shall we say, ‘larger kids.’ Actually it’s a combo of antibiotics and a high-fat diet. If young kids are exposed to both, they run a greater risk of obesity, adiposity, and metabolic dysfunction.
The reason, found Vanderbilt University microbiologists, is good ol’ gut bacteria — specifically, the phenyllactic acid that one Lactobacillus bacteria produces. Phenyllactic acid normally tells the epithelial cells of the intestine to ease up on packaging and secreting fat, but when the bacteria aren’t there to produce it, more fat enters circulation.
So could you give kids some phenyllactic acid or Lactobacillus bacteria when they get antibiotics? Maybe. But that, as you can imagine, will require some more research.