New heart guidelines questioned, GLP1s are back(ish), easy colon-cancer prevention, and more
06 Aug 2024
Posted by Andrew Kantor
Lilly’s GLP-1s out of shortage (sort of)
On Saturday we told you that one of Lilly’s two tirzepatide products, Zepbound, was expected to come out of shortage. Now the FDA says that both of them — Zepbound and Mounjaro — are available. They’re both still listed as in shortage, though, because the agency needs to consider the demand and how much of a backlog the company faces.
Look up a shortage
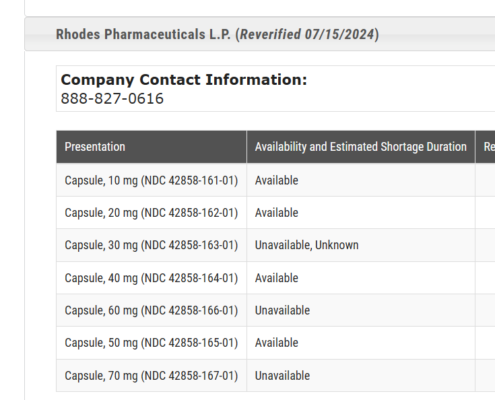
Did you know you can (easily!) search the FDA’s drug-shortages database? Just enter the generic name for a drug and you can see the different formulations and manufacturers, why they’re in shortage, and when they’re expected to be back, if the agency knows. (Sadly, it often doesn’t know.)
Check out the database: https://www.accessdata.fda.gov/scripts/drugshortages/default.cfm.
Interestingly, a drug like lisdexamfetamine might be in shortage, but some manufacturers, like Rhodes Pharmaceuticals, still have some forms available — you just have to scroll down the list.
Aspirin vs colon cancer
Regular aspirin use can reduce your risk of colorectal cancer — something that’s particularly important these days, when the disease is (mysteriously) rising among younger people.
That’s what Harvard researchers found after analyzing “three decades’ worth of data collected from 100,000 health care workers.”
[A]spirin was associated with a one-third drop in colon cancer risk among those with a low “healthy lifestyle score” [which includes] regular tobacco and alcohol use, the lack of a healthy diet, a lack of exercise, and a high body mass index.
Yes, aspirin has some dangers, notably the risk of GI bleeding, so there’s no one-size-fits-all for taking it. But when it comes to whether and how much to take, there are more factors to consider than heart risk.
RSV season is starting
It’s time to encourage your unvaccinated senior patients to get their shots before the season gets into full swing.
Florida, with its humid weather, is the nation’s ground zero for RSV. Each year, infections typically start in Florida and the Southeast before spreading to other parts of the United States, according to the University of Florida’s Emerging Pathogens Institute.
The road to myocardial infarction is paved with good intentions
Last year, the American Heart Association and American College of Cardiology released new guidelines for determining whether someone should start on statin therapy. Called PREVENT (Predicting Risk of cardiovascular disease EVENTs), it’s supposed to calculate whether someone should start on statin or blood pressure therapy based on their risk profile.
But there might be a problem with PREVENT. A study out of Harvard Med calculated that using it instead of older guidelines* called PCEs would mean a lot fewer people taking statins and a lot fewer taking antihypertensive meds.
And that, they say, would lead to “107,000 additional instances of myocardial infarction (MI) or stroke over 10 years.”
That said, both the AHA and ACC guidelines say that medication is recommended for anyone who shows a high risk based on either PCE or PREVENT scores. I.e., the new guidelines aren’t meant to replace the old ones, just to supplement them.
* Pooled cohort equations, which date back to 2013
Pharma will survive
Drug companies have claimed, over and over, that if they have to negotiate the price of their drugs, the world will end innovation will end and patients will suffer, yada yada yada. In reality, they spend more on marketing, stockholder dividends, and executive pay than on research.
Two new analyses out of Bentley University found a couple of tidbits that show how wrong these arguments are. First, the researchers found that drug prices don’t influence investment in biotech companies. Second, pharma companies pay for their R&D from their own investments, not from drug sales.
But even in a worst-case scenario, all pharma companies need to do is what they have been doing: Let other companies (or universities) do the initial research, then use their R&D budgets for late-stage product development. In that case, “According to the analysis, even a drastic 10% drop in global revenue would hardly impact the number of drug approvals.”
Fighting flesh-eaters
If you’ve ever gone swimming in a lake or the ocean near Florida, you’ve probably thought about flesh-eating bacteria. It’s out there. Waiting.
Luckily there’s some good news out of Washington University School of Medicine in St. Louis: Scientists there have developed what they say is a compound that can kill the kind of gram-positive bacteria that causes necrotizing soft-tissue infections like the flesh-eating disease that keeps popping up in Florida. (It also kills C. difficile, enterococci, staphylococci, and streptococci.)


