Drug delivery by smartphone, ice water vs menopause, boosting prostate cancer chemo, and more
30 Jan 2024
Posted by Andrew Kantor
Icy water for hot flashes
Women dealing with menopause might consider taking the Polar Bear Challenge. That is, swimming in cold water seems to help with a bunch of typical menopause symptoms. That’s based on a survey of more than 1,100 women by British researchers.

The findings showed that menopausal women experienced a significant improvement in anxiety (as reported by 46.9% of the women), mood swings (34.5%), low mood (31.1%) and hot flushes (30.3%) as a result of cold water swimming.
The big big caveat: The survey was online and by women who already cold-water swim, so they’re a lot more likely to report their symptoms easing. Still, you might still suggest that someone take a jump in a lake. (Perhaps with different wording, though.)
Legislative update
The 2024 Georgia legislative session is moving along, and Melissa Reybold is there. Her latest update covers two bills in particular where GPhA has a horse in the race: One concerns white bagging/brown bagging, while the other covers the idea of selling opioid antagonists via vending machines. Read the details right here.
Ketamine ain’t esketamine
Ketamine’s been in the news a lot as a potential treatment for depression, PTSD, and more. It’s not FDA-approved (yet), but its cousin esketamine is approved for treating some forms of depression.
That gets confusing, especially among lay people who don’t realize how important those extra two letters are. (Consider how you’d feel if you landed in Kansas instead of Arkansas, especially during tornado season.)
Luckily, the good folks at Medscape have a great overview of the differences between ketamine and esketamine, including how they’re delivered, what they’re approved for, and the issues popping up as clinics offer “treatment” that could be ineffective, dangerous, or somewhere in between.
While ketamine and esketamine are chemically related, they are very distinct in terms of their chemical compositions, the FDA-approved indications, dosing, and administration, as well as the level of study and data supporting their safe and effective use.
Death confusion
What’s the leading cause of death in the US? If you said “heart disease,” congrats! You’re correct … and you’re in the minority. More than half of Americans didn’t know that, either assuming it was cancer, saying they didn’t know, or picking something else like terrorism, lung disease, exposure to 5G/microchips, or Jewish Space Lasers.
That’s from a Harris poll commissioned by the American Heart Association, which, as you might imagine, is trying to raise awareness of heart disease.
Prostate cancer updates
Boosting chemo
People with advanced prostate cancer are often given chemotherapy with docetaxel, but after about six months cancer cells can become resistant. What might overcome that resistance? Dicyclomine, the treatment for irritable bowel syndrome.
Researchers at Washington State University found that dicyclomine can block a protein on cancer cells called CHRM1. Without CHRM1’s help the cancer loses its resistance, then docetaxel can get back to work.
“The effect was pretty dramatic in all the experimental models we tested. And because dicyclomine already has a clinical use, this work has immediate translational potential.”
Not only can dicyclomine help docetaxel keep working, it can also allow it to be given in lower dosages, avoiding some of the side effects of chemo.
Go big or go home
When a prostate cancer patient’s PSA suddenly jumps, that usually means it’s time for hormone treatment to lower testosterone. That’s a good idea, found UC San Francisco scientists — but don’t hold back. Hit the patient with multiple testosterone-blockers and you’ll see better results.
Compared to the prostate cancer patients who only received a single drug therapy during their year of treatment, patients who received either one or two additional drugs stayed cancer-free, with low PSA levels, for longer.
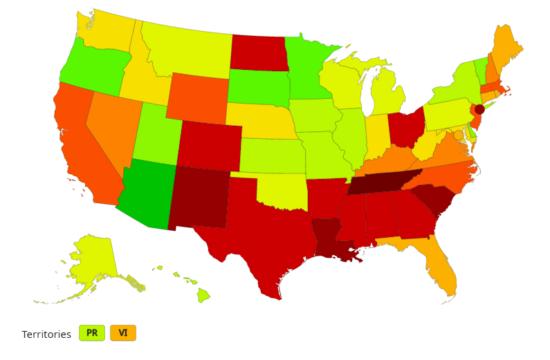
Respiratory virus season is easing
Positive tests for flu, Covid-19, and RSV are dropping, but there’s still plenty going around. (Just ask the Georgia General Assembly — if you read Melissa Reybold’s update, you know that Covid is causing legislators to reschedule meetings.)
The latest CDC data shows Georgia is still seeing high rates of respiratory illnesses (10 on a sale of 1-13) but the numbers are down from their end-of-2023 peak.
The X-for-Y Files: Cancer drug for kidney cysts
MIT and Yale researchers have found that drugs called 11beta compounds (which are being tested against cancer) also work against the kidney cysts that develop in certain kidney diseases. That’s because both tumor cells and kidney cysts are particularly susceptible* to oxidative stress and those 11beta compounds push that stress past the breaking point.
Tumor cells and kidney cyst cells tend to produce increased levels of free radicals because of the oxidative stress they’re under. When these cells are treated with 11beta compounds, the extra oxidative stress […] pushes the cells over the edge.
The treatment actually hits the sweet spot of oxidative stress, adding enough to kill the tumor or cysts but not enough to do damage to healthy cells. “The results also suggest that in patients, treatment with 11beta compounds once every few months, or even once a year, could significantly delay disease progression.”
* I just wanted to say that I spelled this right on my first try, which surprised me.
A smartphone-based drug patch
Imagine a world where people wore Band-Aid-sized patches on their arms that could deliver whatever meds they needed on demand via microneedles. Then imagine that med delivery could be controlled by a smartphone or computer. Need a painkiller? Boop-beep-boop and you’ve got it. Insulin? Beep-boop-beep, done.
That’s the vision researchers at UNC are working towards, with just such a patch they’ve tested on mice (with melatonin) and think “could be the next frontier in treatment of neurodegenerative disorders and neurological injuries.”
Even better, because drug delivery would be controlled by computer or smartphone, murder-mystery writers would have a field day with the possibilities of hacking someone’s device. Win-win!


