Syphilis test limitations, Covid/flu shot fails trial, healing with electric bandages, and more
20 Aug 2024
Posted by Andrew Kantor
Combo shot setback
Several companies are working on a combination flu/Covid-19 vaccine, but now another candidate seems out of the running. The Pfizer/BioNTech shot worked great against Covid and influenza A, but it failed to work against influenza B in a phase-3 trial.
CureVac and GSK had the same problem with their mRNA flu vax, as did Sanofi. Interestingly, though, both Pfizer and Moderna have separate mRNA flu vaccines that do seem to work against influenza B, but for whatever reason they can’t be combined with the Covid shot.
The companies are now back in the lab, thinking about what they’ve done.
Dues are due!
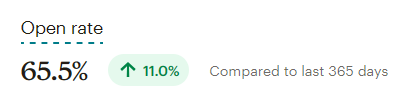
It’s that time of year — GPhA membership dues are up for renewal! Great news: As a part of our 150th anniversary next year, we’re extending membership benefits for an extra three months!
That means when you renew your membership by September 1, 2024, your membership won’t expire until December 31, 2025 — that’s three months of membership FREE. Zilch. Nada. Bupkis.
Not enough? How ’bout this: Dues are the same for 2024–25 — no increase.
Watch your email and snail mail for your renewal information and invoice. Or you can pop over to GPhA.org/renew to renew there.
We’re glad you’re a member, and we’re counting on you to continue being one, and to be a part of all of the celebrations in store to commemorate GPhA’s 150 years as the Voice of Pharmacy in Georgia!
File under: “Huh, that’s interesting”
Some people get Covid or the flu and barely notice, while some end up in hospital or even dying. It feels like a crapshoot, but that might not be the case.
A new Australian study looked at what the sickest people had in common. What they found is high levels of one enzyme called oleoyl-ACP-hydrolase — Olah to its friends — in the sickest patients. As one immunologist put it:
“[I]n some patients who develop life-threatening disease, Olah is produced at substantially higher levels, whereas we find very low levels in healthy individuals and patients with mild disease.”
What can be done with this info isn’t clear yet, but just finding the correlation is worthy of, as always, more research.
What to know about mpox
The current outbreak of mpox might be worth keeping an eye on. This clade (clade I) is a lot more infectious than the one that spread last time (clade II). Perhaps more importantly, it’s already been seen in at least a couple of patients outside of Africa — and authorities in Pakistan lost track of the one guy there.
Syphilis test reality check
You may have seen that the FDA has given approval to the first at-home test for syphilis, but what you may not have caught is the big caveat that comes with it.
The test won’t actually tell you if you have syphilis — it’ll tell you if you (probably) don’t have it. That’s because “positive test results from this test alone are not sufficient to diagnose syphilis infection and should be followed by additional laboratory testing.”
One big reason: “Results of this test will be positive for individuals previously diagnosed with syphilis, even if they were successfully treated.”
So it’s useless if you’ve ever had syphilis before. If it’s negative it means you’re probably okay. And if it’s positive it doesn’t mean you have syphilis, just that you need to get tested for real.
The Long Read: Gabapentin edition
Gabapentin is technically supposed to be used for seizures and diabetic nerve pain, but lately it’s being used for … well, for a lot of conditions, even if there’s hardly any evidence that it works. (And some older patients just keep taking it, even if they don’t remember why.)
The X for Y Files
You might think of ustekinumab as a psoriasis treatment, but a new British study found that it might also help children diagnosed with type-1 diabetes by protecting the function of pancreatic beta-cells and slowing the disease’s progression.
The science-y detail: “Ustekinumab was associated with a 49% higher C-peptide AUC at week 52 [vs placebo].”
Do androids dream of electric Band-Aids?
One way to help a chronic wound heal more quickly is to use an electric current, but that’s an expensive proposition. People with diabetes dealing with those are at risk of amputation. If only someone could create a cheap, disposable bandage that produced a small electric current.
Hearing that call were engineers at NC State*. They created a tiny, flexible, water-powered electrical wound dressing.
The dressing is applied to a patient so that the electrodes come into contact with the wound. A drop of water is then applied to the battery, activating it. Once activated, the bandage produces an electric field for several hours.
Because they’re flexible, they can fit over irregularly shaped wounds, and when tested on mice the bandages healed wounds 30% faster than regular dressings. And the cost? A couple of bucks apiece.
* As well as Columbia, Beth Israel Deaconess Medical Center, UNC, Georgia Tech, and Korean researchers