October 27, 2023 ✒ Andrew Kantor
There’s apparently a link between higher levels of triglycerides and lower risk of dementia. That’s what Aussie researchers found when they parsed the data on more than 18,000 people over six years (average age 75). The higher someone’s triglyceride level, the lower their risk of dementia. (Which makes sense, as triglycerides are one of the brain’s main energy sources.) Of course, this doesn’t mean one causes the other, just that there’s a link. And it doesn’t mean it’s time to load up on green eggs and ham, either. Even if there was a cause and effect, the high triglycerides come with their own set of problems, obviously. The article’s lede sums up the issue nicely: “Diabetes patients who stop using metformin are more likely to develop dementia.” [R]esearchers found that patients who were prescribed metformin but stopped using it were 21% more likely to get a dementia diagnosis compared with patients who continued using metformin throughout their treatment. The big issue, though, is that people don’t like taking metformin. The pill is big and the stomach issues can be an issue especially for people living in small apartments. When oncologists get money from the pharma industry, they’re more likely to prescribe “non-recommended and low-value treatments.” That’s according to a group of cancer researchers and statisticians publishing in the British Medical Journal. Docs prescribing meds from the companies that ‘take them to lunch’ isn’t new, but this is one of the first studies that looked at whether the meds were actually good for the patients. Um … nope. One example: The difference between the prescribing patterns of doctors was biggest for denosumab, a drug sold by Amgen as Xgeva, in castration-sensitive prostate cancer. U.S. guidelines recommend against the use of denosumab in the setting. Yet, 49.5% of patients whose doctors took pharma payments received the drug, compared to 31.4% of their counterparts whose oncologist hadn’t received payment. And now a twist: When there was a choice between a brand-name drug and a generic, the docs who got more money were slightly more likely to prescribe the generic. So at least they’re trying to save the patients some money. “More than 7 million Americans unaware they have mild cognitive impairment.” “Foods like ice cream, chips and candy are just as addictive as cigarettes or heroin.” British researchers have developed a simple blood test that they say can … well, “diagnose” is a strong word. It can reveal biomarkers associated with bipolar disorder. Well, sort of. When they say it can help diagnose it, they mean the blood test alone has about a 30% chance of hitting the mark. When combined with a mental health assessment, though, it’s more useful. Bottom line is that it’s more of a confirmation thing. “Psychiatric assessments are highly effective, but the ability to diagnose bipolar disorder with a simple blood test could ensure that patients get the right treatment the first time and alleviate some of the pressures on medical professionals.” With another walkout planned at chain pharmacies, stress levels high while staffing is low, robotics and AI are coming to a pharmacy near you. Maybe. The idea is to automate the repetitive tasks (and even help with issues like medication interactions) freeing pharmacists and pharmacy technicians for the more important work.7 million to watch for, choosing between the heart and brain, robots in pharmacy, and more
Bad for the heart, good for the brain?
Don’t stop thinking ’bout metformin
Quid pro quo
Short takes
“I ate what?”
You can have my M&Ms when you pry them from my cold, dead fingers
Vaguely useful bipolar test
The Long Read: The Future of Pharmacy edition
October 26, 2023 ✒ Andrew Kantor
If you don’t make enough of a protein called ACE2, your body (and bodies of rats) will produce angiotensin II, a hormone that raises blood pressure. So how do you get more ACE2? By changing your gut bacteria, of course. Researchers at the University of Toledo started with Lactobacillus paracasei (a friendly gut bacterium), engineered it to produce ACE2, and gave it to hypertensive rats with high blood pressure. You’re expecting to read that it work, and it did, sort of. [T]he blood-pressure-lowering effects were only seen in female rats. Though there was no difference in ACE2 expression between male and female rats, only the female rats saw a decrease in their blood pressure. Why? Because, they think, “The gene encoding ACE2 is located in a region of the X-chromosome” that can sometimes be deactivated. The ladies have two copies of it, so they’ve got a backup. Regardless, they call the finding a steppingstone: “It is a real possibility that we can use bacteria to correct hypertension.” High-fives all around to Sharvari Kshirsagar, Sreelakshmi Menon, and Tanishka Saraf — three Mercer students who just took home half of the American Association of Indian Pharmaceutical Scientists’ annual Graduate Student Awards. W00t! They politely sat in alphabetical order When mom is vaccinated for Covid, Junior doesn’t just get protection from the virus, but also has a lower risk of a bunch of “poor outcomes” — notably NICU admission and death. That’s what Canadian researchers found when looking at the health data for more than 140,000 births in Ontario. “Our results were consistent across the number of doses someone received during pregnancy, the trimester in which they were vaccinated, and the vaccine product they received.” Forget injections or even pumps. British researchers say that pregnant women with diabetes should all be using automatic insulin-delivery systems. Their study found that automatic, smartphone-based “hybrid closed-loop technology” technology for mom reduced a baby’s risk of “…premature birth, need for intensive care after birth, and being too large at birth, which increases the lifelong risk of overweight and obesity.” “Compared to traditional insulin therapy methods, women who used the technology spent more time in the target range for pregnancy blood sugar levels — 68 percent vs 56 percent, which is equivalent to an additional two-and-a-half to three hours every day throughout pregnancy.” Even better, they called the technology — wait for it — “game-changing.” When kids get “routine elbow surgery” (apparently that’s a thing), it’s tempting to give ’em opioids for the pain rather than deal with the whining. No need, say researchers at the Children’s Hospital of Philadelphia — ibuprofen and acetaminophen work just as well. The researchers found no significant differences in pain ratings between opioid and non-opioid groups at any timepoint. Notably, 35% of patients who were prescribed opioids never took them, and 49% took only one to three doses over the entire postoperative period. The study looked specifically at a procedure called closed reduction and percutaneous pinning (I see a few people in the audience nodding), but the docs say it might also apply to other orthopedic procedures. GSK reports AOK results for its RSV vax for people ages 50 to 59. It was a phase 3 trial, meaning the company is planning to submit final results to the FDA in hopes of having the shot approved for that age group — or at least people that age who are vulnerable to RSV. GLP-1 drugs like Ozempic and Wegovy can save a lot of lives and a lot of money on healthcare, but they’re way too expensive for many of the people who could benefit. Or are they? The New York Times explains how it’s more than just list price vs. actual price — there are plenty more reasons these drugs are going to be less expensive than we think. Georgia is one of 41 states (and DC) suing Facebook parent company Meta for ‘exploiting and manipulating’ children and playing a major role in the the ongoing youth mental health crisis. Collectively, more than 40 states paint a picture of a company that brushed aside safety concerns about its products in order to addict as many young people as possible as a way of juicing its profits. “[A] flesh-eating parasite known as Leishmania mexicana is now likely spreading locally through some sand flies native to the southern U.S.” Elbows don’t need opioids, change the gut to change your BP, Georgia sues Meta, and more
Bacteria for blood pressure
Today’s Mercer shout-out

For moms to be
Covid vax protection
The right way to give insulin
When OTC painkillers work just fine
RSV vax coming for younger folks
The Long Read: The Cost of GLP-1s edition
Short Takes
States sue over social media
Add it to the list
October 25, 2023 ✒ Andrew Kantor
Patients may be able to give themselves the FluMist quadrivalent vaccine next year, if AstraZeneca’s request is approved by the FDA. The company said it expects the FDA to decide on the vaccine by the first quarter of 2024, adding that it expects the vaccine to be made available for self-administration in the United States during the 2024-2025 flu season, if approved. When you’re looking for a place to stick a device that help provide insulin, you probably wouldn’t think “in the eye.” That’s just what Swedish researchers did, though, and it wasn’t just because it sounds cool. The miniature implants consist of a combo of insulin-producing islets of Langerhans and some electronic sensors, and they’re implanted between the iris and the cornea. Why there? First, the eye is “immune-privileged,” meaning it doesn’t have immune cells that will attack the device. Second, it’s easy for the Swedes to look into it (it being the eye and all) and see how the implant is doing. The first tests on mice found that the implants work just fine for at least several months. It’s a proof of concept — now they want to see about adding the electronics to adjust the release of insulin as needed. Due to shortages of the RSV vaccine — nirsevimab — the CDC is asking providers to ration their supply and only give the vaccine to the most vulnerable infants. CDC recommends prioritizing available nirsevimab 100mg doses for infants at the highest risk for severe RSV disease: young infants (age <6 months) and infants with underlying conditions that place them at highest risk for severe RSV disease. Drexel University released this bombshell: “Can We Trust Autism Information on TikTok? Not Always.” [T]he research team concluded most of the information provided on TikTok appears to be misaligned with current clinical knowledge. Canadian researchers have found a shocking list of “10 predictors linked to opioid overdose in chronic pain patients.” Who needs Daddy’s Little Helper? Apparently an effective alternative to Viagra is a bit of aerobic exercise*. A new study in the Journal of Sexual Medicine … …found that aerobic activities — such as walking or cycling – improved erectile function in all men with erectile dysfunction, regardless of body weight, overall health, or medication use. And the worse the, er, problem, the more the exercise helped. On the standardized scale for this sort of thing, men with the biggest (?) issues reported an average improvement of 5 points with exercise and 4 to 8 points with Viagra or Cialis. So that’s pretty good. This isn’t entirely new. Back in the Long Long Ago (2011), Nigerian researchers published a paper, “Effects of Aerobic Exercise in the Management of Erectile Dysfunction: A Meta Analysis Study on Randomized Controlled Trials” where they found the same thing. * “If I could get the aerobic exercise, I wouldn’t need the Viagra!” Ha ha. A big thank-you to all the AIP members who attended AIP’s fall meeting in Peachtree City! Check out some photos on AIP VP Jonathan Marquess’s Facebook post! People who get a bone marrow transplant have a big risk of graft-versus-host disease (GCHD) — we’re talking 50%. You know what can help reduce that risk? The right gut bacteria. Researchers from Baylor College of Medicine and the University of Michigan found that the gut biome changes after a bone marrow transplant, “and that this change contributes to GVHD aggravation.” Specifically, their levels of butyrate go down. How do you get butyrate levels up? Potato starch. People can’t digest it directly, but a specific gut bacteria can — and it produces butyrate. So add a potato starch supplement, make the right bacteria happy, and reduce the risk from GVHD. So far they’ve confirmed that taking a supplement isn’t a problem. Now they’re beginning to see how much of a difference it’ll make for transplant patients.Insulin inside the eye, easy Viagra alternative, Captain Obvious double duty, and more
DIY flu vax?
Diabetes treatment: The eyes have it
CDC: Ration the RSV vaccine
Captain Obvious is working overtime
Did they really need to do a study?
“Wearing an ‘I abuse drugs’ T-shirt” isn’t on the list
Get up and exercise
Thanks, AIP members!
Safer bone marrow transplants … with potatoes
October 24, 2023 ✒ Andrew Kantor
If you’ve got a patient who takes Paxlovid after testing positive for Covid, keep a metaphorical eye on ’em. A lot of folks who take it are taking other meds and there’s a decent chance of a drug-drug interaction. The median number of concurrent medications was seven. Researchers found that 70% had at least one DDI, which increased to 82% in patients ages 70 and older. Most DDIs required clinical intervention, with most needing assistance from a pharmacist. Note those last two sentences — if there’s an interaction, it’s probably not a minor one. The most common drugs that interact, say the Canadian researchers who did the study, are “cardiovascular drugs and those for benign prostatic hyperplasia, followed by central nervous system drugs and oral antithrombotic agents.” Sure, chances are low that a Covid infection will be a big deal, but it comes with a lot of baggage. A new one to consider: Guillain-Barré syndrome. Based on data for more than 3 million people over 18 months, the Israeli study found that contracting Covid increases your risk of GBS in the six weeks after infection. (Being vaccinated with an mRNA shot reduces that risk.) The bad news: “[P]eople with a recent Covid infection were six times more likely to develop Guillain-Barré than those without a recent infection.” The reality check: GBS is really, really rare, so while a 600% risk increase sounds scary, the actual numbers are still pretty small. (Also, the data show an association not a cause.) NOMINATE A PHARMDAWG TODAY! Do you know a PharmDawg alumnus* who deserves special recognition? The College of Pharmacy is seeking nominations for the 2023 Distinguished Alumnus, Distinguished Service, and Outstanding New Alumni Awards. Click the links below to learn more about the criteria for each award. All nominations should be submitted by Sunday, October 29, 2023. * We assume you can also nominate an alumna. Or an … alumnex? So far it’s a lot lower than last year, but a bunch higher than late October before the pandemic. Take from that what you will. (Georgia has the 17th highest level of flu, and the South in general is seeing higher numbers.) Georgia Pathways, Georgia’s ‘work for Medicaid’ program, is off to a bumpy start, per the Atlanta Journal-Constitution. The plan is expected to cover about 90,000 poor adults within two years, but so far “has enrolled just 1,343 in the three months since it was opened, the state Department of Community Health reported.” Georgia’s program is an experiment; of the 10 remaining non-Medicaid-expansion states, Georgia is the only one given permission to try this kind of enrollment, which “limits coverage to people who can prove they work 80 hours a month or perform other specified activities.” Remember: If a new program doesn’t succeed immediately, it’s a complete and total failure and has to be scrapped*. To hit the state’s projection of 90,000 enrollees by 2025 would mean enrolling about 11,250 people every three months. So we’re behind at the moment. Maybe give it more than 90 days? * That is sarcasm. What’s the biggest driver of obesity? It depends on the diet program you ask. Maybe it’s sugars. Maybe it’s fats. Maybe it’s simply calories. The answer, say University of Colorado researchers, is all three — but behind them all, like a criminal mastermind, is fructose. In broad strokes, fructose prevents the body from using its fat stores for energy (it “triggers our metabolism to go into low power mode”) causing us to eat more to get energy, but also to keep those fat deposits growing. We become, they say, like hibernating bears, but instead of eating a lot and storing fat just for the winter, we’re doing it every day. As always, they say, more research is needed. Sneaky obesity culprit, flu’s start is slow (and fast), beware Paxlovid interactions, and more
Paxlovid reactions
Yet another reason you don’t want Covid
From our friends at UGA’s College o’ Pharmacy
The new Flu Index is here! The new Flu Index is here!
Georgia Medicaid’s slow start
Obesity mastermind
October 21, 2023 ✒ Andrew Kantor
Taking levonorgestrel (aka Plan B) to prevent unwanted pregnancy is effective … but not 100% effective. A way to get it closer to that 100% mark might be to add piroxicam (aka Feldene). A group of researchers from Hong Kong and Sweden found that, by blocking prostaglandin production, piroxicam makes levonorgestrel significantly more effective, especially if the Plan B is taken later rather than sooner. The results showed that the percentage of pregnancies prevented by piroxicam-levonorgestrel co-treatment (94.7%) was significantly higher than that of the levonorgestrel emergency contraceptive pill alone (63.4%). “I love you. I love you on Xanax more.” But benzos might not be as effective as everyone’s been led to believe. That’s the conclusion of researchers at Oregon Health and Sciences University that crunched the data from five FDA-reviewed, phase 2 and 3 studies of alprazolam (aka Xanax XR). Of the five trials the FDA reviewed, get this: Only three were published in medical journals, and only one (!) showed clearly positive results. Using meta-analysis […] they found that alprazolam extended-release was still superior to a placebo, but not as much as the published data had conveyed. Specifically, they found that publication bias inflated the drug’s efficacy by more than 40%. As the senior author put it, “Our study throws some cold water on the efficacy of this drug. It shows it may be less effective than people have assumed.” [But … well, insert something about the placebo effect here.] News stories keep appearing about how the companies selling new weight loss drugs are suing to prevent compounding pharmacies and others from dispensing their own versions. But so many news sources don’t seem to get it. Currently it’s probably* legal to sell compounded versions of semaglutide, no matter what the brand-name companies (Lilly, Novo, etc.) say. The FDA is clear: Drugs in shortage can be compounded. Compounded meds are not individually FDA-approved. Never have been. The active ingredients, though, are. So saying, “The FDA does not review the products for safety, quality, or efficacy” is misleading and designed as a scare tactic. That said, is illegal to call those meds “Ozempic” or “Mounjaro” or whatever — but that’s a trademark issue. It’s also not legal to sell them without a prescription. Duh. What’s happening is that drug companies are trying to confuse these issues to make it sound as if semaglutide compounded by legitimate compounding pharmacies is illegal and otherwise a Bad Thing. It’s not. Take this sentence from a Fierce Pharma article: In September, Eli Lilly filed lawsuits against eight companies in the U.S. that it claims are producing or selling compounded versions of its blockbuster diabetes drug Mounjaro. The word “claims” makes it sound like compounding is bad or illegal. (“Smith Claims Jones is Wearing Shoes Made in Indiana” makes it sound as if there’s something shameful about Indiana shoes.) So when you see “Company X is suing over unauthorized versions of its drugs,” read the details, and don’t fall for this stuff. * I’m not a lawyer so I’m not going to say that with certainty, but the folks at the Alliance for Pharmacy Compounding have a PDF explainer. Not waiting for the FDA to remove phenylephrine products from the market, CVS said it’s yanking decongestants that use it from store shelves. Of note: It’s only removing decongestant-only products like Sudafed PE, not other meds that contain phenylephrine … yet. The idea sounded good: Ban flavored e-cigarettes to reduce the appeal to people, especially minors. But it may be backfiring and driving them to a worse option: traditional cigarettes. An analysis out of Yale of vape policies and sales data over 5 years found that… During the study period, hundreds of localities and seven states restricted or prohibited flavored e-cigarette sales. While these policies did reduce per-capita vape sales, they also substantially boosted cigarette sales. For each 0.7 milliliters of e-cigarette e-liquid not sold due to these policies, the authors calculated that 15 additional cigarettes were purchased. What’s not clear is why people would opt for tobacco — which is obviously a lot worse for you — than for unflavored vapes. (With 71% of the cigarette sales bump for non-menthol varieties, it’s not the flavor. Maybe they just figure life isn’t worth living without flavored vapes. It’s become common after replacing a knee or hip to give patients vancomycin to prevent MRSA infection — after giving them cefazolin during surgery. That might not be a good idea. Aussie researchers found that not only was adding vancomycin to post-surgery treatment not any better, it might even be worse: Unexpectedly, in patients undergoing knee joint replacement, the risk of infection was higher in the group that had the added vancomycin, at almost 6%, than in the placebo group, with a roughly 4% infection rate. “People who eat just two servings of red meat per week may have an increased risk of developing type 2 diabetes” according to a study out of Harvard.Has Xanax been lying to us? Plus a better Plan B, confusing compounding, and more
Boosting Plan B with an NSAID
Benzos may not be that effective
Clearing up some compounding confusion
CVS pulls phenylephrine
When vape bans backfire
Post-joint-replacement antibiotics: one and done
Quick take
October 20, 2023 ✒ Andrew Kantor
Nestlé is so worried about the effect of new weight loss drugs on its bottom line, it’s developing ‘companion products’ to be sold to people taking Ozempic, Mounjaro, and their kin. No, this isn’t candy or packaged food (“Now that you’re on Ozempic, you can eat what you want!”). These are supplements that can help with the “loss of lean muscle mass” from taking the drugs, and — if someone gives up the shots — can help deal with the “rapid regain of weight.” Keep in mind that all this hubbub is because Walmart reported a slight downtick in grocery sales since GLP-1 drugs hit the market. There’s not necessarily any connection, but it’s got food companies in an uproar. Our bet: Could be a mountain, probably a molehill. A US/Canadian company says its smartphone-based AI tool can detect type 2 diabetes from basic medical info and 6 to 10 seconds of voice. You read that correctly. (And it’s not just a press release — the study was published in Mayo Clinic Proceedings: Digital Health.) “Our research highlights significant vocal variations between individuals with and without Type 2 diabetes and could transform how the medical community screens for diabetes.” Think about how much data Big Tech already has about you next time you ask Alexa, Google, or Siri a question … and start getting info about treatment centers near you…. The headline says it all. With the pandemic emergency over and no longer able to suckle on the government teat, the company has announced the new price of its Covid treatment: $1,390 for a five-day course, compared to the $529 the federal government was paying for it. Of course, patients won’t pay that much — between insurance coverage and discount programs it’ll cost a lot less out of pocket… well, directly. Insurers will have to pick up the tab, even with discounts. And when insurers pay more, they pass that cost down. In unrelated news, “Employer Sponsored Health Insurance Premiums Grew by 7% in 2023”: The average annual premium for employer-sponsored health insurance is $8,435 for single coverage and $23,968 for family coverage. It seems that 95% of what ails us is caused by either gut bacteria or inflammation, and when it comes to the latter, vitamin B12 deficiency could be a driver. A new study out of Spain found that “Higher circulating vitamin B12 is associated with lower levels of inflammatory markers in individuals at high cardiovascular risk.” They say that the lower someone’s vitamin B12 levels were, the more interleukin-6 and C-reactive protein they had, and those are both markers of inflammation. Exactly why that’s the case isn’t clear, but the correlation was enough to raise those Spanish eyebrows. Side note: B12 deficiency is something vegetarians need to consider. Just FYI. In case you’re curious, the FDA approves drugs a little bit faster than its European counterpart, the EMA. It’s even faster than the Swiss, and we know how efficient they are. The researchers found that overall, the median review time, from submission to approval, was 39 weeks (about nine months) in the US compared with 44 weeks (about 10 months) in the EU and Switzerland. Part of the reason is the fact that the FDA, by law, “must review and and act on 90% of standard applications within 10 months of the 60-day filing date,” whereas the EU doesn’t have such a rule. A Swedish nursing home has installed — inside its walls — a fake bus stop for its dementia patients. You might think the idea is to make them feel … I dunno. Like they have someplace to sit? (The Dutch have created an entire village for people with dementia — “a nursing home disguised to look like the outside world.”) In Germany there are such fake bus stops outside of retirement homes “to give wandering patients a place where they would instinctively go to sit.” And that makes sense: “Rolf got out again.” “Did you check the bus stop?” But that’s not exactly what’s going on in Sweden. The staff clearly cares about their patients, but the description sounds like some kind of freakish psychological torture: Staff have installed a fake bus stop in a hallway to ease the minds of anxious dementia patients eager to leave. (Emphasis ours.) Yeah, “Some have their bags packed” as they wait on the bench. For the bus that never ever comes. Diabetes changes your voice, Swedish horror home, why to check your B12, and more
Nestlé has Ozempic plans
I can hear your diabetes
Pfizer doubles the price of Paxlovid
Meanwhile
B12 and inflammation
Speedier approvals
They think this is uplifting but it sounds horrific
October 19, 2023 ✒ Andrew Kantor
High blood pressure is bad, and it seems that so is changing blood pressure. Significant fluctuations in BP can lead to dementia and other cognitive impairments, according to a new Aussie study. At the same time, they also found that higher variations in systolic BP (i.e., “the top number”) was linked with arterial stiffness. “These results indicate that the different types of BP variability likely reflect different underlying biological mechanisms, and that systolic and diastolic blood pressure variation are both important for cognitive functioning in older adults.” So it’s worth A) taking your blood pressure frequently, and B) learning to spell sphygmomanometer. In today’s first entry for “drug for X also treats Y,” we have amitriptyline, the antidepressant. It can also treat irritable bowel syndrome. And not just a little bit, either. “[P]atients taking amitriptyline were almost twice as likely to report an overall improvement in symptoms as those taking a placebo,” according to the British scientists who published their findings. Wondering why? According to one pharmacist, it’s not surprising that an SSRI would affect IBS: “With 90-95% of serotonin production occurring in the gut, it would seem viable that the gut can be affected by a regular dose of amitriptyline.” And in today’s second entry for “drug for X also treats Y” comes DHA (dihydroartemisinin), the malaria drug that — as predicted by one of our coming AI overlords — treated osteoporosis in mice by reducing their bone loss and preserving the bone structure. The Chinese scientists who did the study used an AI to predict what kinds of molecule might tweak the right genes to get the body to build up its bones. And apparently that AI got it right. Two caveats, though. First, it was in mice, and (with a few exceptions) mice aren’t people. Second, it wasn’t just popping a pill — they delivered the DHA directly to the bones using nanoparticles. (And because the effect was predicted by an AI and uses nanotech, they get a double-buzzword score.) Everyone knows that melanoma is the deadlier kind of skin cancer. Apparently, though, everyone is wrong. Well, sort of. A new study out of France finds that while melanoma is deadlier in a head-to-head comparison with non-melanoma skin cancer, the latter has a lot more heads to compare. (Link is a PDF.) In 2020, [non-melanoma skin cancer] accounted for 78% of all skin cancer cases, resulting in over 63,700 deaths. In contrast, melanoma caused an estimated 57,000 fatalities in the same year. It’s been a long time coming, but the FDA is proposing to ban “formaldehyde and other formaldehyde-releasing chemicals (e.g., methylene glycol) as an ingredient in hair smoothing or hair straightening products’ — the kind used by a lot of Black women. The agency has been warning about the chemicals for a while because they can cause a host of health issues especially if they’re breathed in (e.g., when heated in a poorly ventilated space). It’s also a carcinogen. It’s also been considering a ban for the last seven years but only got around to formally proposing it now. Yellow fever. Yep, a warming climate means the mosquitoes that carry it are movin’ on up to the southern US. We’ve already seen homegrown cases of malaria, so it’s not entirely surprising. And there have been outbreaks of other diseases carried by the Aedes mosquito in the South. The good news is that there’s a vaccine. The bad news is that we don’t have a stockpile of it, so a serious outbreak “could tear quickly through unimmunized populations across the American South, and it is unlikely that the U.S. government would be prepared to acquire and distribute vaccines in a timely manner.” A doctor in Virginia prescribed a woman a cat to treat her depression. (Spoiler: It worked. Teaser: It worked in the most tear-jerky way possible.) Amazon is launching (ha!) drone delivery of prescriptions in College Station, Texas, before a planned expansion to other cities. Artist’s conceptionFeline depression fix, variable BP danger, two repurposable meds, and more
For BP, flexibility is bad
Treating the gut (and depression)
Fighting bone loss (and malaria)
Quantity over ‘quality’
Formaldehyde on the chopping block
The next next thing to worry about
Short takes
That’ll be in aisle 3
Drugs getting high

October 18, 2023 ✒ Andrew Kantor
Got patients with skin conditions? You might ask them how they’re sleeping. A new study found that itching and burning didn’t just keep people from falling asleep, it also reduced the quality of that sleep. ‘[P]atients with skin disease experienced a feeling of fatigue more often upon waking up; periods of drowsiness during the day; tingling sensations in the eyes; and repeated yawning.’ So they might not realize the connection between being tired the next day and the fact that their skin condition is affecting them while they sleep. After “Unfortunately, I think, rather than serve as a warning to the rest of the industry, this lawsuit created an opportunity for competitors by weakening Purdue’s marketing grasp over its lucrative OxyContin prescribers.” The NCPA Foundation named GPhA’s own Jonathan Hamrick its 2023 Outstanding Faculty Liaison of the Year. Congrats, Jonathan! We could’ve run the pic of him dancing at convention, but …. CAR-T cells are pretty good at finding leukemia or lymphoma cancer cells, but when it comes to solid tumors they get lost. So Columbia U biologist engineered a bacteria that would find the cancer and “paint solid tumors with a synthetic marker that the CAR-T cells can recognize.” (That synthetic marker is a antigen, making this “the first example of pairing engineered T cells with engineered bacteria to deliver synthetic antigens safely.”) Next up, hopefully, are clinical trials. This time it’s scientists at UPenn weighing in, and their hypothesis is that long Covid is caused by [spins wheel] low serotonin levels. [S]erotonin reduction is triggered by remnants of the virus lingering in the gut. Depleted serotonin could especially explain memory problems and some neurological and cognitive symptoms of long Covid, they say. Even better, they think this could be the Grand Unifying Theory of long Covid. …the biological pathway that their research outlines could unite many of the major theories of what causes long Covid: lingering remnants of the virus, inflammation, increased blood clotting and dysfunction of the autonomic nervous system. “All these different hypotheses might be connected through the serotonin pathway.” So the obvious next step: a clinical trial with Prozac (really). Here’s an unexpected connection: If you have older siblings and have had your tonsils removed, you’re at a greater risk for a form of arthritis called ankylosing spondylitis. In fact, the more older siblings you have, the greater the risk: 18% higher for one older sibling, 34% for two or more. But there’s a good reason: infection. If you need your tonsils removed, there’s a good chance you’ve been exposed to something nasty. And the more older sibs you have, the more exposure you’ll get to various bugs. So no, getting your tonsils removed isn’t the risk factor. Needing them removed is. The study found the correlation — infection as a child can mean arthritis as an adult — but haven’t teased out the cause. Yet. A monkey with a kidney from a genetically engineered pig survived for two years without rejecting the organ. [T]he researchers edited 69 of the pig’s genes. Three were involved in producing rejection-related molecules and 59 were related to retroviral DNA that became embedded in the pig genome many generations ago. The final seven involved adding human genes that are known to promote healthy organ growth, such as by preventing improper blood clotting. Not surprisingly, “The researchers suggest that they are on the right track, but more testing is required.”Another long-Covid idea, itching to stay awake, the tonsil-arthritis connection, and more
Itchy, Scratchy, and bad sleep

Nature abhors a marketing vacuum
Fortunato Purdue Pharma got into the crosshairs of states and the federal government, it made the smart choice to dial back the marketing of OxyContin. But its competitors might have gotten the wrong lesson. Instead of trying to lay low, they increased the marketing of their own opioids.High-five to Hamrick!

Painting a target on tumors (with bacteria)
The latest long-Covid explanation
Siblings, tonsils, and arthritis
ICYMI
October 17, 2023 ✒ Andrew Kantor
There are people who take and hoard antibiotics without a prescription — pills they’ve saved, gotten from someone who didn’t finish a course, or bought overseas. Why? Because of “personal beliefs” (i.e., they wanna) but more specifically it’s “based on past treatment experiences and health care system barriers.” In other words, they couldn’t get them when they needed them. Interviewees struggled with getting transportation to appointments, paying for parking and affording the associated costs of doctor visits. Many patients opted to use nonprescription antibiotics because they are more convenient than visiting a clinician and are easier to obtain and afford. Interestingly, the authors of the paper say what’s needed is education on antibiotic resistance, rather than, I dunno, helping people overcome the barriers to care. Not that it’s a surprise; we’ve been covering the road here for a while. But now it’s official. The company already has $3.45 billion in new financing, and it named a permanent CEO (one Jeffrey Stein). One of the requirements of the process wins the Euphemism of the Week award: “Accelerate the company’s store footprint optimization plan.” The Walgreens walkout that was expected last week has been moved to late October, as pharmacists work to coordinate the effort … and hope they and the company will reach an agreement before that happens. The Walgreens organizer said they have been in talks with pharmacy staff from other retail chains about participating in the group walkout. The person sees nationwide walkouts across several retail pharmacy chains as the “next step” in the fight against current working conditions. The FDA has decided it might be time to regulate CBD-based products, or at least think about thinking about regulating it. But to ensure the process moves as slowly as possible, it’s turned to Congress for advice and permission. [Owen] McMaster* explained FDA has received several citizen petitions requesting that the agency allow CBD products to be regulated as dietary supplements. “Unfortunately, the existing regulatory frameworks that we have for foods and supplements are not appropriate for CBD. It’s not apparent how CBD products can meet the safety standards for dietary supplements or food additives,” he explained. The problem is that the agency can’t actually regulate CBD products until Congress gives it the authority. So until then, to quote Cole Porter, anything goes! * He is “a senior pharmacology/toxicology reviewer with the Division of Pharm/Tox for Infectious Diseases (DPT-ID) in the Office of Infectious Diseases (OID) in FDA’s Center for Drug Evaluation and Research (CDER)” and a man with a very large business card. By declining to hear a case challenging the FDA’s power to ban flavored e-cigarettes, the Supreme Court has effectively given its approval to the agency’s regs. The FDA has been banning sales of flavored vapes unless the companies can prove that their flavored products ‘were more effective at helping adult smokers quit than tobacco-flavored e-cigarettes.’ Methotrexate is already used for rheumatoid arthritis and psoriatic arthritis, and now Aussie researchers found it works for hand osteoarthritis, too. It’s not a huge, game-changing drug, but it helps: “A 20mg weekly oral dose over six months had a moderate effect in reducing pain and stiffness in patients with symptomatic hand OA.” They noticed it took a few months to really work, but from three to six months the pain levels decreased — and looked like they would continue to decrease. Prescribers can prescribe it now, of course, but you know the mantra: More research is needed… … “to establish whether the effect of methotrexate extends beyond six months, for how long we need to treat patients, and whether methotrexate reduces joint damage in patients with hand osteoarthritis and associated inflammation.” It’s an interesting correlation: From 2006 to 2019, kids with type 1 diabetes have been prescribed a lot more psychotropic meds — stimulants, anxiolytics, SSRIs, and more. The researchers found that psychotropic medication dispensing increased from 0.85 to 3.84 percent among children and from 2.72 to 13.54 percent among adolescents with T1D, consistently higher than their peers without T1D. Why? They don’t know. “These findings call for further in-depth investigations.” A big stumbling block to acne treatments is getting patients to use it every day. To counter that, a group of American researchers have developed a weekly topical treatment made from the powdered form of a freshwater sponge called Spongilla lacustris. (Apparently it’s been used for inflammation since the 1700s.) Called DMT310 and tested on teenagers for 12 weeks in a phase 2 trial, the “once-weekly topical treatment significantly reduced both inflammatory and noninflammatory lesions” with no notable side effects. Next up: a larger, phase 3 trial.Acne-fighting sponge, why people hoard antibiotics, SCOTUS rules for FDA, and more
Antibiotic hoarders
Chain-pharma news
Rite Aid formally declares bankruptcy
Walgreens pharmacists plan late-October walkout
Scholarship applications are open!
FDA considers CBD
FDA can regulate e-cigs: SCOTUS
Give a hand to methotrexate
Diabetic kids are getting lots of brain meds
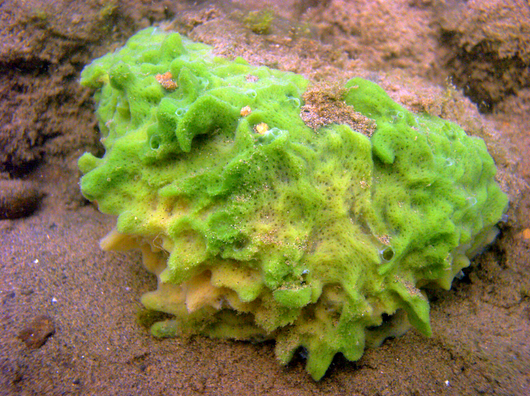
Acne is sponge-worthy
October 14, 2023 ✒ Andrew Kantor
As a matter of fact … maybe. But not the over-the-counter pills — it requires sodium ascorbate, according to the Aussie researchers who tested it in a small trial. They added that into the bloodstreams of 30 sepsis patients “resulting in promising improvements to multiple organs.” (To answer the obvious question: The placebo group got standard treatment for sepsis. They didn’t not treat them.) The study found that patients with sepsis who received the sodium ascorbate treatment: Next up: a 300-patient trial. One way to make chemo treatments more targeted is to create a version of cisplatin that carries a second drug with it. The cisplatin sticks to the tumor, and the second drug is a light-activated med called a PDT. Once the PDT is brought to the tumor, doctors use a laser to activate it. That’s a great idea, but it only works on the surface of the tumor. So scientists in Hong Kong came up with a similar idea, but one that uses ultrasound. Unlike light, the sound waves can penetrate so the drug can be activated throughout the tumor. Working with cancer cell cultures in their lab, the researchers created a small-molecule platinum-based prodrug called cyaninplatin, which gathered at the tumor sites. […] They then beamed the cyaninplatin with highly-targeted ultrasound waves, which converted it to carboplatin, a common chemotherapy drug. This induced tumor death by damaging the mitochondria inside the cancer cells. Bonus: The drug combo also fluoresces, so it can help map the details of the tumor. Nifty! Apparently a whopping 40% of college-aged women tested positive for HPV infections within 2 years of starting a heterosexual relationship. That’s the result of a two-year study by Canadian researchers. HPV often clears up on its own, but persistent infections can lead to cervical cancer. Why use just one acne med when three will do a better job? Specifically a “combination gel containing clindamycin phosphate 1.2%, adapalene 0.15%, and benzoyl peroxide 3.1%” that Henry Ford Hospital researchers call IDP-126*. Patients with serious acne saw a 50% success rate with IDP-126 compared to 20–25% of the placebo group, and “significantly greater absolute mean reductions in both inflammatory and noninflammatory lesions.” (Side note: Eew.) And since all three meds are already approved, it’s just a matter of combining them. Compounders, take note. * Also the name of a droid in an upcoming Star Wars movie So, remember that game of Whack-a-Mole we all played with Covid-19 and its seemingly endless line of variants? The ones that took the “new year, new me” mantra a bit too seriously? Harvard Medical School and University of Oxford teams might just have developed a way to see which mole (or, erm, variant) is gonna pop up next. Meet EVEscape, the new artificial intelligence kid on the block. She’s not predicting your next terrible relationship choice, but she IS forecasting the future moves of viruses. If EVEscape was around at the start of the pandemic, she’d have been like “Called it!” on all the major Covid-19 variants. And she’s not a one-trick pony — she’s got insights on other viruses like HIV and influenza too. How does this work? Well, think of it as two key ingredients in a virus prediction cocktail: 1) A model predicting the virus’s next evolutionary move (think of this as the bartender) and 2) Lots of intel about the virus itself (the cocktail recipe). Mix ’em together, and voilà: you’ve got a pretty good guess at the virus’s next step. In a recent experiment, the researchers played a bit of “What if?” They sent EVEscape back to January 2020 to see how she’d fare against the actual pandemic. Not to brag, but she did pretty darn well, often better than real-world experiments. Now, with all these insights, the big goal is to design “future-proof” vaccines. Instead of always playing catch up with a mutating virus, why not be a step ahead? It’s like having a cheat sheet for a test, but instead of acing History 101, you’re saving lives. So, while we can’t predict your next life choice (or whether you should cut bangs during a lockdown), with EVEscape, we’re getting closer to anticipating a virus’s next move. Cheers to that! Big twist: That entire summary, including the headline, was written by an AI and pasted in verbatim. Yes, I am well aware that I’ll soon be out of a job. “Pharmacist shortages and heavy workloads challenge drugstores heading into their busy season” Pancreatic tumors are very good at finding new food sources when one gets cut off. If they rely on the amino acid glutaminase for making food, drugs that block glutaminase just trigger the tumor to find a different source. Regardless of the source, the tumor’s goal is to find glutamine, so a team out of NYU came up with a idea. Instead of trying to block the glutamine-seeking process, they made a drug “designed to starve cancer cells by mimicking glutamine, so that unlike glutaminase blockers it broadly inhibits all metabolic pathways that use glutamine.” They replaced the tumor’s normal food source with a fake one. But pancreatic cancer has one other trick: It can turn to sources other than glutamine, but there’s a drug for that — trametinib. Adding trametinib to the new drug “further improved survival in pancreatic cancer mouse models.” More testing is in order, of course. Cannabis use can result in more hospitalizations. A-ha! some of you might think, we knew legalization was a bad idea! But there’s a twist. It seems that marijuana legalization actually causes a drop in hospitalizations. It’s marijuana commercialization that’s the problem. Making pot legal — i.e., removing the criminal aspect — was good from a public health standpoint, according to Canadian researchers. But when pot began being sold commercially, hospitalizations for issues like cannabis-induced psychosis went up. The period of legalization with restrictions was associated with a gradual monthly decrease of −0.06 in hospitalizations due to cannabis per 100,000 individuals. During the commercialization period, which coincided with the Covid-19 pandemic, there was an immediate increase of 0.83 hospitalizations due to cannabis per 100,000 individuals. This information will certainly ensure that lawmakers consider the nuances of marijuana legalization rather than have knee-jerk reactions one way or the other.Cannabis-legalization twist, variant-predicting AI, possible sepsis cure, and more
Can vitamin C cure sepsis?
The sound of better chemo
Mothers don’t let your children grow up without the HPV vaccine
Acne three-fer
Shaken, not stirred: AI’s new recipe to forecast virus variants

News shocker
We replaced your tumor’s food source with Folger’s Crystals
Cannabis legalization vs commercialization



