April 25, 2023 ✒ Andrew Kantor
Oopsie — the National Academies of Sciences, Engineering and Medicine, which is supposed to be about as open and unbiased as the best of ’em — turns out to have received $19 million from the Sackler family (you know, the Purdue Pharma folks) while it was giving policy advice on the opioid epidemic. Being given money is one thing, but failing to, you know, mention this fact while making recommendations … that’s a problem. One pain researcher summed it up nicely: “It sounds like insanity to take money from principals of drug companies and then do reports related to opioids. I am really shocked.” Express Scripts says it’s going to start offering rural independent pharmacies … well, not necessarily higher reimbursement rates, but “increased reimbursement opportunities.” It will apply to independent pharmacies ‘that are the only location within 10 or more miles of an Express Scripts customer.’ So what are these opportunities for better reimbursement? This includes enhancing performance- and incentive-based programs that pay pharmacies more when they drive better outcomes, such as prescribing 90-day supplies of prescription drugs that improve adherence. The PBM also says it wants to help independent pharmacies offer more preventative services, from vaccines to testing to substance-abuse counseling. And the biggest news: It’s forming a committee to think of yet more ideas to help indy pharmacies. MIT researchers are all excited about an electronic patch that can deliver drugs through the skin. Why yes, they even call it “game-changing.” It uses battery-powered ultrasonic technology to deliver drugs as opposed to the microneedles in existing patches. What’s different? Well, it can deliver drugs to different depths in the skin, and in theory it can deliver large molecules because it uses sound to open pathways through the skin. And it works faster than microneedles: “The researchers found that their patch was able to deliver the same amount of niacinamide in 30 minutes that could be delivered with microneedles over a six-hour period.” You can hardly notice it. People over 50 are open — quite open — to cutting down on their prescription meds. They just want someone to tell them it’s okay. A new poll out of the University of Michigan found that 80% of older adults would be willing to stop taking one or more prescription meds if their health care provider said it was possible. What do they want to stop, if they can? Hypertension or cholesterol meds top the list, followed by diabetes meds and pain management. But they need someone to talk to them about their meds, their conditions, and their options. Any ideas? There’s a big downside to taking a genetic test (an APOE4 test) for Alzheimer’s risk — it might turn out you’ve got those risky genes. Yes, there are more options for earlier treatment now, but just because they exist in news articles doesn’t mean practitioners are aware of them or how to help you take advantage. [F]ew support services are available to help people deal with the implications of APOE4 testing, according to interviews with more than a dozen neurologists and genetic counselors. Alzheimer’s patients and caregivers face a shortage of genetic counselors to explain the tests and help them navigate the psychological, medical, financial and legal consequences. Before you send in the swab, think about what you’ll do if you don’t get the result you’re hoping for. What can we add to the list of “conditions caused by an imbalance in the gut biome”? How about hay fever? [R]educed diversity of gut bacteria can lead to an increased risk of hay fever makes sense since the gut microbiome plays a key role in regulating the immune system, and we know the immune system influences allergies. More and more places are going cashless — accepting only credit and debit cards to avoid the hassle of bank visits and security worries. Part of the solution: “Reverse ATMs” that turn customers’ cash into credit cards. Express Scripts wants to help, stores go cashless, NASEM’s little oopsie, and more
Oh, that money!
Express Scripts offers “opportunities”
A faster skin patch

Help them deprescribe
Sometimes ignorance is bliss
Short takes
Bless you, prebiotics
Is your future cashless?
April 22, 2023 ✒ Andrew Kantor
A test to evaluate someone’s sense of smell might also indicate whether they’ve got depression. Indian researchers, presenting at the American Physiological Society meeting, found that people who did poorly identifying smells (via the standard sniff tool called the Brief Smell Identification Test or BSIT) were more likely to have been diagnosed with depression. In fact, “All the members of the depression group identified fewer smells than the control group.” The test has 12 scents; identifying fewer than 9 is abnormal; people with “recurrent depressive episodes” averaged 5.2 scents. Boston University researchers have made an important step to controlling traveller’s diarrhea without using antibiotics that can mess with the good gut bacteria. They’ve figured out how the troublesome E. coli. bacteria attaches itself in the gut. The bacteria, it seems, “use long, thin filaments called ‘pili’ to bind to cells in the gut, allowing an infection to start.” In fact, they found, the pili will change depending on the environment. This is important because finding a way to keep the bacteria from attaching would be better than killing them. “Therapeutics that disrupt pili and allow bacteria to be washed away have advantages over current antibiotics, as physical removal would not lead to the evolution of resistant strains and only the pathogens would be targeted.” Who are you? What’s your practice area? What do you like about what GPhA is doing, and what do you wish would change? Now’s the time to let us know. GPhA’s annual member survey is online and waiting for your input! Trust me on this: Your answers are read and discussed across the association, and they really do make a difference in GPhA’s priorities over the next year. There are now two bipartisan proposals in the Senate for lowering insulin prices (“and for other purposes”). The existing one comes from Georgia’s own Sen. Raphael Warnock (and John Kennedy of Louisiana), and it “would ensure maximum costs of $35 per month for all insulin products, and would also lower costs for uninsured patients.” The new proposal, though, takes into account that pharma companies have already said they’ll lower insulin prices, and it takes that a bit further: [It] would cap insured patients’ insulin costs at $35 per month for at least one insulin of each type and dosage form, and require pharmacy benefit managers to pass through rebates they collect from insulin manufacturers to the insurance plans that employ them. It would also make it faster and easier for the FDA to consider biosimilars and for Medicare plans to get them into the hands of patients. The good news is that the proposals are similar enough that it seems they could be merged, and they both have blue and red support. For now, at least. When drug companies suddenly lowered some of their insulin prices earlier this year, the conventional wisdom was that they did it because they knew they’d have to, with new regs coming down the pike. Might as well make it sound like it was their own idea. But the reality, it seems was more complicated, as a new analysis in the New England Journal of Medicine explains. We don’t have access to the journal itself, but the folks at Fierce Pharma have done a great write-up of how “The price cuts can be explained by a mix of factors.” A CDC study — part of the National Health Statistics Reports — gives some detail about who’s using dietary supplements these days. The basics: For all the detailed details, check out the paper itself (14-page PDF). Apparently it’s not a myth — according to Aussie epidemiologists, cranberry juice really can prevent urinary tract infections. They did a meta-analysis of existing research, so Big Cranberry probably* wasn’t involved. Now, they say, there are 50 studies on the effects of cranberry products on recurring UTIs, and they point the same way: These data support the use of cranberry products to reduce the risk of symptomatic, culture‐verified UTIs in women with recurrent UTIs, in children, and in people susceptible to UTIs following interventions. Caveats: 1) They didn’t test whether cranberries were better than antibiotics or probiotics for prevention, and 2) “The data also doesn’t show any benefit for elderly people, pregnant women or in people with bladder emptying problems.” * The paper doesn’t list the source of funding, but that may not really matter for this kind of analysis. The latest drug to Plague America’s Streets is (in case you missed it), xylazine — the common animal tranquilizer that’s being used to cut heroin … and ends up killing users. The problem: As we learned from the knee-jerk reactions to the opioid crisis, knee-jerk reactions cause as many problems as they solve. As the government ponders xylazine limitations, legit users, i.e., veterinarians, are legit concerned: [A]ddressing the threat is proving to be a tricky balancing act involving stakeholders in areas as disparate as addiction medicine, commercial livestock and law enforcement. The challenge is to walk a careful line by managing a drug that is essential for veterinarians but is fueling a public health crisis.Cranberries for UTIs, scratch-’n’-sniff depression test, insulin prices explained, and more
A smell test for depression
Our number 2 story: counterattacking Montezuma’s Revenge
Don’t miss the GPhA annual survey!
One Senate, two insulin-price proposals
Speaking of insulin prices…
In case you’re curious, here’s some supplement-use data
It seems cranberries work after all
The Long Read: xylazine balancing act
April 21, 2023 ✒ Andrew Kantor
Hospitals and physicians’ offices jack up the prices of medications far beyond what they would cost at specialty pharmacies. That’s according to new data from America’s Health Insurance Plans. “See what insurance companies say” is often good advice. They tend to ignore politics and focus strictly on their bottom line, for better or worse. So when they point fingers at what’s costing them money, it’s worth listening. In this case, their data found that, of the 10 highest-cost drugs, physician offices marked up prices by $1,559 and hospitals marked them up by $8,278. “Specialty pharmacies lower a patient’s health care costs by preventing hospitals and physicians from charging exorbitant fees to buy and store specialty medicines themselves,” the study explained. “Secure, direct delivery is more efficient and effective and reduces health care costs.” Click here for the AHIP’s report (2-page PDF). Congrats to UGA postdoctoral researcher Smita Rawal, winner of a Best Poster Award at APhA’s Annual Meeting in Phoenix! She was among the UGA College of Pharmacy’s faculty and students presenting posters and serving as delegates to the Academy of Student Pharmacists at the meeting. W00t! Another team — this one out of Australia — says it’s cracked the problem of oral insulin. That problem: Proteins like insulin (and monoclonal antibodies) tend to get destroyed by the digestive system, hence the need to inject them The Aussies’ solution is pretty simple: “a special coating designed to not breakdown in the low pH environment of the stomach, before the higher pH levels in the small intestine trigger the capsule to dissolve.” But not to miss out on using nano in their work, the insulin itself is encased in “a fatty nanomaterial within the capsule.” Result: It works well for slow-acting insulin, but only so-so for the fast-acting stuff. Their next step is to try tweaking the capsule to release the dose on a particular schedule. Four of the FDA officials involved in the controversial approval of Biogen’s Alzheimer’s drug Aduhelm were being … well, we won’t say investigated, so how about looked into? They were being looked into for their overly close ties with the company. And, not being suspicious at all, all four have now left the agency — three to work for drugmakers. (The fourth’s landing spot isn’t yet known.) This isn’t to say they’ve done anything wrong, but … seriously guys. Why would people complain if the FDA wants to study how effective opioids are for chronic pain? Proponents of the study say it will prove that opioids don’t work well for the long term and thus shouldn’t be prescribed that way. But people opposed to the study say we already know that opioids do work long term so the study is “an awful lot of work for a very predictable answer” that will play into the hands of pharmaceutical companies. Did you follow that? One side is certain that opioids don’t work long-term (and wants the study to prove it), and the other is certain that they do work (and doesn’t want the study to prove it). And then, just to add to the mess, there are people who say that the study itself might get people addicted. Get your popcorn. Congress to NIH: Here’s $1 billion. That’s a thousand million dollars. Investigate long Covid and help develop treatments. NIH: (hums quietly to itself) Congress, later: So, whatcha got for us? NIH: Well, we did some “broader, observational research.” Congress: Got any patents? Started any patient studies? NIH: (rubs neck, looks embarrassed) Patients: [expletives deleted] First the idea of long Covid was just ignored or denied entirely. Now, says Ed Yong*, it “has morphed into a subtler dismissal.” Yet long COVID is a substantial and ongoing crisis—one that affects millions of people. However inconvenient that fact might be to the current “mission accomplished” rhetoric, the accumulated evidence, alongside the experience of long haulers, makes it clear that the coronavirus is still exacting a heavy societal toll. * He won the Pulitzer Prize for his coverage of the pandemic. The chain lost $241 million the past quarter — even on revenues of $6.1 billion. Non-Covid scripts are up, but Covid vaccines and testing are down, as is business for its Elixir PBM. A small study out of Washington University in St. Louis suggests that taking suvorexant (or other sleep aids — but suvorexant is what they used) can help break the cycle of ‘brain changes – sleeplessness – brain changes’ that Alzheimer’s patients can experience. No, it’s not a treatment, but it’s at least a bit of small arms in the arsenal if further studies pan out.Opioid-study protests, $1 billion for nothing, specialty pharmacy savings, and more
Insurers heart specialty pharmacy
Congrats to Smita (and UGA)!
(Another) potential insulin capsule
Gamers would call this “sus”
Should the FDA study opioids?
Money for nothin’
The Long Read: Long Covid Remains edition
Short Takes
Can Rite-Aid survive?
Sleep aid for Alzheimer’s
April 20, 2023 ✒ Andrew Kantor
Some facts to ponder, fellow taxpayers: About 11% of Medicare spending was on 27 drugs that — while new and expensive — had no evidence that they were better than existing treatments. Sure, they were FDA approved; they’re safe and effective. Just not more effective, according to a JAMA paper out of Harvard. 55% of the top-selling Medicare drugs in 2020 “had a low added therapeutic rating,” according to health technology assessments from Germany, Canada and France. A better use of the money, they suggest, would be creating an independent body that determined whether a drug was better or just more expensive. A simple screening test for Alzheimer’s may be on the horizon — one that uses blood rather than looking at brain proteins. Swedish researchers found that sugar molecules called glycans* in the blood are affected by the levels of tau proteins, which are a hallmark of Alzheimer’s. And glycans in the blood are a lot easier to measure than tau in the brain. “We also show that a simple statistical model that takes into account blood glycan and tau levels, the risk gene APOE4, and a memory test can be used to predict Alzheimer’s disease to a reliability of 80 per cent almost a decade before symptoms such as memory loss appear.” (Side note: In case you keep track of these things, we reported on a different type of early Alzheimer’s detection back in December 2022.) * Specifically one called bisected N-acetylglucosamine As the idea of amyloid plaques being the cause of Alzheimer’s comes under scrutiny, other therapeutic targets are emerging. One of the new ones: blocking an overactive enzyme (CDK5) that appears in the brains of people with Alzheimer’s. Using a peptide on mice that had the condition, MIT neuroscientists… … found dramatic reductions in neurodegeneration and DNA damage in the brain. These mice also showed improvements in their ability to perform tasks such as learning to navigate a water maze. Calling the peptide’s effect “remarkable,” the hope is that it’s opening a new pathway to treat dementia patients — at least those with overactive CDK5. A new device the size of a grain of rice can deliver drugs — nanoscale drugs, of course — directly to pancreatic tumors. The drugs are a monoclonal antibodies (“a promising immunotherapeutic agent” called CD40*) and because the device is implanted in the tumors, the doses are a quarter of what would normally be necessary. But wait, there’s more! If there are multiple tumors, the device also shrinks other tumors simply by activating the immune system, according to one of the nanomedicine researchers — this is a thing now — at Houston Methodist. * Not to be confused with WD-40, although who knows? WD-40 seems to do everything else. We’re not even halfway through the year, and already pharma companies are going nuts with the ads — so much so that the industry is now second in terms of ad spending behind “consumer packaged goods,” displacing technology companies. This isn’t just traditional “linear” TV ads; it includes commercials on streaming services, digital ads, billboards, and soon the ads that will be beamed directly into your brain when you walk past a pharmacy. Pro tip: Here at Buzz HQ, we don’t see ads on the Web (including social media!) thanks to uBlock Origin, a free, open-source ad blocker available for Chrome, Edge, Firefox, and Opera. (No, we weren’t paid to say that. We just hate ads.) In case you’re interested, here are the — well, the title says it: the top 20 pharmaceutical companies by revenue in 2022: Some preliminary experiments show that teriflunomide, which is used to treat patients with multiple sclerosis, might also be preventative — it could “stall the onset of symptoms in those with scans showing early signs of the disease.” The FDA has formally revoked authorization for the OG monovalent Covid-19 vaccines. The newer, bivalent vaccines from Pfizer and Moderna “are now cleared as a single-dose series for first-time recipients.”Easy Alzheimer’s test, pharma’s ad blitz, Medicare buys the pricier drugs, and more
‘No added benefit’
A new kind of Alzheimer’s screening
… and a new target for Alzheimer’s treatment
Delivering the drug to the tumor, micro-style
Pharma moves to #2 in ad spending
Saving you a click: top 20 pharma companies
Short Takes
MS treatment could be MS prevention
Good-bye, monovalent vaccines
April 19, 2023 ✒ Andrew Kantor
A pharmacy professor at UConn suggests that “Psychedelics may better treat depression and anxiety symptoms than prescription antidepressants for patients with advanced cancer”. The logic is simple (and he’s got some meta analysis to back it up): Psychedelics can often help treat people with PTSD, and a diagnosis of cancer or other life-threatening disease often leads to a form of that. We found that taking psychedelic medication alone – specifically LSD, psilocybin or MDMA – reduced depression scores as measured by the Beck’s Depression Inventory by six points, where a score below 10 indicates minimal to no depression. An important caveat: This isn’t a case of giving them these meds and sending them home. Treatment with psychedelics involves a combination of monitored drug use and psychotherapy. And, as always, “More research is needed.” Spring is here, spring is here — and now’s the time to take a good, hard look at your pharmacy and where you want it to go. Mollie Durham, PharmD, is here to help with a two-part virtual course giving you the tools you need (and the enthusiasm to use them!) to know where you are and where you want to be and then take smart, actionable, realistic steps to get there. Each part is just an hour long (and gives 1 hour of CPE credit), but it’ll pay years of dividends. Part 1: Where Am I, and Where Do I Want to Be? Wednesday, May 10; 7:00 – 8:00 pm via Zoom Part 2: How do I Get Where I’m Going? Wednesday, May 17; 7:00 – 8:00 pm via Zoom Each part is just $35 for GPhA members and $45 for non-members. The FDA has said that people 65 and older, or immunocompromised, will be allowed to get yet another Covid vaccine booster as soon as CDC Director Rochelle Wolensky signs off. (Only the Moderna and Pfizer/BioNTech bivalent vaccines are covered). People 65 and older should only get another shot if at least four months have elapsed since their most recent booster, according to the recommendation. For people who are immunocompromised, the suggested interval between shots is two months. Mammals, it seems, have a gene that’s expressed only in testicular tissue — the first one of the sort ever found. This is interesting for two reasons. First, if the gene is missing it leads to the most common form of male infertility. But more important for headlines, that means it’s also a target for “a highly effective, reversible and non-hormonal male contraceptive for humans and animals.” That’s because of what Washington State University molecular biologists found: When they knocked out the gene in mice, it created infertility only in the males, impacting their sperm count, movement and shape. [We assume they mean the sperm’s movement and shape, not the males’.] In theory — remember, testing has only started — “you could remove the drug and the sperm would start being built normally again.” The idea that Covid-19 could increase diabetes risk isn’t new; we wrote about it back in January. But now comes the first evidence — a whopping 1 in 20 new cases could be a result of Covid infection. That’s what Canadian researchers found when they examined the health records of 630,000 Canucks… …and found those who tested positive were significantly more likely to experience a new diagnosis of type 1 or type 2 diabetes in the following weeks and months — with 3-5% of new diabetes cases attributable to Covid overall. And in case your inner scientist is wondering: “Assuming the virus is directly to blame, the underlying mechanism also still needs to be teased out.” With the pandemic mostly behind us, the CDC has updated its immunization schedule (like it says in the headline) to account for missed vaccinations, the addition of Covid shots, and some small changes to existing vaccination recommendations. (There are a few other tweaks, like ones involving polio and dengue fever, that hopefully you won’t encounter.) New COVID-19 vaccines, new abbreviations for COVID-19 vaccine products, and revised text for vaccine injury compensation were included in the updates. The pneumococcal vaccine has also been added to the catch-up schedule… If you have a patient who keeps getting bouts of arthritis, here’s some advice you can pass on: Visit your dentist. Rockefeller University clinical investigators found that bad gums can lead almost directly to autoimmune flareups, like those of rheumatoid arthritis. [B]reaches in damaged gums allow bacteria in the mouth to seep into the bloodstream, activating an immune response that ultimately pivots to target the body’s own proteins and causes arthritis flare-ups. As one researcher put it, taking care of your teeth is kind of a no-brainer: “Gum disease is quite curable; rheumatoid arthritis can be much more difficult to treat.” The latest drug candidate to emerge from traditional Chinese medicine comes from a compound called indirubin, a natural dye that can be extracted from certain plants. It seems to improve the survival of mice with glioblastoma, and the Brown researchers working on it say they’re actually close to starting human trials. “That’s appealing because this type of cancer keeps finding ways around individual mechanisms of attack. So if we use multiple mechanisms of attack at once, perhaps that will be more successful.”The diabetes bump from Covid, gums and arthritis, LSD and PTSD, and more
Psychedelics and PTSD
Clean your business with Mollie Durham
Spring Covid boosters for some
Yet another (potential) male contraceptive!
Covid might be causing 5% of diabetes cases
CDC updates immunization schedule
Bad gums, bad arthritis
Short take
Purple cancer fighter?
April 18, 2023 ✒ Andrew Kantor
Merck’s Keytruda — aka pembrolizumab — can help treat high-risk stage III/IV melanoma, sure, but when you add an mRNA vaccination from Moderna it becomes a lot more effective. In fact… The findings, published Sunday, show that 44% of patients who received the combination therapy reduced the risk of recurrence compared to those who only received Keytruda. That’s accurate, but it’s not the number to get excited about. Get this: “[N]early 79% of the 107 patients who received the mRNA vaccine in combination with Keytruda were cancer free after 18 months.” Wow. Phase 3 trials will be starting soon, followed by trials on other types of cancer. Another reason to come to Amelia Island for the Georgia Pharmacy Convention: It might not be there in a few years. The island, that is: Study finds record-breaking rates of sea-level rise along the U.S. Southeast and Gulf coasts since 2010 So head over to GPhAConvention.com for the details and to register today! Stanford scientists have found a nifty way to attack skin cancer: genetically engineered bacteria. Specifically, it’s Staphylococcus epidermidis which (as you can tell by the epidermidis part) naturally lives on the skin. They souped-up the bacteria so it could produce an antigen — a copy of a protein unique to the problem tumor. Like mustering an army, the bacteria was able to “trick the mouse’s immune system into producing CD8 T cells targeting the chosen antigen.” These cells traveled throughout the mice and rapidly proliferated when they encountered a matching tumor, drastically slowing tumor growth or extinguishing the tumors altogether. In fact, the result even shocked the researchers: “The resulting immune response was strong enough to kill even an aggressive type of metastatic skin cancer, without causing inflammation.” Said one: “I honestly hadn’t expected it to work. Every other type of tumor vaccine research involves radiation, chemotherapy or surgery, but we barely did anything to these mice. The T cells did the work for us.” Why do some people respond better to immunotherapy for lung cancer? The answer could be millions of years old. Some people produce white blood cells (B cells, specifically) that attack the tumors, but not everyone. What’s the difference? Scientists at the Francis Crick Institute found the surprise answer: In some cases, the cancer was ‘waking up’ dormant genes — viral DNA that was thousands or millions of years old. And those genes attracted the B cells. [T]he antibodies recognised proteins expressed by ancient viral DNA, known as endogenous retroviruses (ERVs), which form about 5% of the human genome and are passed down from the historic infections of our ancestors. In the majority of healthy tissue these viral genes are silenced, but in cancers they can be woken up. This means they may have found a way, either by using or mimicking that old DNA, to turn up the response of the body’s B cells and get them to attack tumors. What do you do when vancomycin can’t kill bacteria? How about giving the drug the ability to shape-shift — to change its atomic structure so that if one version doesn’t work, another might? And as a bonus, bacteria would have a tough time developing resistance; it’d be like trying to defend against Jackie Chan while he’s got a Swiss Army Knife*. The trick (found scientists at Cold Spring National Laboratory) is to combine vancomycin with a molecule called bullvalene. Bullvalene has an interesting property: Its atoms can swap positions, Rubik’s Cube-style. Using a technique called click chemistry, scientists at Cold Spring National Laboratory clicked the vancomycin with the bullvalene to create a “shape-shifting antibiotic significantly more effective than vancomycin.” And it worked. On moth larvae, anyway, where it cleared an infection without the bacteria becoming resistant. Next up … you guessed it. More research. * Not the best analogy, we admit, but you get the idea. UPC bar codes are out, and “2D barcodes” are in — well, they will be over the next few years, with a full phase out by 2027. (That sounds a long way away, doesn’t it? But it’s not even four years.) The difference? QR codes will be able to link to a lot more information for both businesses and consumers — distributor tracing, manufacturing data, dosage information, side effects … you get the idea. Will you need to update your barcode scanners? Why yes, you probably will. Side note: Want to create your own QR codes that link to your website, Facebook page, YouTube channel or more — or that simply contain your contact info? Here at Buzz HQ we use the free QRCode Monkey. No, we weren’t paid to say that. “Poverty could be a major risk factor for death in the U.S.” The FDA has updates its label requirements for opioids, requiring packages to have warnings about overdose risk and opioid-induced hyperalgesia, as well as mandating changes to the boxed warning and the “Indications and Usage section.” You can see a handy-dandy chart here (PDF). The end of bar codes, Rubik’s antibiotic, double-teaming melanoma, and more
mRNA vax + pembro = skin cancer killer
Get to the convention while you can
Bacteria train the body to attack melanoma
Ancestor’s virus, today’s cancer-fighter
Shape-shifting antibiotic
Coming soon: QR codes for everything

Captain Obvious thinks Norway may be on to something
Short Take
New opioid label requirements
April 15, 2023 ✒ Andrew Kantor
The power to administer Covid-19 and flu vaccines, that is. The Biden administration officially ended the pandemic emergency, but HHS will keep some of its powers — notably the rules (plural, because there isn’t really one emergency rule) “that let pharmacists, pharmacy technicians, and pharmacy interns give Covid-19 vaccines and tests and seasonal flu vaccines will stay in place through December 2024.” The estrogen in contraceptives could be cut by — get this — 92% and still be effective. Well, maybe. That’s what the computer model suggests, anyway. Keep that last part in mind when you see the headlines. This wasn’t tested in the real world, just “an existing mathematical model of the menstrual cycle” plus data from 23 women. It also “assumes that the estrogen coming from birth control stays at a consistent value and doesn’t incorporate how the body absorbs the hormone over time” and relies on the hormones being delivered “during a critical window of the menstrual cycle.” Interesting? Yes. About to change how birth control is delivered? Nuh-uh. May 21 is your last chance for a while to take the Big Kahuna of immunization certificate courses: APhA’s Pharmacy-Based Immunization Delivery Certificate Training Program. It’s a total of 23 hours of CE, and it’s the nationwide immunization training you want. The live portion (8 hours) is being held at GPhA’s North American headquarters in Sandy Springs from 8:00am to 5:00pm on Sunday, May 21. Space is limited and time is running out. Click here for the details and register today! (After you take the live portion, the rest is self study — easy peasy. At the end you get the certificate for your wall and that important line on your CV!) Remain immobile long enough, on a long flight or while bedridden for instant, and you run the risk of dangerous blood clots — venous thromboembolism. Yet bears hibernate all winter without issue*. What’s up with that? German cardiologists decided to find out, and find out they did. It’s all about a protein called HSP47 that helps make platelets sticky, and that pretty much disappears from the blood of hibernating bears. (And there’s evidence that lower HSP47 levels in humans reduces clotting risk.) The finding raises hope that researchers can develop drugs that block HSP47, giving doctors a new tool to treat or even prevent clots in immobile patients. * Unless they sense a nearby pic-a-nic basket Rather than relying on standard doses of analgesics, it’s better to monitor absorption and tweak the dose to match the patient. And that’s why Brazilian researchers… … have developed a simple, cheap and flexible sensor that rapidly analyzes saliva to detect paracetamol [acetaminophen], a widely used analgesic, and monitors its action in real time to permit dosage correction. Not that it’ll be available any time soon: They’ve made a prototype and now want to find “a future partner company interested in mass-producing and marketing the device.” People with protoporphyria — where, when exposed to sunlight, protoporphyrin in the blood vessels “triggers inflammation, cell damage, and severe pain” — now may have a simple, oral treatment (as opposed to an implant that needs to be replaced). Called dersimelagon, it increases the skin’s pigmentation, letting vampi— er, protoporphyriacs spend more time in the sun. The drug did have side effects — most often nausea, freckles and headaches. The nausea and headaches were short-lived and “well-tolerated,” Desnick [one of the researchers] said. (Some people did not like the freckles, though, he noted.) Larger-scale human trials are underway in northwestern Romania. * “They call themselves shadow-jumpers, because they have to run from one shady spot to another to avoid the sun.” Why do some people get urinary tract infections over and over? And why does getting one increase the risk of getting a second? Microbiologists at Washington University in St. Louis think they’ve finally cracked the case. It’s epigenetics, aka ‘Lamarck was right.’ The paper suggests that UTIs can actually change the DNA in the cells lining the urinary tract. Those cells can then change size and start an immune response that actually makes them more susceptible to repeated infections. [Technically it’s changing the way the DNA is being read, not the DNA itself. Sorry, Lamarck.] The good news: Assuming the WU folks are right, now we know why some folks are reinfected. The bad news: There’s not a lot to be done about it … yet. (Also, the tests were done on mice, not humans.) Bats carry human diseases but don’t get sick. They rarely get cancer. They can live to the human equivalent of 200 years. So they’re an obvious animal to learn from. [T]o researchers and biotech investors, they are a miracle mammal that could help prevent pandemics and reveal blockbuster treatments for deadly human diseases or to slow aging.Vampire treatment, learning from da bears, pharmacists keep vax power, and more
Post-emergency, pharmacists still have the power
Hormone headlines vs. reality
Do NOT wait to get your APhA vaccination certificate!
Why sleeping bears lie (safely)
A tongue-based med monitor
Good news for vampires (really)
Why UTIs repeat
The Long Read: Learning from bats
April 14, 2023 ✒ Andrew Kantor
If a hypertension drug isn’t working for a patient, the solution isn’t to increase the dose, but to switch meds. Swedish researchers studied 280 patients on 4 drugs over a year. What they found is that — for reasons they haven’t teased out yet — there are optimal meds for each person. Taking more of an ineffective drug it seems, is just as ineffective. “The effect of a change of medication can be twice as great as the effect of doubling the dose of the patient’s current medication.” For once, “game-changer” applies: A new test for Parkinson’s disease can accurately diagnose early signs of the disease long before symptoms appear, and with 90% accuracy. Although screening people isn’t around the corner, it is just down the street. Not only will this enable patients to get a jump start on treatment, by confirming a sign of the disease — the presence of a misfolded protein called alpha-synuclein — it can pave the way for treatments … or at least show which way the road has to go. The Parkinson’s test is a direct result of the work and funding of the Michael J. Fox Foundation — here’s the story. Diabetics might want to avoid NSAIDs. Taking them even for a month “sharply raises the risk of an [heart failure] hospitalization” according to a new study out of Copenhagen University. That doesn’t mean every diabetic is in danger, according to those shifty Danes, but certain subgroups should probably be monitored more closely… … including the very elderly, patients with uncontrolled diabetes, those prescribed an NSAID for the first time, and patients already taking both a renin-angiotensin-system inhibitor (RASi) and a diuretic. What’s the deal? Part may be temporary fluid overload from the NSAIDs’ effects on the kidneys, and part may be “direct effects on the heart by any of several proposed mechanisms.” Or, you know, both. Here at Buzz we like to point out when a new treatment appears that treats mice or rats. Sure, the implication is that humans will get it next, but that’s not always the case. One reason: Most rodents can’t vomit, and “Over the years, millions of dollars have been lost on treatments that failed after vomiting cropped up as a side effect.” There’s no treatment for fatty liver disease in humans, but now there appears to be one for other primates — that’s good news could be on the way for we hairless apes. It’s called DT-109 (not to be confused with JFK’s PT-109) and it comes out of the University of Michigan where medical researchers found that “DT-109 reversed fat buildup and prevented scarring in the livers of both mice and primates that had developed NASH [nonalcoholic steatohepatitis, the later, worse stage of fatty liver disease].” If it pans out, DT-109 could make a big difference, what with fatty liver disease often leading to chronic liver disease and eventually the need for a transplant. On the one hand, being double-jointed might let you run away with the circus or become part of a bank-heist gang. On the other hand, its extreme form — hypermobile Ehlers-Danlos syndrome (EDS) — can mean fragile connective tissue and a host of health issues. Breakthrough: Both might be caused by a folate deficiency caused by a particular gene, according to Tulane University neuroscientists. Those with this genetic variant can’t metabolize folate, which causes unmetabolized folate to accumulate in the bloodstream. The folate deficiency may prevent key proteins from binding collagen to the extracellular matrix. This results in more elastic connective tissue, hypermobility, and a potential cascade of associated conditions. The treatment is simple: Methylated folate, which is already processed and available over the counter. Listening to music — with vocals — may make your child better able to understand speech (and thus more likely to get into a fancy private school and ivy league university). Scream. It might make the experience less painful. Just be sure to use the University of Michigan-designed Fitzmaurice vocal technique.When mouse models fail, NSAID dangers for diabetics, double-jointed treatment, and more
The Monty Hall problem, BP meds-style
A major Parkinson’s breakthrough
Side note (and today’s Long Read)
Diabetics’ NSAID danger
Of mice and men
Fatty liver disease gets a (potential) drug
Flexibility and folate
Short Takes: The sound and the fury
Before your baby’s born
While you’re giving birth
April 13, 2023 ✒ Andrew Kantor
Hangover “cures” are as common as hiccup cures, and they’re at best hit or miss. Now Chinese scientists think they’ve got one that actually works thanks to, you know, science. The idea is simple: “An enzyme called ADH1B accelerates the breakdown of alcohol in the body. Researchers genetically engineered a probiotic to express ADH1B in mice.” When they gave the mice the probiotic, it reduced the amount of alcohol they absorbed and let them recover sooner. Picture this: Untreated mice showed signs of drunkenness 20 minutes after exposure to alcohol. When the mice were placed on their backs, for example, they were unable to get back on their feet. But in the group that received a probiotic that expressed human ADH1B, half the mice were still able to turn themselves over 1 hour after alcohol exposure. A quarter never lost their ability to turn themselves over. Fun fact: That ADH1B enzyme is common in East Asian and Polynesian populations, which is why you never get into a drinking contest with a Samoan. Check it out: GPhA’s marketing and communications manager, Lucy “Yes, I play the ukulele” Haney, was profiled in VoyageATL, where she talked about her role with GPhA, and how her creative background has helped her career in healthcare communications. Working at GPhA allows me to support the growth and development of the pharmacy profession in Georgia, as well as to contribute to Georgian’s overall access to healthcare (after all, pharmacists are the most accessible healthcare professionals)! If you’ve spawned a mean kid (we won’t say mean girl because we all know they come in both flavors), you might want to consider vitamins. Really. A Canadian review study (in the journal Aggression and Violent Behavior) — found that in between “psychosocial interventions” and prescription meds are supplements to help the nervous system develop properly — before Junior can recite the Miranda warning from memory. Well, maybe. The results of 22 studies that covered macro- and micro-nutrients were mixed, although 14 of them found vitamins and other supplements (e.g,. omega-3 fatty acids) had beneficial effects on aggression. A full 19 studies found they could help depression and even symptoms of ADHD. The conclusion: A single supplement may not help, but “wide-range vitamin and mineral supplements may have beneficial effects in reducing excessive hetero-aggression in children and adolescents.” The US continues to lag the rest of the developed world in life expectancy — Americans average 3 to 5 years less — and it’s getting worse. One reason, says FDA commish Robert Califf, is the spread of misinformation (what we used to call lies). Our medical system is almost as good as that of Western Europe, for example, but we simply don’t use it as well because too many people believe what they see on social media. “Why aren’t we using medical products as effectively and efficiently as our peer countries? A lot of it has to do with choices that people make because of the things that influenced their thinking,” Califf said. These days half of new treatments seem to involve either mRNA or nanotechnology. Now UCLA immunologists are using both, and they think they’ve got essentially a peanut allergy vaccine. It delivers an mRNA payload to the liver, where they “teach the body’s natural defenses to tolerate peanut proteins.” It works similarly to how mRNA vaccinations prevent Covid-19, but instead of encoding for the SARS-CoV-2 spike protein, it encodes for a peanut protein — one that doesn’t trigger an allergic reaction, but that primes the body to deal with the peanut proteins that do present a problem. How about a vaccine against food poisoning? Specifically, against norovirus? How ’bout if we throw in protection from rotavirus, too? That’s what Washington University in St. Louis molecular microbiologists think they’ve accomplished. They piggybacked a norovirus protein onto an existing rotavirus vaccine and presto: “Mice that received the experimental vaccine produced neutralizing antibodies against both rotavirus and norovirus.” So far it’s just in vitro and in mouse-o, but obviously more experiments are underway. Antibiotic resistance has a cousin: antibiotic tolerance, where bacteria aren’t killed by a drug, but instead slip into a dormant state, waiting for the danger to pass. A microbiologist explains. China reported the first human death from the H3N8 bird flu. It had been found in humans for the first time last year. Food manufacturers found it’s less expensive to add sesame to food — and add a warning label — than to sterilize the equipment so they can call it “sesame-free” as a new law requires. The result? Foods that sesame-allergic kids and adults have eaten safely for years are now potentially life-threatening. Sexually transmitted diseases hit a record high in the US in 2021 according to the latest CDC data — up 5.8% from 2020, in fact. Some STIs such as syphilis saw their highest numbers in more than 70 years. The 176,713 syphilis cases recorded in 2021 were the highest since 217,558 in 1950. Preventing mean kids, potential hangover cure, sesame shenanigans, and more
Probiotic of the dog
Shout-out to GPhA’s Lucy

Mean kids need their vitamins
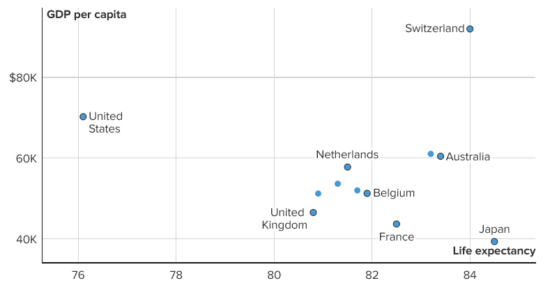
Don’t believe the lies (and live longer)
Peanut allergy vaccine in the works
Soon you’ll be able to schedule that Royal Caribbean cruise
The Long Read: When bacteria play possum
Short Takes
Well that’s not good
Elmo needs his Epi-Pen
ICYMI: STIs on the rise
April 12, 2023 ✒ Andrew Kantor
Stored at room temperature, insulin may have a shelf life up to four times longer than what’s on the package — that’s according to a new international study led out of Sweden’s University of Gothenburg. How’d they test? Let’s just say they didn’t use any fancy temperature controls: Six different families in Nagpur, India, stored the insulin for a period ranging from one to four months in the summer. It was stored either in a box in the coolest room in the home or in clay pots designed to serve as simple cooling systems, with evaporation of water keeping the contents cool. Larger studies are needed, they say, but “The period when insulin may still be used can potentially […] be extended to three or perhaps even four months.” Don’t wait to treat high blood pressure. A new study out of UC Davis found that having hypertension in your 30s could mean that, 40 years down the line, your brain isn’t working properly. The researchers found that the high blood pressure group had significantly lower regional brain volumes and worse white matter integrity. Both factors are associated with dementia. The research also showed that the negative brain changes in some regions — such as decreased grey matter volume and frontal cortex volume — were stronger in men. With treatment for dementia so limited, the researchers point out, it’s critical to find ways to reduce the risk as early as possible. New stage 3 trials confirm Pfizer’s earlier results: The company’s RSV vaccine “was found to be 82 percent effective in preventing severe cases of RSV in infants when it was given to pregnant mothers in the second half of their pregnancy.” One downside is that it only prevented severe cases, but didn’t do well to prevent non-severe infections. The University of Rochester would like you to know that there are three other RSV vaccines in the works (and it’s been involved in the testing of Pfizer’s vax and two of the others, including a candidate from GlaxoSmithKline). There was a lot of hubbub regarding the regulation of mint-flavored e-cigarettes, mostly because they were disproportionately marketed to and used by kids and the Black community. But a new study out of the University of Pittsburgh finds that … … e-cigarette liquids containing menthol generated a larger number of toxic microparticles in the lungs compared to menthol-free juice. And when they looked at patients themselves, they confirmed that yep, there was a “difference in lung function between menthol e-cigarettes and non-menthol smokers.” CMS has finalized a rule for Medicare Advantage providers designed to keep those insurance companies in line. First of all it sets marketing rules (e.g., prohibiting confusing words and imagery) and second, it improves the prior-authorization process. [It] requires prior authorization approvals to be valid as long as medically necessary and states that coverage denials based on medical necessity must be reviewed by healthcare professionals with relevant expertise before issuing a denial. It will also make it easier for patients to switch MA plans, and “implements provisions of the Inflation Reduction Act to improve access to affordable prescription drug coverage” by expanding eligibility to individuals with incomes up to 150 percent of the federal poverty level. It’s infecting condors in Arizona and — notably — more pet cats. Food processing giant Archer Daniels Midland is working with a biotech startup called Brightseed to develop biological products designed to improve that ol’ gut microbiome. As they put it “natural and plant-based solutions that target immune function, metabolic health and mental well-being.” The companies are expecting to launch their synbiotics as functional ingredients in foods, beverages, dietary supplements and medical foods, by 2025. A new vaccine for Lyme disease is still coming down the pike — this one’s from Moderna. Treat hypertension sooner, discard insulin later, give up the menthol vapes, and more
Insulin lasts longer than you think
High BP now, smaller brain later
RSV vaxes gets closer still
Side note: There’s more
Minty not-so-goodness
New Medicare Advantage rules in place
Short Takes
Bird Flu Watch
Gut health goes even more mainstream
Another Lyme vax is in the works




