July 08, 2023 ✒ Andrew Kantor
Did you know that Merck found making Keytruda in the microgravity of Earth orbit made the drug more stable? That the space-built version could be given by a shot instead of infusion? Now you know. With the concept proven, a startup called Varda Space Industries has launched a test of the first space-based drug factory. During the satellite’s first week in space, Varda will focus on testing its systems to make sure everything works as hoped. The second week will be dedicated to heating and cooling the old HIV-AIDS drug ritonavir repeatedly to study how its particles crystalize in microgravity. It will return to Earth in about a month so the Vardians can see how well it performed and prepare to create a working factory. Cipla is recalling 6 batches of albuterol because of a leak found in an inhaler. Check its press release (PDF) for the list of batch numbers. You know how a drug is approved to treat one condition, then gets approved to treat more? Turns out that it’s less effective for each new condition it’s approved for. In a commentary about the research the found this, the head of the Institute for Quality and Efficiency in Health Care’s drug assessment department pointed out that, even though a drug’s added value declines, “the pharmaceutical industry often succeeds in obtaining such supplemental indications to optimize resource use and extend the period of patent protection for its drugs.” Perhaps, she suggests, we should focus more on whether an indication is better rather than just new: “The system’s current performance does not meet the expectations of patients and the public, clinicians, or policy makers.” It turns out that a lot of people didn’t gargle or drink bleach to prevent Covid — but they said they did. Back in 2020, a CDC survey found that 4% of people claimed “they were drinking or gargling diluted bleach to prevent a Covid-19 infection.” It was believable because it seems logical that 4% of people are imbeciles. But a follow-up study found a large number of “problematic respondents.” So how did they know these folks were less than truthful? “[W]e also observed that 3–7% of respondents reported having never used the Internet while taking the survey online and having suffered a fatal heart attack.” Yeah, a fatal heart attack tends to make it harder to answer surveys. Those shifty Danes at Novo Nordisk are suing more compounding pharmacies, this time in Florida and Tennessee. Claim: The pharmacies aren’t allowed to create compounded versions of Ozempic and Wegovy. Reality: FDA rules say that compounding is permitted for drugs in shortage, as semaglutide is. Claim: The FDA hasn’t approved these compounding medications. Reality: The FDA doesn’t approve compounded products, just their active ingredients. Semaglutide is FDA-approved. Claim: “[T]he pharmacies are making the products with an unauthorized version of their active ingredient, semaglutide.” Analogy: Someone is using McDonalds’ beef supplier to make their own burgers. Claim: More than a decade ago, a compounding pharmacy broke the law and people died. Analogy: The Danes once murdered and pillaged their way across Europe. The Novo Nordisk Board of Directors (artist’s conception) Curious about the differences between hepatitis A, B, C, D, and E? HealthDay’s got you covered. Arizona becomes the latest state to allow adults to purchase contraceptives over the counter at pharmacies after completing a brief screening including a blood pressure test. Previously it required a pharmacist’s prescription. That makes the total 19, including DC; only 9 require the patient to be 18 or older (per the Guttmacher Institute). After falling during the pandemic, tuberculosis cases have been rising again worldwide and in the US. In fact, “tuberculosis numbers have quickly climbed back up to pre-pandemic levels, marking the first time in decades that cases and deaths have risen globally.” Caveats: Some of that 2020 drop is due to less testing (or confusion with Covid), and some of the 2021 rise is due to better testing. Sillier than drinking bleach, space drugs get closer, indication overload, and more
Drugs … in … spaaaaaaaace

Albuterol recall
More uses, less usefulness
Who lies to look stupid?
Novo hates compounders

Learn your hepatitis ABCDEs
Short Takes
Elsewhere: OTC birth control in Arizona
Consumption resumption
July 07, 2023 ✒ Andrew Kantor
It’s safe to give kids stimulants for ADHD — well, safe in terms of their developing substance abuse issues later in life. This had been a concern, or at least a reason to hesitate prescribing the meds, but a study out of the University of Pittsburgh found there’s nothing to worry about. The Pitt researchers studied kids over 16 years (!) and found that the chance of a child treated with stimulants turning into a young adult with a drug problem was no greater than kids who didn’t have the meds. On the other hand, taking stimulants didn’t protect the kids from having a substance-abuse problem, either. Hoping to avoid another “tripledemic*” this fall, the feds are gearing up to make sure people can get the shots they need to keep their lungs working: for flu, Covid-19, and RSV. The flu shot is, well, the flu shot. The Covid vaccine will be tuned specifically to the most common XBB variant. And the newly minted RSV shot is particularly important for the youngest and the oldest patients. “The number of elders who die of viral infection every winter in our intensive care units, and also sometimes in the summer, is large — it’s in the tens of thousands of individuals. Each of these vaccines is a huge win.” Pro tip: It might be good to space the flu and RSV shots a few weeks apart. There’s some evidence they can interfere with each other. * The fact that it’s still in quotes is a good sign. When taxpayers pay to develop a drug, they should be getting a fair price for them. Thus a proposal from Sen. Bernie “the Angry Grandpa” Sanders, chair of the Senate Health, Education, Labor and Pensions Committee, that would limit what they could charge when the federal government paid for the research. The proposal would “mandate price caps for drugs that were developed with the help of government funding” by prohibiting them from exceeding “the lowest price charged for it in Canada, France, Germany, Italy, Japan, or the U.K.” Because the US doesn’t do any kind of cost-benefit analysis on the value of a drug (we just pay whatever the drug company feels like charging)… This move would essentially leave the U.S. price of government-developed drugs in the hands of regulators in Europe, who assess therapies by way of cost-benefit analysis. This system keeps prices in check, much more so than in the U.S. Drug companies and their champions call this “price setting,” as opposed to what they do which is setting the price. The FDA is poised to approve Eisai/Biogen’s treatment for Alzheimer’s, but it comes with a load of caveats. First is safety, as three people died during trials. Then there’s cost to patients and taxpayers; the companies are charging $26,000 per year. Then there’s the limited number of specialists who are qualified to determine if it’ll actually help. Finally, the testing involved very few Black patients, and Alzheimer’s seems to affect them differently. Blacks are up to twice as likely as whites to be diagnosed with Alzheimer’s, while showing equivalent levels of amyloid in most major studies. No one is sure why, but the hypothesis is that having multiple simultaneous health conditions and being exposed to environmental stressors put Blacks as a group at higher risk. While Leqembi can’t reverse the signs of dementia, but it at least “delayed cognitive decline by 27% over 18 months.” How much that will actually mean to patients in the real world isn’t clear. That’s why CMS said Medicare will cover the drug, but it will require prescribers “to collect and share data about the drug’s real-world performance.” When it comes to hypertension drugs, there’s no one size fits all. Finding the best med can mean a lot of trial and error. So Boston U researchers set a computer on the task, teaching it about previous patient outcomes so the AI can recommend a treatment more likely to work. In other words, instead of considering just the benefits and risks of various meds, the program “generates a custom hypertension prescription using an individual patient’s profile, giving physicians a list of suggested medications with an associated probability of success” based on how effective a med was with similar patients. The initial training database was big, too — medical records of almost 43,000 patients over 8 years. It seems to have paid off: The researchers found [the AI] achieved a 70.3 percent larger reduction in systolic blood pressure than standard of care and performed 7.08 percent better than the second best model. Slowly but surely, vaccines against Lyme disease are making their way through clinical testing. Valneva’s candidate just passed its phase 1 trial, showing that it’s safe, tolerated, and generally effective. Larger phase 2 trials will further test its effectiveness. The downside so far is that it seems to require an initial shot and a booster, and then gives about 6 months of protection. As Veterinarian of Buzz told us, Lyme-carrying ticks are around all year, even if they’re most active in summer.AI BP med chooser, should taxpayers pay twice, stimulants are safe, and more
Stimulants aren’t a gateway
Feds prep for fall vax campaigns
Give us a break — we paid for the research: Sanders
Alzheimer’s drug is almost here … but
Let the computer choose the med

Lyme vax continues its approach
July 06, 2023 ✒ Andrew Kantor
Chances are you’ve got female patients in the 12–21 range. Fun fact: There’s a good chance they’re iron deficient. A new multi-university study found that the CDC-recommendation of screening non-pregnant women every five to 10 years for anemia isn’t nearly enough. Anemia takes years of iron deficiency to build up. What they found is that among women who had hit puberty, “27.1% had iron deficiency when using the 25-μg/L ferritin level threshold,” but when you add in the younger ones it reaches 38.6% deficient. “Given the high prevalence of iron deficiency,” the authors wrote, “…current screening guidance may miss many individuals with iron deficiency.” Something bugging you about Georgia’s pharmacy’s legal landscape? Should something be outlawed or in-lawed? That’s what GPhA is all about! Each year, the GPhA Legislative Committee takes ideas submitted by members about what laws need to be enacted or changed, and that’s where our legislative priorities come from. It’s that time of year again. If there’s a law or policy issue you want to see changed — something that will improve patient care or the practice of pharmacy — tell us about it! E-mail a brief explanation of the issue to our VP of public policy, Melissa Reybold, at mreybold@gpha.org. Yes, it’s that simple — just give as much detail as you can about how it affects you. Oh, and do it by the deadline of Friday, July 21 at 5:00 pm. Time to change the world … or at least the state! Well look at the time! It’s time to take another look at whether legalizing cannabis has an effect on pain-med prescriptions. And the latest answer is [insert drum roll] … nope, legal pot (medical or recreational) doesn’t affect painkiller prescriptions for patients with chronic pain. See you in a few months for the next study! Did you happen to catch the story about the WHO deeming aspartame a carcinogen? That’s actually not what the announcement said at all, but that didn’t stop it from being reported that way. In fact, all the WHO did was move aspartame from unclassified to possibly carcinogenic — a catch-all category that just means the data don’t rule out the sweetener being unsafe. (The other two categories are probably carcinogenic and carcinogenic.) As one journalist put it, “It’s a bloated category, essentially one big epidemiological shruggie.” So before you think about giving up that sweet, sweet Diet Dr Pepper, check out “Being Alive Is Bad for Your Health,” which gives more detail about what the WHO really said. Whether you’re working or studying, Aussie researchers have proven that the anecdotal life hack of taking a five-minute break really does reset your brain. There is no need for a walk along a river, or a lengthy video of bamboo forests swaying in the wind (although that could be nice). A five-minute total break will do the trick. The important thing is that it has to be a real break — “unstructured,” as they put it. No computer or phone, no switching to another task. Turn your brain off. “[D]o some breathing or just sit quietly to rest your brain from the task.” The result will be better concentration and problem-solving when you get back on task. I won’t say anything if you don’t, but for patients with diabetes, getting a “prescription” for fresh produce — i.e., “which would provide free or discounted fruits and vegetables to eligible Americans living with diabetes” could save the current cohort of diabetic Americans $40 billion in medical bills by preventing cardiovascular problems. That’s the result of a Tufts University data analysis. But fruit and veg ain’t cheap — it would cost a bit more to pay for it (and administering a program). The net price would be about $18,000 per “quality-adjusted life year”: This is on par with other “best buys” in health care, like blood pressure screening and control, cholesterols screening and control, and cancer screening. (In comparison, the new GLP-1 weight loss medications cost about $200,000 per quality-adjusted life year gained). The headline reads “Being overweight may not be associated with early death,” but the details aren’t nearly as interesting. So no, you can’t just rush out to hit the Oreo aisle. What the Rutgers study found was that a high body-mass index by itself doesn’t mean you’re likely to die earlier. It’s the various problems with being overweight — diabetes, heart issues, etc. — that’ll do you in. (And there’s also the issue of BMI no longer considered a good indicator of obesity, raising the question of why they used it in the first place.) As one reader of the study put it, “The main hazard of overweight and moderate obesity is a three times greater risk of developing diabetes which contributes to cardiovascular disease, renal failure and blindness.” Five minutes for your brain, obesity-study confusion, aspartame reality check, and more
Girls need iron
It’s that time: What oughta be a law?
Cannabis laws and painkillers
Aspartame: What’s the real deal?
Take 5 for your brain

An ounce of (non-pharma) prevention
Why you need to read past the headline
July 04, 2023 ✒ Andrew Kantor
Georgia (and Florida) is the epicenter of a national outbreak of cyclosporiasis, probably from raw imported broccoli and other veggies. The worst part is that the main symptom is explosive diarrhea. It can take a week or two for the symptoms to appear (they also include “nausea, a loss of appetite, cramping, bloating, increased gas, and fatigue”). The treatment, luckily, is simple: trimethoprim/sulfamethoxazole, aka Cotrim. If a patient is allergic to sulfa drugs … well, there’s nothing to do but wait it out. [T]he CDC recommends that the “best way to prevent cyclosporiasis” is “avoiding food or water that may have been contaminated with feces.” That is important news if all along you’ve been seeking food or water contaminated with feces. More than 1.5 million Americans have been “disenrolled” from Medicaid since the end of June. The worst part: 71% of them were disenrolled for “procedural reasons,” not because they weren’t eligible. (Of those, 35% were children.) Procedural disenrollments are cases where people are disenrolled because they did not complete the renewal process and can occur when the state has outdated contact information or because the enrollee does not understand or otherwise does not complete renewal packets within a specific timeframe. In response to so many people losing coverage, the Biden administration has given states more options to slow the disenrollment flow, including allowing states an extra month “to conduct more targeted outreach to individuals” and — notably for Buzz readers — “allowing pharmacies and community-based organizations to reinstate coverage for some individuals disenrolled for procedural reasons.” Michigan is taking advantage of that offer and will pause disenrollments until the end of July while it works to help its citizens complete the paperwork. South Dakota became the 40th state to expand Medicaid under the Affordable Care Act; it will cover people earning $20,120 per year for an individual or $41,400 for a family of four. Australia has become the first country to legalize psychedelics to treat some mental health conditions: “MDMA to those suffering post-traumatic stress disorder and magic mushrooms for some types of depression.” It’s by prescription only and “Use of the psychedelics would be carefully monitored and not a case of ‘take a pill and go away’.” Bonus: Includes the phrase “game changer” twice. A blood condition called clonal hematopoiesis of indeterminate potential (CHIP) has an odd association: People who have it are significantly less likely to develop Alzheimer’s. Unfortunately, they’re also much more likely to develop blood cancers and heart conditions. CHIP is caused by a mutation in the bone marrow’s blood-producing cells. It results in mutant blood cells that outcompete normal ones. The twist is that some of those cells slip into the brain and can replace the brain’s immune cells — the microglia. Those are supposed to do trash pickup in the brain. So … could these mutant cells be boosting the microglia so they fight Alzheimer’s? You know the mantra: More research is needed. Sure, Americans want to lose weight, and we love an easy way to solve a problem. But when it comes to all those new weight-loss drugs, a poll shows there’s a limit to how much people are actually willing to spend. Ozempic, Mounjaro, Wegovy — they all cost big bucks, and many insurers aren’t covering them. With a list price of $900 to $1,600 per month, even with insurance that’s a lot of co-pay. It’s also co-pay that keeps on taking, because you can’t just use these drugs to hit a goal; you have to take them forever. “Can you really ‘address’ annoying eye floaters with a supplement?” No. Don’t be. They’ll do just fine.Explosive GI infections, Aussies legalize psychedelics, Medicaid changes coming, and more
The worst kind of outbreak
Medicaid news
Disenrollment troubles
Elsewhere
A trip down under
Blood mutation-Alzheimer’s connection
The cost of weight loss
Short Takes
Saving you a click
Worried about health insurance companies’ profits?
July 01, 2023 ✒ Andrew Kantor
Semaglutide: “I can help people lose 15% of their body weight!” Tirzepatide: “Pshaw! I can help them lose 21% of their body weight!” Retatrutide: “Hold my beer.” After 48 weeks, Eli Lilly’s new, still-in-phase-2-testing drug, retatrutide, led to an average weight loss of more than 24% — we’re talking 57.8 pounds (14,797 drams). How? By not just targeting GLP-1 (like semaglutide), and not just GLP-1 and GIP (like tirzepatide), but by targeting those two plus activating of glucagon receptors, which help regulate blood sugar. Next up: Four different phase-3 studies. In what’s not entirely a surprise, it turns out that higher doses of semaglutide do a better job helping with blood sugar and weight loss. [O]nce-daily oral semaglutide taken at 25 milligrams and 50 mg did a better job in lowering blood sugar levels and promoting weight loss than the lowest dose of 14 mg. Lots of people lose hair where they want to keep it, but sometimes you get hair where you don’t want it. Say, for example, on a hairy mole. It takes a special kind of person to look at such a hairy mole and think, “I wonder if the secret to treating hair loss lies within?” And yet that’s just what some UC Irvine researchers did … for a decade. All because they realized that some of those ugly moles — called nevi — can “induce luxurious hair growth.” Over some 10 years of work, the researchers identified a chemical released by a mole’s pigmented cells that “potently stimulates hair follicle stem cells for robust hair growth.” That molecule is osteopontin. […] The secreted osteopontin interacts with a molecule on the stem cells called CD44, apparently flipping the hair-growing switch to “gonzo.” Tests continue with a hope of creating, say, a biannual injection that would cause hair to pop out where it’s wanted — but sans the mole part. Bonus: Includes the phrase “game-changer.” You wouldn’t think there could be “An Unexpected Doorway into the Ear,” but here we are. And the good thing about this particular door is that it can be used (Rochester University researchers found) to “deliver a gene therapy that repairs inner ear hair cells [and] restore hearing in deaf mice.” Using gene therapy this way isn’t a new idea, but the problem was reaching the cochlea without surgery. But now with the cochlear aqueduct, they were able to do that, injecting a virus that carried a gene therapy into the inner ear. That therapy was able to fix the ear’s hair cells and restore hearing … to mice, at least. The EU has made a deal with Pfizer (and others) to reserve vaccine-making capacity for the next pandemic — whatever that pandemic might be. “The agreement covers mRNA, vector-based and protein-based vaccines [and] ensures that companies are ready to respond to a crisis by keeping their facilities up to date and monitoring their supply chains, ‘including stockpiling where necessary’.” mRNA vaccines work great, as we’ve learned, and are being used to treat other diseases, notably cancer. But they could be better. mRNA vaccines are very good at getting muscle cells to generate an antibody response, but what you really want is a longer-lasting T cell response. To do that you need to activate dendric cells — the ones that teach T cells to attack … well, whatever you want attacked. Muscles are low on those dendric cells, but the spleen has plenty, and now Johns Hopkins researchers have developed an intricate little nanoparticle wrapper for mRNA that that can find its way to the spleen where it “was taken up by primary dendritic cells at levels about fifty-fold higher than mRNA by itself.” This means they may have found a way to make mRNA vaccines more effective by creating not just antibodies, but (in this case) “an army of T-cells that can recognize cancer-linked antigen.” We can cure hepatitis C, and treating it is expensive. So why haven’t we ended it? The cost (at least in the US) is a big part, but it’s not the only issue. Read on, MacDuff. Israeli researchers found that adding a “natural” molecule called 3,3´-Diindolylmethane (bisindole to its friends) to toothpaste will kill the biofilms formed by bacteria that cause plaque and cavities, reducing it by 90%. “The molecule, which was found to have low toxicity, could be added to toothpastes and mouthwashes to greatly improve dental hygiene.” Not enough for you? Bisindole also has anti-cancer properties. No matter who wins the 2024 presidential election, pharmaceutical companies face and uphill battle. “There is no leading candidate that’s a friend of the pharmaceutical industry at this point. Not DeSantis, not Trump, not Biden.” Low-dose colchicine (LoDoCo, seriously) — the gout med — just got FDA approval “to be used in low dose to prevent cardiovascular events in patients with proven coronary disease.”Hairy mole goodness, hidden ear passages, yet another weight-loss drug, and more
The next next weight-loss drug
Speaking of weight-loss drugs…
We didn’t include a photo. You’re welcome.
A new path for gene therapy
Europe prepares for the next one
A better way to deliver mRNA
The Long Read: Why is hep C still a thing?
Short Takes
Toothpaste as bacteria killer
Dark future for PhRMA
Mo fo’ LoDoCo
June 30, 2023 ✒ Andrew Kantor
When OTC analgesics don’t work for acute back pain, low-dose, short-duration opioids are often the next step. But Aussie researchers found that they don’t work any better than placebos (and, of course, you kinda want to avoid opioids in general). In a study of more than 340 patients suffering from low back or neck pain, a team of Australian researchers found there was no difference in pain severity after six weeks between those who received opioids versus a placebo sugar pill. “It was quite a surprise to us. We thought there would be some pain relief, but overall there was no difference.” Possible downside: The research could convince prescribers not to give opioids when they can actually do good. It’s like this: A study by a group of those shifty Danes found that “Women in their 50s who took estrogen and progestin hormone replacement therapy for menopausal symptoms had an increased risk of dementia within 20 years.” The important bit: As experts point out, that probably means that women who were showing signs of dementia are the ones who sought out HRT. (One big reason is that the effect showed up within a year of beginning HRT — and that’s just “biologically implausible.”) There’s even an editorial with the paper titled, “A causal link remains unlikely.” But that didn’t stop CNN, and presumably other news outlets (including HealthDay News), to phrase it as “HRT use by younger women linked to dementia.” Because that’s more exciting than, “Women with signs of dementia during menopause likely to seek out hormone treatment.” Coming soon: “Aspirin use linked to headaches.” Can vitamin D supplements help prevent heart attacks? One headline for the story on vitamin D reads, “Vitamin D supplements may reduce risk of heart attacks in older adults”. Another dials it back with, “Mixed Results on Vitamin D’s Benefit for Aging Hearts.” But what did the authors of the actual paper have to say? Vitamin D supplementation might reduce the incidence of major cardiovascular events, although the absolute risk difference was small and the confidence interval was consistent with a null finding. (Emphasis ours.) There are often stories about the benefits of coffee, although the terms coffee and caffeine are sometimes (wrongly) used interchangeably; some of coffee’s benefits come from decaf as well. The latest twist comes out of Portugal, where researchers found that even coffee’s wakefulness effect is about more than just the caffeine. First, they found that (no surprise) drinking coffee or taking caffeine directly “made people more prepared to move from resting to working on tasks.” But here’s the cool bit: [D]rinking coffee also increased the connectivity in the higher visual network and the right executive control network – parts of the brain which are involved in working memory, cognitive control, and goal-directed behavior. This didn’t happen when participants only took caffeine. In other words, if you want to feel not just alert but ready to go, caffeine alone won’t do – you need to experience that cup of coffee. The drug maker has said it will “plant and maintain more than 50 million trees by the end of 2025,” and is already more than 20% to the goal with projects in Australia, France, Ghana, Indonesia, the UK, and the US. The maintain part is important. Lots of tree-planting efforts simply plant and abandon, but without maintenance especially during the first few years, the trees just die. To kill cancer cells, you have to find something that differentiates them from normal cells. One of those things is a compound called acrolein that’s unique to cancer. Japanese scientists found that an organic molecule called azide can attach to those cancer cells and, when paired with a fluorescent compound, can light up the cancer. Well well well, they said — if we can attach a fluorescent compound, maybe we can attach a radioactive bomb. That “bomb” is actually a radionuclide called astatine-211 that emits alpha particles as it decays. And the nifty thing about alpha particles is that A) they’re deadly, and 2) they only travel a fraction of a millimeter. In other words… In theory, when astatine-211 is anchored to the inside a cancer cell, the emitted alpha particles should damage the cancer cell, but not much beyond. They tested this on mice, and you betcha it worked — 100% of the mice survived when it was injected into the tumor (80% when injected into the blood). Not only will this work with a lot of different kinds of cancer, thanks to the azide’s targeting ability, “[W]e can use this method to treat very early-stage cancer even if we don’t know where the tumor is.”AZ meets the Lorax, when placebos equal opioids, radiation-bombing cancer, and more
When opioids do nothing
Health journalists not doing their jobs
Bad CNN! No cookie!
Vitamin D non-story
Coffee (not caffeine) gives the get-up-and-go
Shout-out to AstraZeneca
A cancer-seeking radioactive missile
June 29, 2023 ✒ Andrew Kantor
There might be a surprising — and inexpensive — treatment for couples who are “experiencing unexplained infertility”: good ol’ vaginal progesterone, used safely for decades. British researchers who conducted a small study found that women who used the progesterone (400 milligrams twice a day for 14 days) conceived twice as often as the untreated women — 15.3% compared to 7.0%. (The researchers point out the small sample size, though, which means it could have happened by chance.) Oh, and the miscarriage rate with the progesterone treatment was half that of the women who weren’t treated. They don’t know what’s going on — “It could be that treating women with vaginal progesterone is helping the womb to become more receptive to a fertilized egg” — but the results are encouraging. “We need to do further research to prove these results in a larger group of people, but this trial suggests a potential treatment for couples with unexplained fertility. Given its safety and low price, there is no harm in offering this treatment in the meantime.” The hot new way to treat pancreatic cancer is by targeting a gene called KRAS, where mutations drive pancreatic cancer. But there’s a problem. Inhibiting the KRAS gene actually comes back to bite — it turns on a different gene called ERBB, and that just undoes the drug’s hard work: “when KRAS goes down, ERBB goes up and drives KRAS and other related genes back up again.” So the obvious plan: Target both KRAS and ERBB. Which is what UC San Diego researchers did. (There’s already an FDA-approved ERBB inhibitor called Afatinib.) In the lab, that one-two combo worked a treat. “[T]he benefits of using the two drugs together were even larger than the sum of each one’s individual effect. In other words, the drug pairing was greater than the sum of its parts. Thus, the UCSD folks say, “[W]e strongly encourage the clinical testing of this drug combination for patients with pancreatic cancer.” Dutasteride, aka Avodart, is technically for treating an enlarged prostate, but it’s also (wink wink) sold as treatment to stop hair loss. But does it work? And if so, how? The folks at Healthline have all you need to know about dutasteride. (Spoiler: Yes, it does seem to work, but “it may be best to manage your expectations.”) It’s an old question: Why do some statin users get muscle pain and weakness? Now there’s an answer. It’s about an obscure enzyme called HMG-CoA reductase. Two facts about it: As you might imagine, “This connection between a rare disease and a common drug stunned the researchers.” Happy twist: The Israeli team that discovered that it was the cause of limb girdle muscle dystrophy also found a treatment. It’s a drug called mevalonolactone that “allows muscle cells to function more normally even without the HMG-CoA reductase enzyme.” That could mean a treatment for people for whom statins cause severe muscle pain. Sad twist: mevalonolactone may also increase cholesterol, so it would only be for the worst-off patients. This is the kind of interesting connection that might come into play later as we tease out what’s causing what. Johns Hopkins researchers have found a connection between the sense of smell as people age, and the chance of their suffering from depression. Or, put more science-y: “[R]esearchers found that individuals with decreased or significant loss of smell had increased risk of developing significant depressive symptoms at longitudinal follow-up than those in the normal olfaction group.” And the worse the loss of smell, the greater the depression. But which way does the connection go? Is the same factor causing both (e.g., altered serotonin levels, brain volume changes)? Or does one lead to the other — maybe less smell means less appetite means less socializing? “Losing your sense of smell influences many aspects of our health and behavior, such as sensing spoiled food or noxious gas, and eating enjoyment. Now we can see that it may also be an important vulnerability indicator of something in your health gone awry. “Smell is an important way to engage with the world around us, and this study shows it may be a warning sign for late-life depression.” This actually makes logical sense, but it’s good to have a study to prove it: When people have better access to prescription opioids, opioid-overdose deaths go down because “When access to prescription opioids is heavily restricted, people will seek out opioids that are unregulated,” as the lead author of a Rutgers paper explained. Add hypertension to the possible effects of long Covid — in women, at least. A small study (23 women) out of the University of Texas found that… … while only one participant with long Covid had been diagnosed with hypertension prior to contracting Covid-19, “two patients had received a new diagnosis of hypertension post-Covid-19, two had resting [blood pressure] values classified as Stage II hypertension, one as Stage I hypertension and two with high [blood pressure] based on the current guidelines.” The elevation in resting blood pressure was consistent.A better hair loss treatment? Plus fertility made easier, depression and smell, and more
Could a simple fertility treatment be right in front of us?
A pancreatic cancer double-punch
The Long(ish) Read: Keeping the hair?
Why statins cause muscle pain
Less smell, more depression
Short Takes
When opioids are outlawed, people become outlaws
And the latest long-Covid effect…
June 28, 2023 ✒ Andrew Kantor
When it comes to treating migraines, there’s one class of meds that often overlooked: anti-hypertensives. Blood pressure drugs, found Aussie researchers, almost all help with migraine pain, but they’re often overlooked by physicians as a first-line treatment. “[W]hile we can see from the analysis that the effect is true for almost all types of BP medicines, this is not reflected in the current clinical guidelines, which specify just one or two types (such as beta-blockers) but not the full range of therapies that could be useful.” Having trouble makin’ that baby, guys? Did you perchance have even a mild case of Covid-19? That might be your answer. Spanish researchers found that Covid-19 infection caused not only a drop in sperm count months after infection, but also a drop in sperm quality. Worse, this wasn’t just in the sperm that were hanging about while you were infected — the effect continues into the new crop*. “We assumed that semen quality would improve once new sperm were being generated, but this was not the case. We do not know how long it might take for semen quality to be restored and it may be the case that COVID has caused permanent damage, even in men who suffered only a mild infection.” * “Crop of sperm” is either a poor choice of words or a new rock band. Your call. Having a serious Covid infection might lead to chronic pain. It certainly increases the odds, according to researchers at New York’s Upstate Medical University. More than a quarter of the people in a study (25.5%) who had a moderate to severe infection reported chronic pain since their bout. That compared to fewer than 20% of those who were never infected. The bottom line, after the statisticians got involved, is that… “Adjusted probabilities show that chronic pain was roughly 4 percentage points more likely among those with more symptoms during infection than among the never-infected group.” Eli Lilly’s experimental weight-loss pill “helped people lose an average of 15% of their body weight after 36 weeks,” which is as good or better than giving yourself weekly injections of one of the other GLP-1 agonists. Called orforglipron, the pill is still in phase-2 trials, while Novo Nordisk’s semaglutide pill is a bit ahead (phase 3), but requires a 30-minute fast before and after taking it, which could be a complication considering the target audience. Eisai/Biogen’s Alzheimer’s drug Leqembi (aka lecanemab) is likely to get full FDA approval soon, but it comes with caveats that might make it a bit tougher for patients to get. Read the deets. For the first time in 20 years, malaria is spreading locally in the US — and it’s in Florida and Texas. Locally is the key, because cases reported here have always been acquired elsewhere. These, though, “are believed to be locally acquired” and transmitted by mosquitos. Getting people weaned off long-term opioids has to be done carefully, and an international group of clinicians, led out of Australia, has released a set of deprescribing guidelines. They recommend “that clinicians develop personalised deprescribing plans from the beginning for any patient being prescribed opioids” and also published detailed guidelines for creating such a plan. GSK’s vaccine for people at high risk of gonorrhea has received a ‘fast-track’ designation from the FDA. Called Neisseria, it’s currently in a phase 2 trial, but the new designation will mean FDA review could happen more quickly.Covid hurts men where it counts, plus simple migraine meds, malaria makes a comeback, and more
The easy migraine treatment
When your sperm get long Covid
Speaking of Covid…
Another weight-loss pill shines in trial
The Long Read: Getting the new Alzheimer’s meds
Short Takes
Malaria is back
Weaning off opioids the right way
Gonorrhea vax gets fast-tracked
June 27, 2023 ✒ Andrew Kantor
Georgia ranked 45th out of the 50 states and DC for the performance of its healthcare system in the latest annual report from the Commonwealth Fund. The study considered a long list of factors, including “Avoidable deaths from preventable and treatable causes,” access to healthcare, maternal care and mortality, and mental health care. (Of note, this report included the pandemic years, so every state saw its overall score take a hit.) What hurt Georgia a lot: The good stuff: a low rate of alcohol- and drug-related deaths. You can read the overview of the study here, and see the details of Georgia’s performance here (7-page PDF) A new tactic against antibiotic resistance can, it seems, keep bacteria from evolving that resistance in the first place. It’s called dequalinium chloride (DEQ), and right now it’s just “proof-of-concept for evolution-slowing drugs.” Essentially, Baylor College of Medicine researchers found that when stressed (like, say, with impending destruction) certain of the bacteria’s genes can activate to “increase production of protective molecules.” Not only does that program protect the bacteria at the moment, it can also affect its genes for the long term — i.e., making it resistant to the antibiotic. But DEQ, the Baylorites say, can “dial down the master bacterial stress response.” That not only makes the bacteria more susceptible to antibiotics, it prevents its children from inheriting that resistance. Given together with cipro, DEQ reduced the development of mutations that confer antibiotic resistance, both in laboratory cultures and in animal models of infection, and bacteria did not develop resistance to DEQ. Of patients with major depressive disorder, more than a quarter fit into what Stanford researchers say is a new subtype of depression they call the cognitive biotype. Here’s the interesting part: First they tested to see how many fit into this category (which is indicated by “difficulty with the ability to plan ahead, display self-control, sustain focus despite distractions and suppress inappropriate behavior”). That was about 27% of patients. Then they tested to see how three common antidepressants affected them. Result: Patients with this new subtype were less likely to be helped by typical drugs like escitalopram, sertraline, or venlafaxine. [T]he overall remission rates — the absence of overall depression symptoms — were 38.8% for participants with the newly discovered biotype and 47.7% for those without it. This difference was most prominent for sertraline, for which the remission rates were 35.9% and 50% for those with the biotype and those without, respectively. So what could help? They’re thinking guanfacine, aka Intuniv or Tenex, might do the trick; testing is ongoing. “Moms lose significant sleep and free time during kids’ school year, new study finds”. The old thinking: Variants in any of more than 100 genes could lead to early menopause — i.e., before the age of 40. But now British researchers have found that a whopping 98% of women carrying variations of those genes in fact had menopause after 40. In other words, some women might be diagnosed with ‘premature ovarian insufficiency’ when it doesn’t apply at all. As the senior author put it (in, obviously, a lovely British accent), “It now seems likely that premature menopause is caused by a combination of variants in many genes, as well as non-genetic factors.” Using a new type of biosensor, Johns Hopkins researcher found that ruxolitinib — already FDA approved for treating some cancers and skin conditions, can also treat cardiac arrhythmias by inhibiting the CaMKII protein. A 10-minute application of the drug was enough to prevent catecholaminergic polymorphic ventricular tachycardia, a congenital source of pediatric cardiac arrest, and rescue atrial fibrillation, the most common clinical arrhythmia. The finding could lead to new uses for the drug, including (they suggested) “the ‘pill in a pocket’ scenario” where patients could take a ruxolitinib-based medication occasionally as symptoms arise. For a long time, BMI (body mass index — the ratio of weight to height) was the go-to measurement for obesity. But as you might imagine for such a crude comparison, it’s on its way out as a reliable tool. [P]eople with the same BMI may have substantially different body fat percentage based on a variety of factors such as age, muscle mass, sex and race. In an example from one large study, adults with a BMI of 25 had a body fat percentage ranging from 14% to 35% for men, and 26% to 42% for women. GSK, the company formerly known as Glaxo Smith Kline, decided it needed to stop investors from freaking out over impending lawsuits over Zantac. You remember Zantac, right? The heartburn drug that ended up causing cancer? Anyway, the company settled a lawsuit with a guy from California before it could go to trial, and that “could set a precedent for thousands of cases set to go to trial next year” and which gave investors jitters. Merck is now facing a slew of lawsuits over Singulair, its asthma and allergy medicine. The FDA required a black-box warning because of psychiatric side effects. Now, the plaintiffs say, they have evidence that Merck knew about those dangerous side effects long before that warning was required — it just didn’t disclose them.A drug to stop evolution, a new type of depression, why BMI is useless, and more
Report: Georgia’s health needs improvement
Take that, Darwin
A new depression subtype (and why antidepressants don’t always work)
Captain Obvious uses earplugs (and locks the door)
Premature menopause is more complicated than we thought
Old drug, new heart treatment
The Long Read: Why BMI is yesterday’s metric
Short Takes: On the legal fronts
GSK settles Zantac suit
What did Merck know and when did it know it?
June 24, 2023 ✒ Andrew Kantor
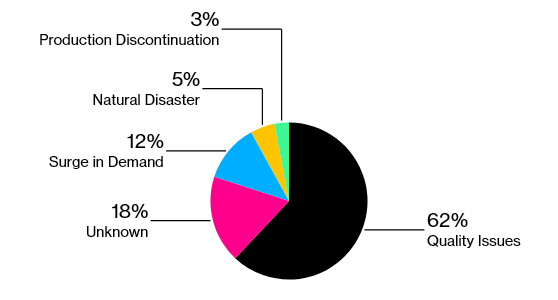
The US military is going all trust but verify on the FDA. The Department of Defense is apparently concerned enough about the quality of generic drugs — many of which come from facilities (foreign and domestic) that have had … issues — that it’s talking to independent lab Valisure to test generic drugs for contamination. The move raises questions about the Food and Drug Administration’s ability to adequately police generic medicines. With mounting drug shortages, most of which are caused by quality problems, military officials have gone so far as to call vulnerabilities in the drug supply chain a national security threat. Fun fact: Kaiser Permanente already does this. “Kaiser, which serves 12.7 million Americans, started working with Valisure on additional drug quality checks more than two years ago.” And with the possibility of regulations being loosened in order to ease drug shortages, you can bet that quality is going to get a bunch more scrutiny. If for some reason you’re selling Elf Bar or Esco Bar disposable e-cigs, stop. They’re illegal, and the FDA is cracking down — it “issued warnings to 189 convenience stores, vape shops and other retailers” so far, and customs officials are seizing the stuff at ports. Fun fact: When vapes are outlawed, only outlaws will sell vapes. Under the law, companies were supposed to remove their vapes from the market and file FDA applications, but new products continue to launch. There aren’t any treatments for tinnitus, but that doesn’t mean people haven’t come up with some interesting ones. Do any stand out? Yes, as a matter of fact, said Brazilian scientists. Shooting lasers at it. Of course, no one calls it “shooting lasers in your ears” — it’s low-level laser therapy and associated photobiomodulation. And, per the study, it’s the best of a so-so lot of options. The contenders: The treatments tested were laser acupuncture, flunarizine dihydrochloride, Ginkgo biloba (a medicinal plant), and low-level laser stimulation of the internal auditory canal or meatus (transmeatal stimulation), on its own and combined with vacuum therapy, ultrasound, G. biloba or flunarizine dihydrochloride. “The best outcomes,” they found, “were observed in patients treated with laser acupuncture alone and transmeatal low-power laser stimulation alone.” Now you know. This is a story that runs every year, so we’ll keep it short. Remember that a bunch of medications you dispense might make your patients more susceptible to sunburn. The folks at Healthline have the list of common and less-common meds that might suggest a bottle of SPF 30 with every purchase. As much fun as I like to poke at the Atlantic, it does do good journalism … although it dies like to channel its inner Eeyore. If you’re interested in a balanced look at the Covid-origins debate, the magazine’s got you covered with the evidence, the questions, and the contradictions for both a lab-leak theory and a public-market theory, taking into account the latest revelations. [T]he origins question has broken down into a pair of rival theories that don’t—and can’t—ever fully interact. They’re based on different sorts of evidence, with different standards for evaluation and debate. Each story may be accruing new details—fresh intelligence about the goings-on at WIV, for example, or fresh genomic data from the market—but these are only filling out a picture that will never be complete. In between flu vaccines and flu treatment are flu preventatives — drugs given to people at high risk from the flu but who can’t be vaccinated. And the FDA has just fast-tracked one (CD388) from Cidara and Janssen. Scientifically speaking it’s technically a drug-Fc conjugate and officially for “the prevention of influenza A and B infection in adults who are at high risk of severe influenza, including those for whom vaccines are either ineffective or contraindicated.” President Biden signed an executive order designed to increase women’s access to contraception. The goal is to keep the issue of abortion from even arising in the first place by reducing unwanted and unplanned pregnancies. Plans going forward “could include convening pharmacies, employers, and insurers to discuss the issue.”Lasers vs tinnitus, DoD distrusts FDA, annual sunburn story, and more
DoD isn’t happy about med safety
FDA: Illegal vapes are illegal
Lasers beat pharma for tinnitus
Sunburn and meds
The latest Covid-origins overview
Short Takes
A new flu-blocking med
Just gonna put this out there