March 01, 2023 ✒ Andrew Kantor
The DEA wants to go back to pre-pandemic rules that severely limited telehealth visits where controlleds were prescribed. After three years of getting comfy with telehealth, the change, if approved, would require more in-person visits in order for physicians to prescribe C-II drugs like Adderall or OxyContin. Some drugs would only require an initial in-person visit, while others would require one every 30 days. That could mean people who may seeking treatment from a doctor who is hundreds of miles away need to start developing plans for in-person visits with their doctors now. […] Patients will have six months to visit their doctor in person when the regulation is enacted. After three years, though, telehealth has boomed, and it gets high marks from both patients and prescribers. Throwing a regulatory wrench back into the works is likely to get some serious pushback. That’s right! Today’s the day — register now to grab that early-bird rate for the 2023 Georgia Pharmacy Convention, June 14–18 at the Omni Amelia Island Resort! Once upon a time, generic drugs were quick to grab 80% of the market — within a few months, in fact. But today, according to a report from the Association for Accessible Medicine, “many generics are experiencing slower than expected adoption.” Even the top 10 generics only had a 70% market share. That means patients end up with higher co-pays when a less-expensive alternative is right there in front of them. So, who is stalling the move to generics? The answer starts with “P” and ends with “armacy benefits managers.” As the AAM put it, “These delays are driven by the perverse incentives of PBMs to prefer high-priced drugs with high rebates over drugs with lower list price.” It’s not just patients; it’s taxpayers, too. Fewer than two-thirds of Medicare Advantage and Part D plans cover the new generics that debuted in 2016. (Commercial plans did a bit better, covering almost half of those new-in-2016 generics.) And PBMs go to great lengths to keep generics down. CVS, the report explains, used a “do not substitute” strategy “that allegedly prevented consumers from obtaining low-cost generics if the company profited through rebate agreements from the brand drug.” To compound matters, the company allegedly trained call center representatives to mislead patients on pricing for the generic options and to discourage beneficiaries from filing formulary exceptions. And the company executed the scheme by refusing to stock the generic versions in its pharmacy, even for patients willing to pay cash. The same doctors who pushed ivermectin as a Covid cure (hint: it’s not) are now saying the horse dewormer can — miracle of miracles! — treat flu and RSV, too*. Apparently there’s a huge worldwide conspiracy to keep this fact from the masses. Or maybe there’s simply no evidence at all, and the docs doing this are making bank charging gullible people hundreds of bucks to write them prescriptions. From Penn State: Researchers have developed a blood-plasma test that can detect and track glioblastoma tumors by measuring levels of an antigen receptor called IL13Rα2. They found that IL13Rα2 can serve as a biomarker for glioblastoma because it’s “significantly overexpressed in tumor tissue.” The test is meant to give physicians more information about the progress of a tumor than can be had with an MRI or CT scan, or even from a needle-sized biopsy. From Australia’s University of Technology Sydney: Instead of a biopsy, Aussie biomed engineers have developed a “static droplet microfluidic device” that can “rapidly detect circulating tumour cells that have broken away from a primary tumour and entered the bloodstream.” It’s based on the idea that tumor cells produce more lactate than healthy ones, but this device is crazy sensitive — “38,400 chambers capable of isolating and classifying the number of metabolically active tumour cells” in a single, small device. When a breakthrough cure enters the market — a cure, not just a treatment — it can cost … well, a lot. Insurance companies will often (reluctantly) pay for high-priced treatments, but that’s becoming an issue with cures. Cures cost more, but over 10 or 15 years they’re cost-efficient for insurers … but only if the patient stays with the same payor. (Otherwise the cost savings goes to the new insurer, which doesn’t have to pay for treatment.) Will we ever know for sure? Probably not. An unclassified intelligence briefing gets to the heart of the matter: China’s cooperation most likely would be needed to reach a conclusive assessment of the origins of Covid-19. Beijing, however, continues to hinder the global investigation, resist sharing information and blame other countries, including the United States. Sources: A Forbes overview of who thinks what. The Atlantic’s coverage of the debate. An unclassified intelligence briefing for the president. Also helpful: a Forbes timeline of the theories. “Personal Psychedelic Use May Be Common Among Psychedelic Therapists” For the first time, pharmaceutical companies are spending more than half their ad budgets on digital advertising, relegating traditional “linear TV” to second place. Georgia pharmacies — and a UGA professor — are featured in a WSB news story about the medication shortages facing patients, some of whom have to pharmacy hop to find their meds. Therapists trip themselves, PBMs block generics, DEA targets telehealth, and more
DEA wants to slash tele-health prescriptions
Convention registration is open!

Visit gphaconvention.com for all the details (the site is being updated as you read this, in fact) — and we’ll see you on the beach!Who’s blocking the generics?
More ivermectin follies
* It’s also a floor wax and tasty dessert topping.
New tests for cancers could be coming
The Long Read: Breakthrough Drugs, Break-bank Pricing edition
Everything you need to know about the Covid-19 lab-leak vs natural-origin theories
* Dang, we have a lot of those.
Captain Obvious tastes the rainbow
Short Takes
Pharma puts its money in digital
Med shortages, Peach State perspective
February 28, 2023 ✒ Andrew Kantor
Antidepressants are often prescribed for people with bipolar disorder, but some of them may do more harm than good (the drugs, not the people) (although it’s true for the people, too, I suppose). Certain antidepressants can increase “mitochondrial energetics,” says a research team from the Mayo Clinic, and when given to a bipolar person, “may elevate the risk of treatment-emergent mania.” In other words, if we were still calling it “manic depression” these meds would turn that manic part up to 11. The increased energy expenditure of mania associated with impulsivity, poor judgment, psychosis, and loss of insight can drive high-risk behaviors, often resulting in hospitalization or incarceration. But which drugs might cause that? There’s the rub — they aren’t sorted that way. “These data suggest categorizing antidepressants based on mitochondrial energetics may be of value.” Would you recognize the signs of mental illness or substance abuse if they weren’t incredibly obvious? Face it: probably not. But catching those signs early is critical to getting patients on the right path. That’s why the Georgia Pharmacy Foundation is offering an important CE course: Mental Health First Aid. It’ll teach you to identify and respond to signs of mental illnesses and substance abuse sooner rather than later. The course: 5½ hours live training, plus 2 hours self study — a total of 7.5 hours of CPE credit for pharmacists and technicians. (You’re expected to complete the home study portion first.) The next date: Saturday, March 18, from 9:00 am – 3:30 pm on the UGA CoP campus in Savannah. GPhF is making this training available to pharmacists, pharmacy techs, and student pharmacists for just $49.00. (It’s normally $170.00.) Be ready to recognize and help the people who need it. An experimental form of HIV PrEP is being tested at the University of Pittsburgh — a combination of tenofovir alafenamide and elvitegravir that’s not a pill. If it entered the market, it would be a form of on-demand protection, rather than the daily dose of oral drugs like Truvada and Descovy. (To be fair, those are often taken on-demand as well, although that’s still off-label.) So far the tests have been small-scale (21 people) and in the lab, but they’ve been promising. That’s not surprising, considering that oral antivirals have been shown to be 99% effective in reducing HIV risk. The ultimate goal, say investigators, is to add yet another PrEP delivery method to the growing menu of oral and injectable options that at-risk men and women can use. Has Merck been playing games with the patent system to protect Keytruda from generic competition? The Senate, led by Senator Elizabeth “Don’t Mess With Consumers” Warren, thinks so, and it wants the U.S. Patent and Trademark Office to look into it. In short, Merck keeps tweaking Keytruda without actually changing the basic drug. As the company put it, it’s creating “innovations around composition of matter, method of use, formulation, dosing and combinations with other agents.” Which is fine, except when (Warren et al. say) it’s trying to use minor tweaks — e.g., a subcutaneous injection formula — to extend its patent on drug itself. In fact, they pointed out, 74% of Merck’s new patents on Keytruda cover “different indications and formulations of the drug, not the key antibody.” “These efforts by Merck appear to be part of a long-standing pattern of drug manufacturers’ abuse of the patent system,” they wrote, adding that Merck’s use of patents is “an example of anti-competitive business practices.” Big news! The Energy Department apparently has low confidence that the SARS-CoV-2 virus likely originated in a lab leak. Why yes, the words “likely” and “low confidence” make the entire conclusion confusing, but it makes for headlines. (The Wall Street Journal breathlessly reported “Lab Leak Most Likely Origin of Covid-19 Pandemic, Energy Department Now Says,” not mentioning the “low confidence” part till later.) Other agencies had similarly low confidence the virus spread naturally, although the FBI said it had moderate confidence it came from a lab leak. The one thing everyone seems to agree on is that, even if it was a lab leak, it was accidental. Still, it’s critical that we spend more time and money arguing over its origins. Once we’re confident we know how it happened, we can … I dunno. Write a strongly worded letter, perhaps. Swedish materials scientists have grown electrodes in living flesh (of a fish, for starters), but by using the fish’s own sugars to build the electrodes inside itself without damaging tissues. The result, published in the journal Science, paves the way for the formation of fully integrated electronic circuits in living organisms. What they hope: These might be used for brain therapies to treat conditions like Parkinson’s or even to advance prosthetics. What the reality will be: The FDA has authorized Lucira Health’s combo flu and Covid test. It takes about 30 minutes, uses a shallow nasal swap (thank you!) and is about 90% accurate for both. Note: It’s been describe as a “major milestone,” but not a game-changer. One booster a year will (probably) be enough, even for the immunocompromised, according to the CDC’s Advisory Committee For Immunization Practices. The current CDC recommendation is that at-risk folks get more frequent boosters, so this would be a change … although the ACIP did say some flexibility is important, especially as we see what new variants might be in store. The viruses that killed one person and sickened another in Cambodia are from an endemic clade of bird flu — i.e., it’s not some new variant that will soon sweep the globe and lead to a new crop of post-apocalyptic video games. It’s one that’s been “among birds and poultry for many years and has sporadically caused infections in people.” Swedish fish cyborg, Merck patent shenanigans, antidepressant bipolar concerns, and more
When antidepressants cause mania

A different PrEP delivery
Playing with patents could mean pending penalties
ICYMI: Moderately confusing
Today’s non-pharma, cool science story

Short Takes
Double-duty OTC test
One booster will do the trick
Whew! Nothing can go wrong now.
February 25, 2023 ✒ Andrew Kantor
Did you ever look out your window, daydreaming about what’s the best treatment for acute lower-back pain? Of course you have. Now there’s an answer: If it’s not caused by something specific (e.g., cancer, kidney stones, YouTube comments) the best pharmaceutical treatment seems to be a combination of NSAIDs, acetaminophen, and myorelaxants. So say a group of German and Italian researchers in a systemic review of lots of literature, looking for the best non-opioid solutions. What they found: NSAIDs alone work great, and myorelaxants alone work to some extent, but acetaminophen doesn’t do much unless it’s combined with NSAIDs. And there you have it. Back to daydreaming. Have you had any run-ins with superbugs outside of Kafka novellas? If you’ve dealt with antibiotic-resistant infections, the Partnership to Fight Infectious Disease (PFID) wants to hear from you. It’s collecting stories from healthcare providers for its Squash SuperBugs Day in March, and so far doesn’t have anything from pharmacists. If you or someone you know is willing to share your story of dealing with — professionally or personally — drug-resistance, please share! Just click here for the handy-dandy (and short) form. (If they use it, you’ll be able to approve it before it appears on the site.) Could we be wrong about insulin’s chemistry? Those shifty Danes think so. They’ve discovered that “we’ve gotten things wrong by 200 percent” when it comes to the distribution of molecules in an insulin shot. Insulin divides itself into either single molecules (which work quickly) or clumps of six (which are long-acting). That’s why a dose does double duty, and the ratio is taken into account by manufacturers. Oopsie, said the Danes. “There are only half as many single molecules in insulin compared to what we thought. Conversely, there are far more six-molecule clusters than we assumed.” That means it might not be working the way we expect. That isn’t necessarily dangerous, but it does mean we can do better. “[O]ur results may mean that when we believe to be administering a certain dose, it may mean that insulin behaves in a different way than expected and that even better insulin therapeutics can be developed.” Cosmetics fall into a loophole of regulation — they aren’t covered by either the FDA or the EPA, so manufacturers are free to put all sorts of unhealthy stuff into them. With the feds not being willing to regulate them, states are stepping in. Washington, for example, “…found lead, arsenic, and formaldehyde in makeup, lotion, and hair-straightening products made by CoverGirl and other brands.” The state legislature is considering a bill that would ban toxic ingredients in cosmetics. Of course, once enough states start banning those ingredients (they’re already banned in Europe), the cosmetic companies will likely remove the chemicals across the country … and make a big deal about how safe they’re making their products. Ogilvy Health has rated 10 pharma companies’ social media efforts using its own six-category scale. Whoopdie-do, you say. Fair enough. But what’s worth noting is how Ogilvy rated each of those six areas. The report is effectively a primer in making social media work for you, including branding, response time, mobile design, and more. Check out the full report here — it’s 10 pages of content squeezed into a 36-page PDF. Should you be worried about bird flu (other than because you have chickens)? Maybe? Some recent headlines: Insulin misunderstanding, cleaning up makeup, back pain relief, and more
The best drugs for back pain
Looking for superbug stories
Our insulin mistake
States aim to detox makeup
A pharma social media guide
Unfriendly skies?
February 24, 2023 ✒ Andrew Kantor
CMS is beginning the process of choosing Medicare’s 10 most expensive drugs — the medications it now has the power to negotiate the prices of*. It’s not entirely simple; the agency first has to decide whether it will use gross or net spending (the latter considers discounts). Then it will look at total spending over a year and determine the top 10. CMS said in January it would announce the list of 10 drugs in September. The agency will make its initial offers in February 2024 and the negotiation period will end that Aug. 1. Capitalism at work: The buyer and seller will come to an agreement on pricing, which will take effect on January 1, 2026, saving taxpayers billions. Who would have thought that taking laxatives regularly could raise your risk of dementia? Yet here we are. In fact, found researchers in China and Boston, using them “most days of the week” increased dementia risk by 50 percent. And those who used multiple types of laxative had an even greater risk — 90% higher than non-users. The big disclaimer: “The study does not prove that laxatives cause dementia. It only shows an association.” Afraid of the Ex-Lax now? No worries — gastroenterologists at the Medical College of Georgia have the solution. CMS said no, it’s not changing its stance on Alzheimer’s drugs. Medicare will only pay for drugs that have been approved through the FDA’s standard process, not the accelerated process. Specifically, it’s not going to pay for Aduhelm or Leqembi. The Alzheimer’s Association immediately made it political, of course, but the reason behind the decision is simple: Neither drug has shown it makes a huge difference in the real world, which CMS said it requires to determine that a medication is “reasonable and necessary.” CMS will expeditiously review any new evidence that becomes available that could lead to a reconsideration and change in the [national coverage determination]. In the beginning, remdesivir was the go-to treatment for Covid-19, but it didn’t always work, and now we’ve got better stuff. (“Stuff” being nirmatrelvir/ritonavir, aka Paxlovid.) But we never figured out why it only worked part of the time. Enter the Swiss. University of Basel researchers wanted to know when remdesivir worked and when it didn’t. What they found was that “a specific group of patients benefits the most from the drug.” What group? People who got, at most, conventional oxygen therapy. If they needed intensive ventilation support, it didn’t seem to help because the infection was too serious. Will this make a difference? Probably not, with Paxlovid the go-to these days, but it does mean that remdesivir is worthwhile in milder cases. The FDA warned vape makers not to sell illegal products because, you know, they’re illegal. Most of the time the industry just ignores the law, but now the agency is showing how tough it is … by fining four smaller companies (of the 120 it warned more than a year ago) for ignoring the rules. It kinda makes sense when you think about it: Wearable fitness devices like smartwatches that use electrical impedance (i.e., tiny electrical currents) to measure things like heart rate can interfere with pacemakers and other implanted cardiac devices. “Bioimpedance sensing generated an electrical interference that exceeded Food and Drug Administration-accepted guidelines and interfered with proper CIED [cardiac implantable electronic devices] functioning.” Ex-Lax of doom, Apple Watch dangers, CMS rejects Alzheimer’s Association, and more
Choosing the most expensive drugs
* “… the prices of which it now has the power to negotiate” if you’re a Latin speaker
So many bad-pun headlines to choose from
So what can you do?
CMS rejects paying for Aduhelm or Leqembi — again
When remdesivir works
FDA on the attack (kinda)
Non-pharma interesting medical story of the week
February 23, 2023 ✒ Andrew Kantor
The bad news: 59% of Covid patients experience organ damage in their heart, kidneys, liver, lungs, pancreas, and spleen, and it continues up to a year after infection according to a new British study. The good news: It’s typically mild. The organ damage, that is. But… While 59% of them experienced impairment in a single organ, 29% were found to have multi-organ impairment one year after a Covid infection. The other good news — sort of — is that between six months to a year later, the number of patients suffering from various Covid-related ailments dropped a bit. (A bit. We’re talking 10 to 12 percent.) So … yay? ICYMI, Reckitt has recalled two batches of its Enfamil ProSobee Simply Plant-Based Infant Formula “because of possible cross-contamination with Cronobacter sakazakii bacteria.” These are 12.9 oz. containers of powder. Per the Georgia DPH: Recalled product batches are ZL2HZF and ZL2HZZ, both with a UPC code of 300871214415 and a “Use by Date” of “1 Mar 2024.” So you know the psoriasis drug apremilast (aka Otezla)? Turns out it can also treat — wait for it — alcohol use disorder. Yep. People taking it “reduced their alcohol intake by more than half — from five drinks per day to two,” according to Oregon Health & Science University neuroscientists. They found the connection by looking for compounds that might “counteract the expression of genes known to be linked to heavy alcohol use.” Apremilast, oddly enough, was one of those compounds. They tested it in mice, then in humans. They found that apremilast triggered an increase in activity in the nucleus accumbens, the region of the brain involved in controlling alcohol intake. Of course, you know the drill by now: More research is needed, including seeing its effect on people who want help vs. those who don’t. Diabetics are more likely to suffer hip fractures thanks to osteoporosis, but Taiwanese researchers found a surprising preventative: statins. They looked at the health records of more than 188,000 people with type 2 diabetes and divided them into a statin group and a non-users group. They found … … 1.48% of the statin group and 3.17% of the nonusers sustained a hip fracture. Adults who used statins had a lower risk for hip fractures than nonusers. Men were less likely to sustain a fracture than women. So there weren’t a lot of hip fractures, but statin users were still half as likely to suffer one. (And get this: They also found that the higher the dose, the lower the risk of hip fracture.) A fifth person has been cured of HIV. A 52-year-old German man — “the Dusseldorf patient” — was treated with stem cells a decade ago and hasn’t taken HIV meds for four years. The virus is gone from his body, and now the people treating him have declared him cured. “It’s really cure, and not just, you know, long term remission.” Howzit work, you ask? In brief, the stem-cell donors had a particular mutation that happens to delete the CCR5 protein, which HIV needs to enter cells, making them effectively HIV-proof. Lilly’s It’s official, at least for the next 20 minutes: “[T]here is enough evidence to support e-cigarettes’ use as a first-line aid for smoking cessation in adults.” Did you know Merck was a player in the Covid-treatment game? It isn’t, really, but not for lack of trying. The company’s latest setback: Its version of molnupiravir, called Lagevrio, “was not effective at cutting the risk of coronavirus infections in people living with someone infected with the virus.” Francisco Franco is still dead, and ivermectin still doesn’t help treat Covid — even at higher doses and with longer duration. But you keep testing it, Duke researchers. (In fact, there are at least 10 ivermectin studies in the pipeline around the world!) A drug to stop drinking, long-Covid organ damage, hip-hip-hooray for statins, and more
We’ll say it again: You really don’t want Covid
Vegetarian Enfamil recall

Skin pill’s surprising other use
Statins, diabetes, and hip fractures
Another HIV patient cured
Short Takes
Our short influencer nightmare is over
diabetes weight-loss drug Mounjaro is back in stock.Vape to quit
Merck slinks back into its corner
If I’ve told you once, I’ve told you a thousand times
February 22, 2023 ✒ Andrew Kantor
Lots of people have high blood pressure, and that’s ungood. A lot of them don’t even know what their blood pressure is, and that’s plus-ungood. And, it turns out, a lot of them know their BP but think it’s fine … when it’s not. Double-plus-ungood. A new study published in the journal Medical Decision Making found that while almost 64% of people said they were confident in their understanding of BP numbers, in reality only 39% actually did. With only 1 in 4 Americans having their BP under control, those “good” numbers might be worth a little reminder now and again. With Covid (mostly) behind us, it’s time to get back to the opioid crisis, which started to leave but, like Tom Brady, was just kidding after all. How convenient for you that the country’s biggest and most important healthcare conference addressing the opioid and addiction crisis is in your own backyard. It’s the RX and Illicit Drug Summit, and it’s coming to Atlanta’s Georgia World Congress Center April 10-13. Get info and register at Rx-Summit.com. If you’re infected with Covid, it’s going to give you some protection against reinfection. But how much? An analysis in The Lancet looked at 65 studies across 19 countries to find out. The answers: Don’t rush ’em. A study out of Northwestern found that getting boosted too soon will weaken the effect of the booster. The problem is that “the original Covid-19 vaccine worked so well that it actually hurt boosters given too soon by ‘mopping up’ the new shots before they can become effective.” Their conclusion: “It’s better to wait six months than two weeks before you boost.” Not getting enough sleep or, in fact, not getting regular sleep turns out to be a risk factor for atherosclerosis. It’s all about consistency, says the American Heart Association, based on “a racially and ethnically diverse study of more than 2,000 adults in six large U.S. communities.” [O]lder people who varied sleep time by an average of two hours within a single week and those who changed their bedtimes by an hour and a half were significantly more likely to exhibit subclinical symptoms of atherosclerosis. So think about that: A ‘big variation’ is varying the time you fall asleep by more than 90 minutes within a week — 10:00 on Monday, midnight on Wednesday, 9:45 on Thursday … you’re in trouble. Well, maybe. You’re “more likely to have high coronary artery calcium scores” at least. “Growing evidence exists that the alcohol industry uses a variety of strategies to influence public policy in a way that is advantageous to its own corporate interests, rather than the interest of public health.” People suffering from long Covid — notably with chronic fatigue syndrome or myalgic encephalitis — are more likely to be unemployed. In fact, among people who had Covid, 12.3% of those with long Covid were unemployed (compared to 8.7% of those without long Covid). It’s a device that warns you when you’ve been talking too much. Developed at Northwestern, it “could be a game-changer for professional singers, teachers, politicians, call-center workers, coaches and anyone who relies on their voices to communicate effectively.” Someday maybe they’ll add AI smarts so it’ll also tell you to shut up because you’re sounding like an imbecile. Why to set your bedtime, blood pressure misunderstandings, don’t rush your boosters, and more
They don’t know from BP
The (illegal) drug summit
How much protection does a Covid infection give?
About those Covid boosters
Set your bedtime or pay the price
Short Takes
Captain Obvious sips her virgin daiquiri
Long Covid ain’t good for business
Non-pharma, but notable — and a “game-changer”
February 21, 2023 ✒ Andrew Kantor
One in three parents give their kids fever-reducing meds even for low-grade fevers (below 100.4°) even though that isn’t recommended by pediatricians, according to a new national poll out of the University of Michigan. And half would give it for fevers up to 101.9°. “Some parents may immediately rush to give their kids medicine but it’s often better to let the fever runs its course. Lowering a child’s temperature doesn’t typically help cure their illness any faster. In fact, a low-grade fever helps fight off the infection. There’s also the risk of giving too much medication when it’s not needed, which can have side effects.” Curious about those pediatrician recommendations? The UMich folks have you covered. Congrats to the 79 members of PCOM Georgia’s Pharmacy Class of 2024! They just held “the most unique white coat ceremony in the history of PCOM.” You might realize why when you think about it: This is the class of ’24, whose ceremony should have been two and a half years ago — but that was 2020, when gatherings like that weren’t a very good idea. Here’s to a happy and productive future! Sure, marketers love social media for reaching the easily swayed. But they also say that social media plays a “vital role” in influencing doctors’ decisions. And those prescribers are proving them right. “[M]ore than half (57%) of doctors said they frequently or occasionally change their initial perception of a medication due to social media.” But there’s cause for hope. Prescribers aren’t getting their info from Twitter or TikTok. They’re mostly talking about Doximity and Sermo — platforms aimed at physicians, as opposed to the general kind where the riff-raff like you and me hang out. In fact, 41% of doctors reported changing their views on a medication based on content on Sermo and 33% based on content on Doximity. Horseshoe crabs have been around for more than 250 million years, and they serve an important purpose (besides creeping out people when they’re upside down): An extract of their blue blood is used to test injectable medicines and implants for endotoxins. Problem: They’re being hunted to extinction, and there’s no official standard for a replacement. Fun fact, per Wikipedia (the source of all knowledge): “Despite their name, they are not true crabs or crustaceans: they are chelicerates, most closely related to arachnids such as spiders, ticks, and scorpions.” In 1999, the CDC reported 608 deaths attributed to methamphetamine use. In 2021, that number was more than 52,000. You don’t need a University of Illinois health researcher to tell you that’s a ‘staggering increase,’ but she does anyway. What’s the deal? The deal is opioids: That U of I team “found that 61.2% of the methamphetamine overdose deaths in 2021 co-involved heroin or fentanyl.” Sometimes it’s unintentional, but sometimes it’s deliberate, as there’s a myth that opioids can blunt the bad effects of stimulants like meth. Unfortunately, a lot of opioids are being laced with fentanyl, which is often deadly. Were you thinking of letting a cyberattack destroy your pharmacy? If so, don’t — even though it’s getting easier and easier to let the bad guys mess with your data systems. With the potential for Narcan to be available over the counter, it could be more easily accessible … but it could also become out of reach for the people who need it most. What color are your veggies? Think purple. Fruits and veg that are blue or reddish contain anthocyanins that “can reduce the risk of diabetes by affecting energy metabolism, gut microbiota, and inflammation.” Docs get ‘influenced,’ you want these crabs, let the kids roast, and more
Cool it on the cooldowns
Two and a half years later…

Doctors can be ‘influenced’ too
The Long(ish) read: The Crabs We Need edition
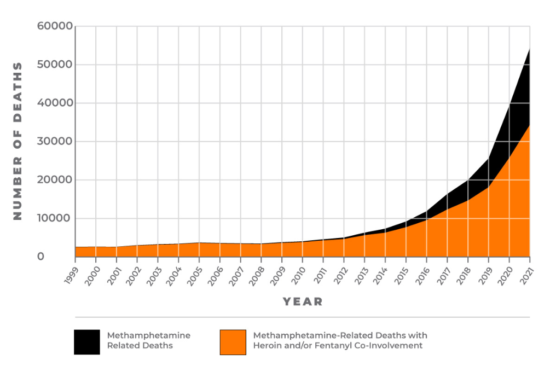
Meth deaths have skyrocketed
Short Takes
Don’t cyber-be a cyber-victim
Downsides to OTC Narcan
Purple is the new orange

February 18, 2023 ✒ Andrew Kantor
All this time we’ve been shoving swabs up our noses when — as Brazilian researchers just discovered — you can test for it just by using tears. [T]his method could be an alternative to nasopharyngeal swabbing, which is unpleasant. Indeed. The next bullet point on the list of “Things CBD Can Actually Do” could be helping people quit smoking. CBD, it seems, inhibits the metabolism of nicotine — at least according to some preliminary research out of Washington State University. As always, the mantra remains “More research is needed to confirm these effects.” It may not be a game-changer, but Pfizer says its new nasal spray for migraines is a “breakthrough.” In a phase 2/3 trial, zavegepant relieved migraine pain within a couple of hours, and the effect lasted up to two days. The FDA is already reviewing zavegepant — a company called Biohaven submitted it to the FDA last year before Pfizer bought it. If the FDA is going to approve it, that should come next month. Taking a common lateral flow assay (LFA) testing platform, engineers at Washington University in St. Louis have made them both more sensitive and faster, thanks to a bit of nanotechnology. Using “nanolabels” called plasmonic-fluors, they turned those LFAs into plasmon-enhanced LFAs or p-LFAs that can test for viral or bacterial infections. The point is: [T]he team’s p-LFAs are 1,000 times more sensitive than conventional LFAs […] p-LFAs are also substantially faster than gold-standard lab tests, returning results in only 20 minutes instead of several hours. Oh, and the test strips cost about a buck, while the scanner is about $300. Cheap. Starting trials now: an mRNA vaccine for shingles from BioNTech and Pfizer. Why bother when we already have a very good shingles vax? Pfizer and BioNTech explained in a statement that they are looking to develop an improved vaccine, with the potential for better tolerability and a more efficient global production by using mRNA technology. Good news: There’s been an 18 percent drop since 2020 in people who reported having medical debt. It’s due to a combination of pandemic-years Medicaid expansion, as well as relief fund used by local governments to help people get out from under. Bad news: Come April 1, when states can begin reviewing families for Medicaid eligibility, as many as 6.7 million kids might lose their health coverage. Georgia is one of the states that could be hit hard, as it saw kids’ enrollment in Medicaid grow by a third during the pandemic. Good and bad: Most of those kids are likely still eligible for Medicaid “but will likely lose coverage because of administrative issues, such as their parents not submitting the necessary paperwork or procedural errors” according to a Georgetown University report.Migraine nasal spray, tears for Covid tests, kids losing coverage, and more
Cry me a Covid test
CBD vs smoking
A month (maybe) to an anti-migraine nasal spray
A faster, better diagnostic test
The march of mRNA continues
Medicine and money — good news and bad
February 17, 2023 ✒ Andrew Kantor
“Moderna CEO to testify in senate on proposed vaccine price hike” — Stéphane Bancel was invited by Senator Bernie Sanders to testify “on the drugmaker’s plans to raise the price of its coronavirus vaccine.” “Moderna promises to provide vaccines at no out-of-pocket cost” — “…regardless of their insurance status, once the US government stops covering the cost of the shots.” Medication therapy management — it’s one of the best ways you can care for your patients (and get paid for doing it). A big step to providing MTM, though, is making sure you’re giving— and getting — the most you can. Patients will appreciate that, not to mention the lovely certificate on your wall. Learn how to provide the best MTM you can when GPhA presents, “APhA’s Delivering Medication Therapy Management Services: A Certificate Training Program for Pharmacists.” Sunday, March 19, 2023 8:00 a.m. – 5:00 p.m. Click here to get the details, see the instructor, and register! Could Alzheimer’s be caused by sugar? Yes, but not table sugar. University of Colorado researchers think fructose might play an important role. Their logic: Early humans’ survival response required “focus, rapid assessment, impulsivity, exploratory behavior, and risk taking” and nothing else — for example, “recent memories and attention to time” just weren’t important. That’s where fructose comes into play. When the body needs to forage, fructose activates that ‘foraging mode’: [F]ructose reduces blood flow to the brain’s cerebral cortex involved in self-control, as well as the hippocampus and thalamus. Meanwhile, blood flow increased around the visual cortex associated with food reward. All of this stimulated the foraging response. Today, high-fat/-sugar/-salt food prompts excess fructose production, triggering (they suggest) that same foraging mode — and might even explain why some Alzheimer’s patients wander off, perhaps searching for something to eat. The migraine drug lasmiditan, aka Reyvow, can treat acute kidney injury … in mice, at least. That’s per a University of Arizona study. [I]t stimulated recovery of kidney function such as mitochondrial biogenesis […], improved vascular integrity, reduced fibrosis, and reduced proximal tubule damage. Diabetics who take pioglitazone “were less likely to later develop dementia than those who did not take the drug,” according to a Korean study. The authors pointed out, though that ’The study does not prove that the drug reduces the risk of dementia for people with diabetes. It only shows an association.’ An FDA advisory panel has unanimously approved making Narcan available over the counter. Note that we said “Narcan,” not “naloxone.” That’s because the panel specifically referred to the Emergent BioSolutions version, although it seems likely that other naloxone delivery systems will eventually follow. The FDA doesn’t have to listen to the panel, which also recommended some labeling changes to simplify using the drug. The agency will make its final decision by March 29. Yet another study — this one out of Britain and published in the British Medical Journal — finds that, despite pharma company claims that high prices are needed to fund innovation, it’s just not true. The justification of high drug prices also ignores the sizeable public investments in drug discovery and development […]; more than a quarter of new drugs approved by the FDA from 2008 to 2017 were linked to public investment during the late stages of development. This means that society is potentially paying twice for new drugs, first in the form of publicly subsidised research and second through high product prices. North Carolina is on the verge of becoming the 40th state to expand Medicaid as part of the Affordable Care Act. The plan has bipartisan support and does not include a work requirement. In unrelated news, state police there are asking residents not to be alarmed by the flying pigs. Viruses jumping from animals to humans are rare, but when they do they can be … problematic. It’s led to efforts to catalog animal viruses before they spillover to humans. But what if spillovers happen frequently, but don’t often spread? Maybe we should instead be looking inside humans for the next pandemic.The fructose-Alzheimer’s connection, hunting viruses in humans, Moderna blinks, and more
Are these stories related, y’think?
Do you care? Of course you do
Live via ZoomForaging, fructose, and Alzheimer’s
Double-duty drugs
Lasmiditan for kidneys
Pioglitazone for dementia
Narcan ready for OTC
Maybe they can come up with another excuse
Elsewhere: Then there were 10
The Long Read: Virus Hunting edition
February 16, 2023 ✒ Andrew Kantor
If — with your phone in your pocket — you don’t think you’ve given up quite enough privacy, Northwestern researchers are here to help. They’ve devised “a smart neck-worn device resembling a lapis blue pendant that detects a user’s smoking.” It uses sensors to track the wearer’s throat’s heat signatures. “This goes way beyond how many cigarettes a person smokes per day. We can detect when the cigarette is being lit, when the person holds it to their mouth and takes a puff, how much they inhale, how much time between puffs and how long they have the cigarette in their mouth.” Don’t worry! Just like Google and Facebook and TikTok, “The necklace, called SmokeMon, completely maintains a smoker’s privacy.” “Will we start seeing prescription lockers at some CVS pharmacies [in Georgia]?” asks Channel 11 in Atlanta. Will they replace technicians? Drugmakers sometimes get accelerated approval from the FDA; the idea is that full trial results will come soon. But often the pharma companies conveniently forget to submit those results, or just never bother to. Now CMS has a big incentive: It’s going to pay less for drugs that get accelerated approval — until they turn in their results and get full approval. It’s a test at the moment (and there are some questions to be answered). Drugmakers, of course, are already complaining, while state Medicaid agencies have already asked that they not be required to cover accelerated drugs at all, so this might make everyone equally (un)happy. Note: The news story about this plays fast and loose with coffee and caffeine. The story is actually about caffeine. Is caffeine good or bad for your kidneys? There’s actually conflicting evidence, but now an international research group thinks it knows why. The bottom line: Half the population has a variant of a particular gene that “can result in coffee [sic] being three times more likely to cause kidney dysfunction” because they metabolize caffeine more slowly. Caffeine does have some toxic properties, and if you don’t get it out of your system quickly enough, it can cause damage. “It was remarkable to see just how striking the effects of [caffeine] were in the group that had this genetic variant, yet no effect whatsoever in those who did not.” Since the 1860s, the average human body has been dropping — it’s currently about 97.7°F. No one knew what was behind the drop. Now, though, researchers at the University of Michigan Medical School think they know. It’s gut bacteria. Of course it is. Looking at hospitalized patients, they found that the composition of a patients gut biome correlated with their fever response — specifically the presences of Lachnospiraceae bacteria. “While we certainly haven’t proven that changes in the microbiome explain the drop in human body temperature, we think it is a reasonable hypothesis. Human genetics haven’t meaningfully changed in the last 150 years, but changes in diet, hygiene, and antibiotics have had profound effects on our gut bacteria.” If you have fat mice, you want them to exercise. Pro tip: Have them do it in the morning. Swedish researchers (with some help from those shifty Danes) found… …that mice that did exercise in an early active phase, which corresponds to morning exercise in humans, increased their metabolism more than mice that did exercise at a time when they usually rest. The end of pharmacy techs? Plus what’s making us colder, anti-smoking jewelry, and more
The necklace will rat you out
The end of pharmacy techs?
CMS testing lower pay for accelerated drugs
Kidneys and caffeine: all about one gene
They do everything else, so why not?
Get up and get moving