December 14, 2024 ✒ Andrew Kantor
A reminder that the latest CDC recommendation for the pneumococcal conjugate vaccine is that people 50 and older should get it. (It had been 65 and older, but that changed this October.) Considering that pneumonia killed 40,000 Americans in 2022 alone, getting the vaccine seems like a no-brainer. Apparently Robert F. Kennedy Jr.’s lawyer — who is helping review candidates for HHS positions — is so off the deep end of the bell curve when it comes to vaccines, he actually petitioned the FDA to revoke its approval of the polio vaccine. In fact, his law firm specializes in trying to prevent vaccines from being required … or even available. It’s not known whether he receives funding from iron-lung manufacturers. It’s been on the radar since 2018, and now the FDA might finally, really and for true officially limit the amount of nicotine allowed in tobacco products. The agency submitted a proposed rule to that effect to the Office of Management and Budget, which will pull out its abacus to determine how much of an impact it might have on the budget. When you consider how much harm smoking does — and thus how much taxpayers pay to treat people — it could be a whopping big savings. Flu activity is still low across the country, but it’s rising a bit. Covid levels are “moderate” and also starting to rise in some parts of the country (not Georgia, though). RSV activity continues to rise. So far this year, only 2 kids in the US have died of the flu. Last flu season the total number was 205, setting a new record — and that’s not counting the 521 kids who died from complications related to the flu. And last year saw the lowest flu vaccination rate among kids in more than a decade. Probably a coincidence. That said, this year even fewer kids have gotten the flu vaccine than last year — only 37% compared to 43% at this time in 2023. The human body naturally produces antibodies against Staphylococcus epidermidis, a harmless bacteria that lives on our skin. Stanford Med researchers found that mice, which don’t have S. epidermidis, will not only generate the same immune response if you just dab the bacteria on their fur, that response is long-lasting. In other words, you can vaccine mice against S. epidermidis with just a skin rub. So the Stanfordians tried something (and this is a very broad-brush description): They genetically engineered S. epidermidis to contain the tetanus toxin. Then they swabbed it on the mice. And those mice “developed extremely high levels of antibodies targeting tetanus toxin.” Then they tried it with diphtheria. Same result. Then they tried lower and lower amounts of the tetanus toxin. Same result. So yeah, they’ve created a topical vaccine delivery system … for mice. “We know it works in mice,” [said the lead researcher]. “Next, we need to show it works in monkeys. That’s what we’re going to do.” If things go well, he expects to see this vaccination approach enter clinical trials within two or three years. Current HIV PrEP antiretrovirals (e.g., Truvada) are taken orally, and they have to be taken daily … and consistently. But an alternative — a twice-yearly shot of Gilead’s lenacapavir — appears to be 96% effective at preventing HIV, according to the company’s phase 3 study conducted by Emory University and Atlanta’s Grady Health System. 99% of the participants in the lenacapavir group did not acquire an HIV infection. During the trial, only two participants in the lenacapavir group, comprised of 2,179 people, acquired HIV. This compares to nine new HIV infections in the Truvada group, which had 1,086 people. In fact, lenacapavir is showing itself to be so effective against HIV that it was named Science magazine’s Breakthrough of the Year. West Virginia started covering GLP-1 agonists for its state employees, figuring it would save on medical costs in the long run. Then a couple of years later, it changed its governmental mind, leaving thousands of employees in the lurch … and gaining back weight. Read about the fallout from “West Virginia’s Weight-Loss Experiment.”Topical vaccine breakthrough, anti-vax extremism, nicotine reduction could be coming, and more
More people can get pneumonia shot
When anti-vax goes to a whole new level
Nicotine reduction moves closer
Short takes
Respiratory update
Not a good sign
Skin in the (vax) game
HIV PrEP breakthrough
The Long Read: Country road edition
December 12, 2024 ✒ Andrew Kantor
ICYMI: A bipartisan bill was introduced in Congress that would prohibit health insurers or PBMs from also owning pharmacies. For example, CVS Health would have three years to divest itself of CVS Pharmacy, while PBMs like Express Scripts would need to divest their mail-order pharmacies. If passed, the legislation would be the most far-reaching intervention yet into the operations of pharmacy-benefit managers, known as PBMs, and their parent companies, cutting off a major source of revenue for the companies and frustration for patients. The chances of the bill passing in this Congress are just about zero, but look for it to appear again early next year. Amusing note: You can tell how the Wall Street Journal headline writer feels — apparently it’s a congressional “plot” to force these breakups. Walgreens is looking to sell itself to a private equity firm next year, which likely spells the beginning of the end for the pharmacy retail giant. Private equity firms typically take a company, run it into the ground with cost-cutting, employee-burning-out, and quality-reduction measures until employees and customers give up. Then the company goes into bankruptcy and whatever remains of the carcass is sold off. Anyone remember Toys ‘R’ Us? The Limited? Friendly’s? Red Lobster? This is still just a possibility, though — “looking to sell itself” isn’t the same as “signing a contract.” The Mysterious Respiratory Virus that’s killed more than 30 people in the “Democratic” Republic of the Congo contains the malaria virus. The question remains, though: Is it just malaria, or is something mixed in with it? A study out of Harvard Med found that GLP-1 drugs reduce the risk of venous thromboembolism — i.e., serious blood clots. Here’s the twist: It works regardless of the patients’ weight, and even before patients start losing weight. So, “It may be beyond just weight loss that there is an impact.” A new study once again shows the benefits of coffee. This one claims that … [M]oderate coffee consumption (three cups per day) not only contributes to a longer life but also enhances the quality of those additional years by reducing the risk of major age-related diseases and maintaining better overall health. Wow! And that’s just three cups, which is about 1 ½ typical mugs! Oh, wait. The study was funded by … coffee companies (via their “Institute for Scientific Information on Coffee”). Here at Buzz we’re optimistic about the benefits of coffee, but we don’t trust any organization that tries to obscure its bias, so here’s your grain of salt: The Supreme Court said it wouldn’t hear a lawsuit from drug makers (via their trade association, PhRMA) challenging a provision in Arkansas’s 340B program. The Arkansas law required pharma companies to give “discounts on drugs dispensed by third-party pharmacies that contract with hospitals and clinics serving low-income populations.” (That emphasis is critical.) Refresher: Now that the Arkansas law has effectively been upheld, the matter is settled: Drug makers must give discounts on medications used by low-income patients at hospitals or clinics, regardless of the dispensing pharmacy. Until they find a workaround, of course.Walgreens could be ending, PBM-breakup bill intro’d, 340B program upheld, and more
Bill would prevent PBMs from owning pharmacies
Walgreens enters the endgame
Short takes
It’s malaria
The latest GLP-1 trick
Coffee … with salt
SCOTUS upholds 340B
December 10, 2024 ✒ Andrew Kantor
Of all the strains of E. coli that might live in your gut, two of them have an interesting adaptation: They produce colibactin, a carcinogen. Researchers at the Wellcome Sanger Institute were curious about this, especially in light of rising rates of colorectal cancer. So they looked to see who was more likely to have these particular strains in their guts. What d’ya know — they’re more prevalent in Western countries with high (well, higher) rates of colorectal cancer. This means that if there really is a fairly direct connection between that bacteria and colorectal cancer, it might be possible to develop a vaccine — or simply some probiotics — to reduce or eliminate those strains. It’s a GPhA Buzz axiom that just about every medical condition seems to involve either gut bacteria or inflammation. Take Parkinson’s. Japanese researchers found an interesting correlation: People with the disease had lower levels of gut bacteria that synthesize vitamins B2 (riboflavin) and B7 (biotin). Lacking those vitamins, they found, weakened the intestinal barrier — meaning more toxins could enter the bloodstream and cause Parkinson’s inflammation. We’d like to say there was a huge breakthrough — that B-vitamin supplements reduced Parkinson’s symptoms. Unfortunately they haven’t gotten that far … yet. They agree, however, that “Supplementation therapy targeting riboflavin and biotin holds promise as a potential therapeutic avenue for alleviating [Parkinson’s disease] symptoms and slowing disease progression.” (And they think their findings might provide more clues to Parkinson’s progression.) There are treatments for the physical effects of Parkinson’s disease, but not for the cognitive decline. That might change, thanks to a protein called PNA5. According to University of Arizona researchers, it seems to reduce the particular kind of inflammation associated with Parkinson’s; it “dials back the microglia’s overly active immune response and brings it closer to a normal state.” It’s still in the early stages of testing, but signs, they say, are hopeful. HPV vax is working. A new study out of the Medical University of South Carolina found that, from 2013 to 2021, cervical cancer among American women under 25 declined by 62%, “a finding largely attributed to the wide availability of HPV vaccination for this age cohort.” The more you know. Did you know that alcohol is a serious risk factor for cancer? If not, you’re in the majority, according to a survey from the University of Pennsylvania. “Six in 10 surveyed were unaware that regular alcohol use increases odds for developing cancer.” (Worse, 20% of people thought alcohol could lower your risk.) One of the ways to fight prostate cancer is to block a particular molecular signalling pathway that seems to help tumor growth. That pathway is started by a protein called glycoprotein 130 (GP130), and it eventually activates a molecule called STAT3 — and STAT3 is critical to tumor growth. So if you stop GP130, that cuts back on STAT3 and slows the tumor’s growth … right? That was the assumption, until Swedish researchers questioned it. What if STAT3 didn’t do what we thought? And that’s exactly what they found to be the case. When they deliberately activated that GP130 pathway (in mice), it increased STAT3 levels as expected. But then the twist: “They could then see that the result was that the growth of the tumour was clearly slowed down in the mice due to the activation of STAT3” (emphasis ours). Then they looked at human tissue samples and found the same thing: “those high levels of GP130 positively correlated with better survival.” What’s next? That old mantra: More research is needed. In this case, it’s to confirm the results and see if this opens a new, ‘opposite’ way to treat prostate cancer. According to the WHO, antimicrobial resistance (AMR) is getting so bad that in the next 25 years it could lead to more deaths worldwide than cancer does. One solution might be better vaccinations to reduce the use of antibiotics. As one virologist put it: “When vaccines prevent illness, they reduce the need for unnecessary antibiotic use. In the past, antibiotics were frequently prescribed for respiratory infections — typically caused by viruses — leading to misuse and heightened resistance. By preventing viral infections through vaccines, we reduce inappropriate antibiotic prescriptions and, subsequently, AMR.” The old way of monitoring brainwaves: a whole lot of wires attached to a complicated, finicky head covering, with EEG sensors glued to the patient’s head: The new way: temporary tattoo sensors printed on the scalp — they can even work through hair. “[O]nce dried, it works as a thin-film sensor, picking up brain activity through the scalp.” Even better, the tattoos last longer than the traditional sensors, which dry out and lose connectivity after a few hours. Tattooed EEGs, two Parkinson’s possibilities, colon cancer might be vax-able, and more
A hint of a colon cancer vaccine
B vitamins and Parkinson’s
Speaking of Parkinson’s…
Short takes
Prostate cancer ‘flip’
Resistance gets worse
Non-pharma cool medical story of the week
December 07, 2024 ✒ Andrew Kantor
Those shifty Danes have a lot of eggs in the Novo Nordisk basket. Macroeconomics blogger Joseph Politano explains how “Weight Loss Drugs Continue to Power Denmark’s Economy”. The boom “has been so strong that it has almost singlehandedly made Denmark one of the fastest-growing economies in the European Union.” People may want to believe otherwise because it just feels more … natural? But one doctor looked at the studies and delivers the verdict, “No, Diet and Exercise Are Not Better Than Drugs for Obesity”. The only reason that the world isn’t comfortable with the eminently provable truth that diet and exercise are inferior to obesity medications for weight management is weight bias. The message is that people simply aren’t trying hard enough. Opioids are often part of cancer treatment to help patients deal with pain. But they can also interfere with the immune system — something you don’t want when you’re giving immunotherapy. (Science: “[M]orphine binds to an opioid receptor called OPRM1 on CD8 T cells, suppressing their activity and canceling out the invigorating effects of anti-PD1 therapy.”) Good news out of the University of Pittsburgh, where researchers found a potential work-around. They found that peripherally restricted OPRM1 antagonists (PAMORAs) — methylnaltrexone is one — “blocked opioid-induced immunosuppression and improved response rates to immune checkpoint inhibitor therapy.” Big ol’ caveat: This was only in mouse models, and specifically head and neck cancers, but it certainly feels like a breakthrough. The healthcare industry may be expressing sympathy for the murder of UnitedHealthcare CEO Brian Thompson, but patients? Not so much. One social post that got the most traction read, “When you shoot one man in the street it’s murder. When you kill thousands of people in hospitals by taking away their ability to get treatment you’re an entrepreneur.” Side note: UnitedHealthcare denies more claims than any other health insurer — we’re talking a third of them. And the company has been facing protests, lawsuits, and even a Senate investigation for its practices. Side side note: The vitriol on Twitter/X got so bad that the company — which allows Nazi sympathizers, Russian trolls, conspiracy theorists, and hate speech without blinking an eye — took some of them down. At least 79 people in the “Democratic” Republic of Congo have died — and almost 400 sickened — from “a mystery flu-like disease” that health authorities there are still trying to identify. They know it’s respiratory and likely airborne, but that’s about it. Of course, how important can a mysterious flu-like disease be when it’s in a country on the other side of the world? Yet another study — this one using health data from about 192,000 people over 30 years — has shown that eating dark chocolate, but not milk chocolate, can reduce your risk of type 2 diabetes. [T]he researchers found that people who ate at least five ounces of dark chocolate per week — equivalent to five servings — had a 21 percent lower risk of developing Type 2 diabetes compared with people who rarely or never ate dark chocolate. The US already has one of the lowest life expectancies among developed nations. It’s getting better, but a new report finds that it’s slowing compared to the rest of the world. That means we’ll drop even further in the rankings by 2050 thanks to “drug use disorders*, high body mass index, high blood sugar, and high blood pressure” combined with our well-below-average healthcare access. Despite the progress the U.S. has made over the last three decades, the country is forecasted to rank progressively lower than other nations globally in the average number of years a person can expect to live in good health. Known as healthy life expectancy or health-adjusted life expectancy (HALE), its global ranking is forecasted to drop from 80th in 2022 to 108th by 2050. * “That’s the highest drug use–related mortality rate in the world and more than twice as high as the second-highest country, which is Canada.” GLP-1s beat dieting, a Novo-driven economy, UHC hammered on social, and more
And you thought it was those butter cookies
Better dieting through chemistry
Kill the pain, leave the treatment
ICYMI
Vicious crime, vicious reaction
Should we worry yet?
Embrace the dark side
Moving ahead, falling behind
December 05, 2024 ✒ Andrew Kantor
Don’t want to get a flu shot, ladies? There could be an alternative: Get pregnant. Canadian researchers found that “pregnancy may trigger a natural immunity to boost protection against severe flu infection. How’s that work? Apparently — at least in mice — pregnancy produces “a powerful molecule* that boosts the body’s antiviral defenses, especially in the nose and upper airways,” thus preventing the virus from getting to the lungs. * Interleukin-17+ γδ+ T cells, since you asked A bipartisan group of federal legislators, including Georgia’s Buddy Carter, is asking the Department of Justice to investigate PBMs for their role in the opioid epidemic. The letter was sparked by an investigative report by Barron’s, “Confidential Files Detail PBMs’ Backroom Negotiations—and Their Role in the Opioid Crisis.” It suggested that “the three largest PBMs colluded and conspired to steer patients towards Oxycontin in exchange for $400 million” in rebates. Wrote Barron’s: In total, OxyContin prescriptions sent $85 million to Express Scripts, $146 million to Optum Rx, and $173 million to CVS Caremark, according to one year of sales data between 2016 and 2017. One set of contracts between Purdue and CVS Caremark indicates that rebates increased if health plans covered higher amounts of OxyContin. The legislators not only want the DOJ to investigate the PBMs, they are also taking aim at the vertical consolidation of the industry, as single companies own insurers, PBMs, and pharmacies, driving up costs and limiting options for patients. In just one decade — from 2010 to 2020 — a whopping 29% of pharmacies in the US closed. That includes both independent pharmacies and chains, and it affected Black and Latino neighborhoods the most. Why? Low reimbursement rates from Medicare and Medicaid could be one reason, as could indy pharmacies being cut out of PBM networks. And of course there are the chains closing their less profitable locations. Twist: From 2010 to 2017 the number of pharmacies actually increased, but eventually the rate of closings blew past the rate of new storefronts opening. If you were thinking of moving to Wales either because you hate vowels or because you want to be able to give tattoos to your patients, we’ve got some bad news. Not about the vowels (they still don’t use them there) — rather, a new Welsh law prohibits pharmacists and pharmacy techs from giving tattoos without a license. Since 2017, they’d been allowed to provide “tattooing, body piercing, electrolysis, and acupuncture” without a license, but a new law strips that exemption. Seeing the writing on the wall, the UK Health Security Agency is buying more than 5 million doses of human H5N1 flu vaccine “to boost the country’s resilience in the event of a possible H5 influenza pandemic.”PBMs could face Justice, flu-shot alternative, pharmacy die-off, and more
Nine months of flu protection
Reps to DOJ: Investigate PBMs
Disappearing pharmacies
Elsewhere: Across the Pond
Tattoo you
At least someone’s preparing
Answering the important medical questions
December 03, 2024 ✒ Andrew Kantor
Medicare open enrollment ends this coming Saturday, December 7. A lot of older women take various kinds of hormone therapy, especially post-menopause. Lurking in the background, though, is a fear of cardiovascular disease — that’s thanks to a 1990s study that found a risk. It focused on a single kind of hormone treatment, though, so Swedish researchers wanted to see if it still applied to today’s varied therapies. They looked at seven different hormone treatments, and what they found was nuance. I.e., “Different menopausal hormone treatments pose different risks.” For example, the synthetic hormone tibolone* […] was linked to an increased risk of both heart attack and stroke, but not to an increased risk of blood clots. Combined preparations containing both oestrogen and progesterone instead increase the risk of blood clots, including deep vein thrombosis. They also found that patches were less risky than other delivery methods, so their next task is to break down the effects by age, medication, and delivery method to uncover that nuance. * Not available in the US. A startup called OncoSwab thinks so, based on the fact that “Tumors shed compounds that can be picked up in screening tests,” and lung cancer obviously affects the airways. Thus the OncoSwab test, which is still in the early stages of development, looks for lung cancer biomarkers that make their way to the nasal passages. The best time for a Covid booster, found Yale researchers, depends on geographic location and whether you’ve had a breakthrough infection. “[O]ptimal booster dates precede peak Covid-19 transmission by about 2.7 months,” so in the Northern Hemisphere that means “Administering boosters in September or October can provide up to three to four times more protection against infection compared to booster shots given later in the year.” (But, if you get a breakthrough infection in the fall, it’s best to wait several months for a booster.) Health researcher have barely agreed on what long Covid is, and they’re still trying to figure out what causes it. The latest suspect comes from Australia, where immunologists at the Burnet Institute think there’s a “compelling case” that long Covid is actually caused by the virus lingering in the body. They reached this conclusion after looking at details from several studies on the condition, such as more than one that … … detected replicating viral RNA and proteins in blood fluid of patients years after their initial infection, a sign that the virus is likely replicating for long periods in some hidden reservoirs in the body, perhaps including blood cells. In fact, evidence of viral activity seemed to be common in these studies. (The GI tract is “of considerable interest.”) And while they can’t say so conclusively, “we and other scientists argue the cumulative evidence is now sufficiently compelling to galvanise action.” Earlier this year there was a study that found that kids who used cannabis were a lot more likely to develop psychotic disorders — 11 times more likely, in fact. Well then. But now the twist: A new study that looked at 4 years of data on almost 12,000 kids aged 9–10 found that those psychosis-spectrum symptoms tended to appear before they started using cannabis. And “symptoms typically did not increase after initiation.” In other words, the arrow of causation seems to point to psychosis leading to cannabis use, rather than the other way around. The drug crisis has been around for decades, to the point that there are survivors who are now in their 70s. The Wall Street Journal looks at one of them.Surprising kids-pot connection, hormone-risk questions, Covid booster timing, and more
Quick reminder
Hormone therapy risks: Not so simple
Short takes
Could lung cancer be detected with a nasal swab?
Timing your Covid shot
The next long Covid suspect
Pot for thought: kids, psychosis, and cannabis
The Long(ish) Read: Drug-war casualties
November 30, 2024 ✒ Andrew Kantor
When a kid gets appendicitis, surgery is the obvious solution; appendectomies are a dime a dozen. (Well, not here. In the US, while being incredibly common, they’re “one of the costliest surgical procedures performed during hospital stays.”) They’re so expensive that surgeons, led by a team at Nationwide Children’s Hospital, looked into whether IV antibiotics are a way for parents to save money on their kids’ care. And yep, publishing in the Journal of the American College of Surgeons (!), they concluded that it’s more cost effective to use drugs than to use surgery. “This cost analysis demonstrates that nonoperative management for pediatric uncomplicated acute appendicitis is the most cost-effective management strategy over one year, compared to upfront surgery.” Side note: Appendectomies cost almost three times as much here as in the UK or Switzerland, so an overseas vacation could be a cost-saving option, too. The problem with opioids is that they have a way of combining pleasure and pain relief, and the result (as we know) is addiction. What if you could keep opioids’ pain-killing effect, but block its pleasure effect? That’s exactly what a couple of researchers in New York say they’ve done by combining opioids with a drug called an MAGL inhibitor, “which increases the level of an endocannabinoid, known as 2-AG, in the brain.” Conventional wisdom said that endocannabinoids would increase the opioids’ pleasurable effect, but that turns out not to be the case. Instead, the MAGL inhibitor blocks the release of dopamine, thus removing the pleasure (other than the pleasure of not being in pain). So far it’s only been tested — successfully — in mice, but if it works in humans it “[has] the potential to meaningfully change pain medicine.” For a flare-up of asthma or COPD, five days of prednisolone is the standard treatment. But British researchers have found a better option: a single, higher dose injection of benralizumab. Typically, low-dose benralizumab is used for longer-term treatment, but when given in a higher dose during an asthma or COPD flare-up, it worked better and longer at keeping symptoms at bay. After 28 days, respiratory symptoms of coughing, wheezing, breathlessness, and sputum were found to be better in those on benralizumab, whether or not they were also on steroids. After 90 days, there were four times fewer people in the benralizumab group who failed treatment compared with those receiving steroids. They also found that the benralizumab injection’s effect lasted longer, meaning fewer trips to the doctor or hospital. And, of course, it also avoids the side effects associated with steroids. Bonus: Yes, they do call it a “game-changer.” As many as 20% of people taking GLP-1 agonists don’t respond (or don’t respond well) to the drugs, but the drug makers claimed the number was only 10–15%. What happened? Sure, the companies exaggerated the effect — they did the same when it came to hyping the amount of weight that’s typically lost. But that’s only part of the issue. A British physiologist explains all the other factors that didn’t appear in the clinical trials, from genetics to simple lack of formal support.Opioids without pleasure, appendicitis without surgery, GLP-1s without weight-loss, more!
When drugs beat surgery
Pleasure-free opioids
A better asthma treatment
Why GLP-1s fail
November 28, 2024 ✒ Andrew Kantor
Automatic insulin delivery systems might have a problem. As British researchers found, there’s a lot more affecting blood glucose levels than just carbohydrates, but insulin delivery systems only have one tool: insulin. If something else is affecting glucose levels — e.g., hormones, exercise, stress — patients will still get a dose of insulin, even when there are no excess carbs to respond to. The problem is that, while we might have a general idea of these other factors, we don’t have specific information about their effects. For factors beyond carbohydrates to become more systematically included in clinical practice, scientists need to find a way to measure and quantify their impact and utilise this information in insulin-dosing. In the meantime, clinicians are left with a single blunt instrument until more research can be done. The Biden administration is proposing that Medicare and Medicaid cover GLP-1 agonists to help reduce obesity and all the issues that come with it. Although Medicare is prohibited from covering weight-loss drugs (to avoid cosmetic use), CMS’s angle is that the drugs are treatments for obesity. This sets up a cage match between incoming HHS secretary-nominee Kennedy (anti GLP-1s) and incoming CMS administrator Oz (pro GLP-1s). “Need to sleep? Study pinpoints optimal melatonin dosage and timing” 4 mg of melatonin three hours before bedtime maximized the sleep-inducing effects of the hormone. Canadian officials have given up trying to figure out where a British Columbian teen contracted bird flu: “an exhaustive investigation of the people and domestic animals the unnamed teen had contact with shed no light on how the teen became infected.” The kid has improved from critical to serious condition, but still requires a ventilator. He or she is showing signs of recovery, though. Concerned about “excessive flatulence,” the Australian national science agency is asking residents to sign up for the continent-wide “Chart your Fart” campaign. Participants download an app and record their gas-passing ‘events,’ with the option to rate them for (seriously) stench, loudness, duration, linger, and detectability. The Chart Your Fart app is designed to better understand the flatulence patterns and concerns of Australians as part of our public-led research in the area of health and wellbeing. Women whose ring finger is significantly longer than their pointer might be more likely to have alcohol-dependence issues. Yep, that’s what a new British study found. There’s actually a logic behind it. The hypothesis is that a longer ring finger indicates more testosterone exposure before birth, and men tend to have more alcohol issues than women. In fact, the same lead researcher — who really has a thing for finger length — previously found associations between finger-length ratio and Covid outcomes and oxygen consumption. At 112 — born August 26, 1912 — the British man was the world’s oldest living man. He died this past Monday. Aussies study farts, insulin-delivery weakness, when to take melatonin, and more
When your only tool is insulin, every problem is a carbohydrate
ICYMI
Saving you a click
Bird flu follow-up
Weird science
Did you have to let it linger? (Press 1 for yes)
Every one of you will look at your hands
RIP, John Tinniswood
November 26, 2024 ✒ Andrew Kantor
Hospitals are finding new and interesting ways to deal with the IV fluid shortage caused by Hurricane Helene. (Baxter says its North Carolina plant is producing the fluid, but it’s far from full capacity.) Something you might not think about: As the end of the year approaches, people are scheduling more surgeries to either use up benefits or to avoid a big hit when their deductibles reset in January. That puts an even bigger strain on IV supplies. Using push medication — IV without the fluid — is one way (although it requires more monitoring). Another is to squeeze every last drop out of a bag before starting another; it adds up. And, of course, there’s simply cutting back on fluids: Patients may be asked to take more accountability for their hydration, by drinking Gatorade or water rather than the default of hydrating through an IV. When Merck launched Singulair (aka montelukast) in 1998, it claimed that the drug had side effects “similar to a sugar pill.” It turned out that wasn’t true (and Merck apparently knew it), and montelukast can have serious neurological effects; in 2020 the FDA added a black box warning to the drug “flagging serious mental health risks like suicidal thinking or actions.” Now, four years later, the FDA expert group that looked into montelukast’s side effects found that yes, it binds to multiple brain receptors. “[T]he new data showed significant quantities of montelukast present in the brain. The receptors involved play a role in governing mood, impulse control, cognition and sleep, among other functions.” They still can’t say for sure that the binding causes those neurological effects, but as one scientist said, “It’s definitely doing something that’s concerning.” A new vaccine for whooping cough has a couple of extra benefits. First, it’s nasal — no needles to worry about. Second (and this is the bigger part), it’s also got an “innovative adjuvant called T-vant, [that] boosts the body’s immune response specifically in the respiratory tract.” So what? That means it not only protects the person getting the vaccine, but also reduces the likelihood of them spreading it to others. As the Tulane University immunologist leading the team put it: “By developing a vaccine that can not only protect individuals but also prevent transmission, we hope to improve on existing vaccines and limit the spread of whooping cough in communities.” Of course, with more people believing the nonsense from anti-vaxxers, it’ll fall on more-informed folks to do their part to stop the surge of pertussis. Oxytocin does some interesting things in the body, among them inducing uterine contractions. But it can also treat abdominal pain. The problem is that it’s a peptide, and like most peptides it’s not gut stable; it has to be injected. Aussie researchers, though, say they’ve found a way to make peptides gut stable, meaning oxytocin and derivatives could be made into pill form, and still have all the benefits of peptide-hood (e.g., few side effects). The research indicates that the new molecules work in the colon and do not need to cross the gut barrier into the bloodstream to suppress abdominal pain. Now they just need someone to pay for them to try to make it something they can sell. Deaths from heart disease caused by obesity have gone up 280% from 1999 to 2020 — i.e., nearly tripled — according to research out of Brown University. “Middle-aged men, Black adults, Midwesterners, and rural residents are most at risk.” —and— More than 100,000 Americans under 20 have inflammatory bowel disease — that’s both Crohn’s disease and ulcerative colitis — according to a study out of UNC Chapel Hill. And since 2009 that number has gone up 22% (Crohn’s) and 29% (ulcerative colitis). Remember all the hubbub Florida made about importing vaccines from Canada? The state even sued the feds for not moving fast enough. Well, Florida got the green light in January 2024, and since then … nothing. A Florida health official familiar with the importation program told KFF Health News there was no planned date yet for the state to begin importing drugs. Speculation was that the fuss wasn’t really about getting the drugs, but, as one analyst put it, “It riles up the crowd.” The reality has always been that it won’t happen because Canada won’t allow it, but that didn’t stop people from having a dream. So while there are lots of excuses, there’s no real plan in the works. Maybe just ‘concepts of a plan.’Singulair’s danger confirmed, IV shortage workarounds, Florida standing still, and more
Handling the fluid shortage
Singulair side-effect update
Pertussis vax does more
A peptide for pain
Two quick health stats
Elsewhere: Going nowhere
November 23, 2024 ✒ Andrew Kantor
Continuous glucose monitoring is old news, but how about continuous blood pressure monitoring? That’s what bioengineers at UC San Diego have developed and tested. The patch is a soft and stretchy device, about the size of a postage stamp, that adheres to the skin. When worn on the forearm, it offers precise, real-time readings of blood pressure deep within the body. For science geeks, it works with a type of ultrasound sonar that can “track changes in the diameter of blood vessels, which are then converted into blood pressure values.” Not only did they find it as good as a blood pressure cuff, it was as accurate as an arterial line — the kind of sensor inserted into an artery and the gold standard of continuous BP measurement. We’re finalizing times and places for our Fall Region Meetings, and we’ve got three more confirmed. Don’t miss out on a great night of food, drink, and networking with your fellow pharma professionals! The latest additions: Click here for complete details on your region meeting! The bad news: Yes, taking opioids regularly can increase your risk of dementia. The good news: It doesn’t affect people using the drugs short-term, and may not apply to younger people (the study only looked at people over 60). It’s about cumulative use. Those shifty Danes found that once someone hits a threshold of about 90 ‘total standardized doses’ — that’s 90 days of treatment on the equivalent of 30 mg of morphine — the risk of dementia increases anywhere from 8 to 29%. (Interestingly, the greatest risk increase was in people aged 60-69.) The study had a lot of data, too — it included health info on almost 2 million people over 25 years — and to reduce the question of correlation/causation, they incorporated a 5-year lag between prescription and dementia diagnosis. Still, as usual, more research is needed. So who’s paying for GLP-1 drugs in the US? Medicaid and federal-employee health plans cover the most, according to the rather frighteningly named AXIACI Obesity Coverage Nexus. Here’s the breakdown: And here’s a chart for you visual people: According to data from Mercer — the financial firm, not the university — GLP-1 coverage from larger employers (more than 20,000 employees) hit 64% in 2024, up from 56% last year. If you include firms with just 500 or more employees, that coverage drops to about 44% — up from 41% last year. Alzheimer’s treatments might still be out of reach (or so it seems), but tests for the condition are emerging — for better or worse. The latest comes out of Sweden, and it uses a finger-prick to collect a sample that can be delivered to a lab for analysis. Like existing blood tests, which are still making their way into the mainstream, this tests for an abnormal protein called ptau217. There are a couple of big differences, though. First, it only requires a few drops of blood from a pinprick — no phlebotomist necessary. (It might even be easy enough for home use.) Second, the sample is sent on a special card that doesn’t require refrigeration, making it suitable for places where transport might be an issue. It’s now being tested in Europe for potential availability in the next couple of years. We all know that a cup of hot cocoa can help with stress, but it might do more. British researchers found that “flavanol compounds found in abundance in cocoa and green tea can protect vascular function during periods of everyday stress.” In other words, if the same stress that drives you to cocoa is also driving you to eat high-fat foods (the Brits used butter croissants, cheddar cheese, and whole milk in their study), that cocoa will help alleviate some of the negative vascular effects of the delicious fatty food. GLP-1 economics, real-time BP monitoring, cocoa vs fat, and more!
Easy BP monitoring
We’ve added more Fall Region Meetings!
Opioids, dementia, and nuance
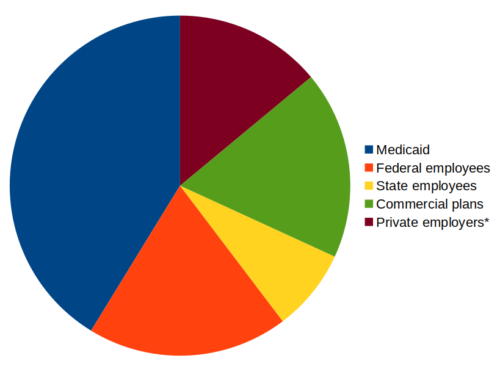
Who’s paying for GLP-1s?
More employers are covering them
An even simpler Alzheimer’s test
Cocoa in times of stress