August 18, 2022 ✒ Andrew Kantor
There’s one treatment for the flu: Tamiflu. The rest is treating symptoms and making patients comfortable until it passes. But now Canadian infectious disease experts have found what they think “could be part of a one-two punch” to treat it … in mice, at least. That second punch: antibody therapy. Yeah, the same stuff used to treat Covid-19. When combined with antivirals like Tamiflu, “the drugs improved the virus-fighting properties of the antibodies” and helped trigger the immune system to kill the virus before it can spread. Their hope, of course, is that this works on humans — especially high-risk groups during next flu epidemic. Switching to e-cigarettes doesn’t seem to increase nicotine dependence. That doesn’t mean vaping is better in terms of addiction, just that it isn’t worse. (And there’s the advantage of skipping the whole “tar and smoke” thing … although e-cigs have their own set of nasty chemicals.) Penn State researchers found that, just because vaping makes it easier (and a bit more socially acceptable) to get a nicotine fix, it doesn’t mean there’s a greater chance of addiction. CVS, Walgreens, and Walmart were ordered to pay $650.6 million to just two Ohio counties after a jury decided “that the companies helped create a public nuisance in Lake and Trumbull counties by over-supplying addictive pain pills.” Of note: This is the first time that pharmacy chains have had to pay for their role in the crisis. The pharmacies, of course, argued that they can’t be held liable for filling legal prescriptions; they plan to appeal. Endo Pharmaceuticals, which is (was) $8 billion in debt while facing thousands of lawsuits for its role in the opioid crisis, is the latest opioid manufacturer to file for Chapter 11 bankruptcy, following in the footsteps of Purdue Pharma and Mallinckrodt. What does the Inflation Reduction Act mean for pharmacy? Glad you asked. NCPA has the answers in a two-page PDF. People are getting to sleep and using fewer prescription meds to do it. That’s what University of Florida health scientists found looking at data from 29,400 people from 2013 to 2018. It wasn’t a small decline, either — overall, they found a 31% overall decline in the use of common sleep medications — “a trend thought to be linked to a greater awareness of the potential pitfalls posed by these prescriptions.” But for those over 80, it was even bigger: an 86% decrease. Big ol’ caveats: First, it only looked at prescription sleep meds, not OTC drugs like melatonin. Second, the data are only through 2018, and there have been some changes in the world since then that might keep people up at night. Despite the temptation (and the official submission), the WHO will not be renaming monkeypox to “Poxy McPoxface.” Nor will it choose “TRUMP-22*,” although “Mpox” is in the running as the agency continues to consider a new name in the hopes that the public will stop calling monkeypox, monkeypox. “It’s very important we find a new name for monkeypox because this is best practice not to create any offence to an ethical group, a region, a country, an animal etc,” said a spokesperson, implying that “chickenpox” and “swine flu” will also receive new names. “Patients Have Higher Health Care Use After Covid-19 Infection” Should you worry about Centaurus, a subvariant of Omicron? Who knows? Not the experts. Centaurus, aka Omicron BA.2.75, is spreading in India and at least 20 other countries, but it’s not clear whether it will be worse than the current BA.5. In fact, getting infected by BA.5 might reduce the risk of Centaurus (and getting boosted this fall should also protect against it). And if you’re wondering why a sub-variant gets to have a name, it’s because some guy on Twitter called it that … and it stuck. Georgia used to have among the highest number of high school football player deaths in the country. That’s changed in the last decade, and now Georgia’s new regulations “have become a model for other states looking to protect student athletes from the heat.”Rejected monkeypox names, variant name is coined, costly pharmacy loss, and more
Two meds, one flu treatment
A good bit of vaping news
Opioid fallout
Pharmacies lose big in Ohio
Endo goes bankrupt
Yes, but what about me?
Sleep without drugs
Namey McNamechoice
* “Toxic Rash of Unrecognized Mysterious Provenance of 2022” (really)
Captain Obvious treats himself
The next Covid variant
Non-pharma, good Georgia health news story of the week
August 17, 2022 ✒ Andrew Kantor
It’s been years (and years), but the FDA has finally approved a new category of over-the-counter hearing aids for people with mild to moderate hearing loss. Essentially they’re the audio version of non-prescription reading glasses. These are not to be confused with non-prescription hearing aids that are already available — those are technically “personal sound amplification products” … although to be fair it’s hard to figure out where the line is. A simple way to help reduce blood pressure: Use a different kind of salt — potassium chloride instead of sodium chloride (e.g., Morton’s Salt Substitute, NuSalt (“Vegan”!), or MySalt). A review by an international team of researchers confirmed that yes, everyone can lower their blood pressure by switching off sodium chloride. Or, if you want to sound smarter, “The beneficial effects of salt substitutes* on blood pressure across geographies and populations were consistent.” (Back in April we reported how switching to KCl could cut the risk of strokes. This new study expands that to general health.) Putting a Band-Aid (or other brand of adhesive bandage) on wet skin is … well, pointless. It just slides off. But Canadian engineers have found a way to force them to stick: ultrasound. It seems the right frequency makes microbubbles in the adhesive, causing to to adhere to skin like a clingy five-year-old in Ikea. Takeaway: Next time you spend a day at the beach, be sure to pack an ultrasound transducer in your first aid kit. (Bonus: The technology may not be game-changing, but they do call it “paradigm-shifting.”) Do you sell CBD products for pets? Maybe you should. Not that they necessarily do much, but because a new report expects “CBD pet products to see double-digit growth” through 2027. As pet and animal products are focused on treats, supplements and food additives, therapeutic CBD with antianxiety and anti-inflammation properties is expected to remain the top-selling product. Want the full report? You can get it here for just $4,750. Researchers at the University of Alabama and Syracuse University, after conducting a two-year trial, have figured out that sending parents personalized text messages (rather than mass communications like TV commercials) works better at reminding them to get their kids a second flu shot. The startling conclusion: [I]f the recipient does not delete the message, [it] allows for them to come back to the information later at their time and convenience. What does it cost to get eye docs to prescribe your brand-name drops over a generic? How about $65 a year? So say Johns Hopkins researchers who checked out the prescription and payment data. [T]he researchers concluded that practitioners receiving any amount of pharmaceutical company payment were 1.8 times more likely than practitioners receiving no payments to prescribe branded eyedrops more than half of the time. And, they say, this applies across the board — it’s not skewed by a few big subscribers, nor is it affected by location, age, or gender. The headline kinda says it all: “Dog catches monkeypox from owners after sleeping in their bed.” The WHO is planning to rename monkeypox to “avoid causing offense to any cultural, social, national, regional, professional, or ethnic groups.” They can’t specify who might find it offensive, because naming a particular group would imply a connection to monkeys … and that would be offensive*. If you have an idea for a name, you can create an account and submit it here. Think you don’t have to worry about monkeypox? A new CDC report found that “Monkeypox can persist in household environments” with viable virus samples persisting15 days after an infected person had left the home, especially on porous surfaces. (It’s not entirely surprising, they say; variola can remain viable for years in a cool, dry, dark environment.) Health-related apps and websites — including those of hospitals — collect loads of personal info. Some of them, it seems use that information in ways that violate their promises … or even the law. You might assume they share that data with some shady, bottom-feeding company that will use it for no good. And you’d be right; they’re sharing it with Facebook by using ad trackers that “followed the patients online and marketed to them based on those activities.” And it’s not just smaller healthcare companies. Hospitals are doing it too by embedding a Facebook tracker in their websites. Clicking the “Schedule Online Now” button for a doctor on the website of Froedtert Hospital, in Wisconsin, prompted the Meta Pixel to send Facebook the text of the button, the doctor’s name, and the condition we selected from a dropdown menu: “Alzheimer’s.” Here at Buzz HQ, we use the Privacy Badger addon for our Web browsers, which keeps most of those trackers at bay, and uBlock Origin to avoid seeing those pesky ads at all. They’re both free. Dogs with monkeypox, eye docs getting paid, who uses your health data, and more
Here come (more) OTC hearing aids
Easy BP control
* Here at Buzz, we don’t like the term “salt substitute.” It’s just a different *kind* of salt. Chicken is not a “meat substitute.”
Making the bandage stick
Their dogs want CBD
Captain Obvious prefers a letter
Cheap and easy
Monkeypox updates
Fido gets the floor

Name games
* Meanwhile, Legionnaires’ disease is still Legionnaire’s disease.
Here, have something to worry about
Sneaky info sharing
August 16, 2022 ✒ Andrew Kantor
A US Court of Appeals has ruled that Pfizer’s co-pay assistance program for its Vyndaqel and Vyndamax meds (tafamidis, if you’re being formal) violates the Federal Anti-Kickback Statute. The logic is that Pfizer is essentially saying to patients, “If you get this med (and we get $212,000 from the government), we’ll give you $13,000.” (Officially, Pfizer is offering to cover Medicare patients’ $13,000 co-pay.) Pfizer argued that, because tafamidis is the only med for a rare heart condition, co-pay assistance didn’t “improperly induce the underlying prescribing decisions.” In other words, it’s not as if patients were able to choose tafamidis over something else. The Office of the Inspector General disagreed, saying it didn’t matter whether Pfizer’s intent was good or evil — the goal of the co-pay program was to pay people to get the government to buy Pfizer’s meds. The court agreed with the OIG, and here we are. How will this affect other co-pay programs? Stay tuned. This is what you need to know: Americans, please form an orderly queue when going to Montreal to get a monkeypox vaccine. Know someone with kidney stones? You might recognize them by the pale complexion or the screaming in agony. You can taunt them by saying, “You know, having enough “calcium, potassium, caffeine, phytate, and fluid[s]” could have prevented that, according to researchers at the Mayo Clinic.” But if you feel like being nice, you can let them know that those same researchers narrowed down the details. It seems that you can prevent recurrence of kidney stones by making sure you have enough calcium and potassium in your diet. (Or as they put it, “Lower dietary calcium and lower potassium intake were predictive of symptomatic kidney stone recurrence.”) Shout-out to Shane Pruitt, GPhA member and director of recruiting and undergraduate advising at UGA’s College of Pharmacy, who was just featured in UGA Today. I didn’t think this could be done, but I’m not a Cambridge University researcher. They were able to change the blood types of three donor kidneys from type B to type O, the universal donor. How? They added an enzyme to blood that they pumped through the organs; it “removed the blood type markers that line the blood vessels of the kidney, which led to the organ being converted to type O.” As you might imagine, this is big news — especially for people with type B blood, because it’s uncommon enough to make finding donors much harder. It’ll be ready this month. The bivalent booster, called mRNA-1273.214, is designed to protect against the OG Covid virus as well as Omicron — including the BA.4 and BA.5 subvariants that are the current 800-lb. (57 stone) gorillas. And that’s why… The UK has approved it. The Medicines and Healthcare products Regulatory Agency (FDA with a British accent) is the first of the big approvals Moderna expects; it’s also submitted it to Australia, Canada, the EU, and the US. There’s a proven way to treat depression: deep brain stimulation of the prefrontal cortex. Problem: You need to drill holes into the patient’s skull to implant electrodes. Various ways to avoid the whole putting-holes-into-someone’s-head thing have been tried, with varying degrees of success. The latest comes from Hong Kong, where biomedical and electrical engineers have come up with a way to stimulate the prefrontal cortex without drilling holes, but maintaining almost the same level of disturbance. They go in via the eye. The call it “non-invasive stimulation of the corneal surface” or transcorneal electrical stimulation (TES). They tested it on animals and it… … resulted in remarkable antidepressant-like effects and reduced stress hormones in an animal model for depression. Furthermore, this technique induced the expression of genes involved in the development and growth of brain cells in the hippocampus. That does not look comfortable. Pro tip: If you find that someone in your pharmacy was in contact with a Covid-19 patient, don’t lock down your building and try to quarantine everyone. News of the flash shutdown sent shoppers fleeing and screaming in an effort to get out of the building before the doors were locked, videos on social media showed. According to pharma companies, capitalism is a one-way street, and it leads to their CEOs’ paychecks. Read how “Big Pharma Went All In to Kill Drug Pricing Negotiations” — and how it’s used the same (wrong) argument for a long long time. The drug industry warns that any price negotiation will kill innovation. Such warnings “constitute the pharma response in literally every instance since 1906,” the year the first drug regulation agency was created. Fun fact: The Affordable Care Act was also supposed to “kill innovation,” and yet pharma companies are reaping record profits. Go figure. Changing an organ’s blood type, calcium stops stones, treating depression through the eye, and more
Court nixes copay assistance
Immunization training: less than a week to go
The French-Canadian connection
People with good calcium shouldn’t get stones
Shaaaaaaaaaaane

Kidneys get their ‘O’ face
A bit about Moderna’s booster
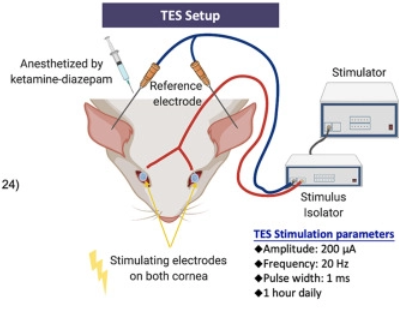
Here’s electrodes in your eye
Business 101
The Long Read: Same Old Song edition
August 13, 2022 ✒ Andrew Kantor
Imagine spending millions on TV ads that annoy the heck out of people, only to find that no one remembers your name? Welcome to the world of diabetes-drug marketing. A new survey found that despite huge spending by companies like Eli Lilly and Novo Nordisk, “patients struggle to remember the drugs’ names.” Jardiance? (shrug) How about … metformin? Yep, that one they know. Fundamentally, said one researcher, “they won’t care whether they are on, say, Jardiance or AstraZeneca’s Farxiga, because those names have little meaning for them.” Amusingly, a new paper just came out of Johns Hopkins claiming that direct-to-consumer ads actually work. Or as they put it: Brief exposure to prescription drug advertisements has a large and positive association with medication-related demand intentions. Baloxavir Marboxil — it’s not just the winning play in the 2019 Lithuanian Scrabble Championship. It’s also the latest drug approved by the FDA for treating kids (5 to 11.99 years old) who have the flu. In fact, it’s the “first single-dose oral medication approved for treating flu in children of this age group.” Just be sure they’ve had symptoms for fewer than 48 hours. Who needs drugs to treat pain when you have sound? And electricity? Not guinea pigs, that’s who. Using a combination of pulses of “broadband sound” (tones ranging from 625 Hz and 40 kHz) and a bit of electrical stimulation, University of Minnesota researchers … … found that the combination of the two activated neurons in the brain’s somatosensory cortex, which is responsible for touch and pain sensations throughout the body. They used needles to send the current, but they say it could be done non-invasively with one of those TENS* units you might even sell in your pharmacy. “Johnson & Johnson plans to halt talc sales worldwide”. The PR person says: “Vitamin D supplementation seems to alleviate depressive symptoms in adults”. The gist is: A meta-analysis out of Finland found “that vitamin D supplementation may alleviate depressive symptoms in adults with depression.” But the study’s lead author says: “[T]he certainty of evidence remains low.” Yet, he adds, it’s worth doing a proper study: “These findings will encourage new, high-level clinical trials in patients with depression in order to shed more light on the possible role of vitamin D supplementation in the treatment of depression.” The Covid-19 pandemic isn’t over. The latest CDC data shows cases dropping … but still 100,000 Americans are testing positive per day, including 20 Georgians. And that’s just the ones we know about. There are more than 40,000 Americans currently hospitalized with Covid (1,800 in Georgia), and 300 to 400 die every day. (That’s lower than the peak, but higher than this time last year.) More than a million* Americans have died since the pandemic began — including almost 38,000 Georgians. If you think you’ve been exposed to Covid-19 and you have symptoms, one negative result from a home test isn’t enough, says the FDA. No, two isn’t enough either. The number of the counting shall be three negative tests 48 hours apart to be sure you’re not exposing others. (If you’re symptom-free but have been hanging out with someone who’s sick, then two should be enough.) This only applies to the rapid-antigen home tests (available free via the gummit at Covid.gov/tests), not the super-accurate PCR tests that are sent to a lab. https://www.youtube.com/watch?v=bEcjFRB-1C4 Biomedical engineers in California have created a prototype contact lens that can detect cancers. They can capture exosomes in a wearer’s tears and analyze them for cancers. The lenses are made with thousands of microchambers containing gold nanoparticles that [insert science magic here] and can thus detect antibodies associated with cancer. (Essentially it’s just a simple way to analyze tears, which the team — from the Terasaki Institute for Biomedical Innovation — say are a better source of exosomes than blood, urine, or saliva.) There’s no cure for tinnitus, but there may be an app for treatment. Kiwi researchers have created a “digital polytherapeutic” — aka, an app, bone conduction headphones, neck pillow speaker, and an audiologist to help personalize that app. The app plays various sounds to mask the tinnitus, relax the patient, and retrain the ear, asking for feedback along the way (e.g., “Which ear do you hear the shaver in?”) to adjust the therapy. “What this therapy does is essentially rewire the brain in a way that de-emphasises the sound of the tinnitus to a background noise that has no meaning or relevance to the listener.”Electric pain treatment, why you need three Covid tests, no one knows diabetes meds, and more
Full of sound and fury, signifying nothing
Trulicity? (shrug)
Januvia? (shrug)New kids’ flu med
Sound and electricity vs pain
* Transcutaneous electrical nerve stimulation, in case you’re unfamiliar
I didn’t know they were still selling it
Can D help depression?
Lest we forget
* A bare minimum of 1,030,777, but certainly more.
Three is a magic number
Look into my eyes (for cancer)
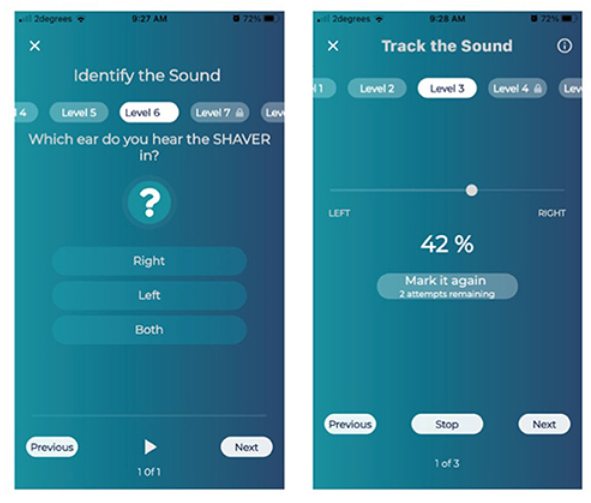
Tinnitus-fighting app
August 12, 2022 ✒ Andrew Kantor
A new virus — Langya henipavirus (LayV) — has infected dozens of people in China. (“Dozens” = 35.) The question: Is this a legitimate concern, or are we on viral hair-triggers because of, you know, other viruses? The answer, per the GPhA Buzz Crystal Ball™, is … it’s probably nothing to worry about unless you’re a cable news producer looking to fill time. Do you want to worry? Fine, here: “[Other] henipaviruses, like Nipah and Hendra, are known to cause severe illness in humans and animals, with death occurring in 40 to 70% of cases” according to the CDC. A federal judge has ruled that Walgreens contributed to the opioid crisis in San Francisco by dispensing ”hundreds of thousands of red flag opioid prescriptions without performing adequate due diligence.” The sort-of twist is that the ruling is that it’s the company’s fault, not the employees’: “The evidence showed that Walgreens did not provide its pharmacists with sufficient time, staffing, or resources to perform due diligence on these prescriptions.” Walgreens said it plans to appeal, and that it didn’t actually make or market the pills — it just didn’t keep track of how many it was dispensing. Your enemies are in prison, your friends are all French ambassadors. Now it’s time to think: What new pharmacy-related laws should Georgia have? GPhA needs your ideas as our advocacy team prepares for the 2023 legislative session. Our best legislative priorities come from members. You folks are on the front lines, after all, but you have to tell us. And GPhA gets it done with an unmatched record of results: Most of these ideas came from members who told someone on the advocacy team, “There oughta be a law.” If there’s a law or policy issue you want to see changed — something that will improve patient care or the practice of pharmacy — tell us about it! It’s super easy — barely an inconvenience: E-mail your idea to VP of Public Policy Melissa Reybold at mreybold@gpha.org. Yes, it’s that simple. “Dear Ms. Reybold, there’s one law I think Georgia really needs….” Give as much info as you can without boring her. All right, we’ll make it a little harder: You have to do it by 5:00 pm this coming Saturday, August 13. The latest drug that will upend the antibiotic landscape is … fabimycin. Never heard of it? That’s because it’s a new compound developed at the University of Illinois at Urbana-Champaign. Chemists there took an antibiotic that worked against gram-positive bacteria, did a little science to it, and created one they say works against those nasty gram-negative bacteria. And really well, too, fighting off 300 drug-resistant bacteria. “[Fabimycin] proved potent against more than 300 drug-resistant clinical isolates, while remaining relatively inactive toward certain gram-positive pathogens and some typically harmless bacteria that live in or on the human body.” Will we ever hear of it again? After more research, perhaps. Saliva of veterans suffering from Post Traumatic Stress Disorder contains a specific microbiotic signature. That is, it might be possible to test someone for PTSD by looking for a particular combination of bacteria in their saliva. Fun side facts: The Israeli researchers who discovered this also noted that 1) “the saliva bacteria of those exposed to air pollution showed a correlation to the picture with PTSD,” and 2) more education seemed to provide a “protective influence.” “New Study: 36% of YouTube Videos Contain Misleading Hay Fever Information” (The real shocker: “43% of videos on allergic rhinitis contained useful information.”) People with higher levels of cholesterol and fatty acids in their blood are more likely to suffer longer from diseases, and that includes being more likely to have long Covid. British researchers found that, Covid or not-Covid, if someone’s symptoms took longer to disappear, they were like to have the same pattern of harmful fats in their blood. “The blood markers in asymptomatic people had a healthier pattern that we know is associated with a lower risk of heart attacks and diabetes. The people with long-lasting symptoms showed higher levels of ‘bad cholesterol’ and unhealthy fatty acids.”Walgreens gets blamed, fast PTSD test, trusting YouTube videos, and more
Here we go again?
Walgreens loses in SF trial
Imagine you’re a tyrant

The next next antibiotic
Saliva test for PTSD
Captain Obvious says “Gesundheit”
Bad blood, long symptoms
August 11, 2022 ✒ Andrew Kantor
“Almost a Third of Patients Don’t Take Drugs as Directed” says a new study out of Canada, and if that many Canadians aren’t taking their meds, can you imagine what it’s like here? In a study that examined more than 200,000 patients and 91,000 unique prescriptions, overall nonadherence rates ranged from 13.7% for patients prescribed antidepressants to 30.3% for patients prescribed antihypertensive therapies. What’s the problem? It might be cost (Canadians’ healthcare is paid for by the government, but not prescriptions), but the researchers say that they just don’t know. “We assume that people are following our instructions. We’re often giving people second and third prescriptions before we even check if they’re taking their first one.” Get 20 hours of CE (!), the world’s best update on immunization skills, and a certificate to impress your patients — all from GPhA, starting August 21, with APhA’s Pharmacy-Based Immunization Delivery: A Certificate Program for Pharmacists. This ever-popular certificate training program prepares pharmacists with comprehensive knowledge, skills, and resources necessary to provide immunization services to patients across their lifespan — skills you need now more than ever. Sunday, August 21, 2022 8:00 am – 5:00 pm Georgia Pharmacy Association Classroom CLICK HERE for more information and to register! When a drug maker tests a drug, one thing it probably doesn’t consider is the patients’ posture. And yet (Johns Hopkins researchers realized), all those fluids churning around the stomach must have an effect. “When the pill reaches the stomach, the motion of the stomach walls and the flow of contents inside determine the rate at which it dissolves. The properties of the pill and the stomach contents also play a major role. So they built … StomachSim, a stomach-simulation computer program. (Sorry, “a biomimetic in-silico simulator based on the realistic anatomy and morphology of the stomach.”) Their goal is to use it to figure out how the position of the stomach might affect the absorption of medication — “unique insights into the complex physiological processes behind the oral administration of pills.” When it comes to improving how asthma patients use their inhalers, who do you think is a good choice? Why yes, as a matter of fact it is pharmacists. Granted, the folks at the Cleveland Clinic did more case studies than study-studies, but their conclusion sure makes sense. They tested the effect of having a pharmacist demonstrate and check inhaler technique before hospital discharge, then again at a follow-up visit. Result: Fewer errors and fewer problems. Fun facts: “exhalation before inhalation” was the most common error, followed by patients not holding their breath after inhalation. A new international study found that “a median of about 66,000 people are infected with [SARS-related coronaviruses] each year in Southeast Asia,” and that “suggests that bat-to-human SARSr-CoV spillover is common in the region, and is undetected by surveillance programs and clinical studies.” The good news: Many of those strains that infect humans “may not be able to replicate well in people, cause illness, or be transmitted sufficiently among people to cause an outbreak.” The bad news: “Many.” (Above link goes to the paper in Nature Communications. For the short news story, click here.) Giving fluoroquinolone to patients with chronic kidney disease increases their risk of an “adverse event” — and higher doses lead to higher chances. What kind of adverse event? We’re talking hospital visits for “nervous system and psychiatric disorders, hypoglycemia, or […] collagen-associated events.” The rate isn’t high, thankfully — around 0.9% on a low dose or 1.2% on a higher one, but still, that’s 1 out of 100 patients being hospitalized, and it’s not considering fluoroquinolone’s other possible side effects: aortopathy, arrhythmia, hyper- or hypoglycemia, neuropathy, or tendinopathy. This suggests, say the Canadian researchers who did the study, “that fluoroquinolones should be prescribed cautiously and at lower doses among older adults with advanced CKD.” British bioscientists say they’ve found a way to treat a cause of asthma, rather than just its symptoms, and it could lead to long-term treatments. The target: pericytes, stem cells in the lining of blood vessels. During an asthma attack, they move to the airway walls and then do what stem cells do — they turn into other cells. Like, for example, muscle cells, which tend to block the airways. What the Brits found is that 1) pericytes get the signal to move to the airways via a protein called CXCL12* and 2) a molecule called LIT-927 can block that signal. Asthmatic mice that were treated with LIT-927 had a reduction in symptoms within one week and their symptoms virtually disappeared within two weeks. The researchers also found that the airway walls in mice treated with LIT-927 were much thinner than those in untreated mice, closer to those of healthy controls. The usual mantra: “[F]urther research is needed before we can begin to test this in people,” including determining dosage, timing, what other effects LIT-927 might have, and what cool name they can give it. Combining drugs to treat osteoporosis (especially the postmenopausal kind) is often the best treatment. But which drugs? There’s no clear answer. Why not? Maybe because no one thought to ask the computer. Until a group of German researchers, that is. Using evidence of how bone is broken down and renewed, and how different kinds of osteoporosis medications work, they “built a mathematical model of bone renewal that predicts the effects of various osteoporosis medications in postmenopausal women.” They literally created an equation for osteoporosis: Then they tested it on various med combinations — and even the order those combinations were given. And that led to a surprising (and useful) finding: They […] found that combinations that cause the most rapid increases in bone density do not always strengthen bone in the long term and can instead cause a rebound of accelerated bone loss after the treatment stops. The end result wasn’t The Answer for the best meds combo for osteoporosis. The goal is to inform clinical trials that can confirm what the computer came up with, and hopefully design personalized treatment plans. Is prolonged skin-to-skin contact the only way it spreads? (Not exactly.) And how did the virus change to make this outbreak different? (It didn’t.) The details are in “What scientists know — and don’t know — about how monkeypox spreads” from Stat.Electronic stomach, lots more SARS infections, teaching to inhale, and more
I thought it would have been higher
Pharmacists: Your hot immunization date is coming
SimStomach
Teaching technique
Something to look forward to in an upcoming season
Fluoroquinolone risks
Hitting asthma at its source
* Also a droid in the upcoming series, “Star Wars: Random Background Characters” on Disney+
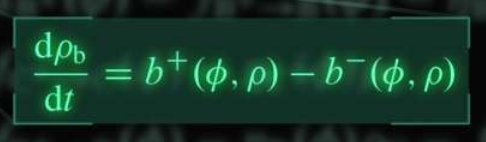
Drug combo equation
The Long Read: The Spread of Monkeypox edition
August 10, 2022 ✒ Andrew Kantor
On the latest list of “50 Highest Paying Medical Jobs in the U.S.” that is, just below prosthodontists and just above optometrists. (Topping the list are cardiologists and anesthesiologists, if you’re thinking of a second career.) Optum (the PBM) is going to be offering Sanofi’s insulin products at $35 a month for people who don’t have health insurance. All they have to do is go to the Optum Store (essentially the retail pharmacy), “get qualified,” and they’ll get a card allowing them to get Sanofi insulin for $35 at any retail pharmacy. Could Optum be doing this out of the goodness of its heart? Maybe. But then there’s this: “A mail service option will soon be available for people who prefer home delivery through the Optum Store.” We reported, you decide. So what exactly does the soon-to-pass Inflation Reduction Act mean for Medicare pricing and drug companies? The folks at the Kaiser Family Foundation have a handy chart. (It’s part of a deck of charts and info on the effects of the bill.) Remember, if you’re against allowing Medicare to negotiate drug costs, they’re price controls; if you’re in favor of the new rules, they’re spending controls. Something for everyone! That’s what an Argentinian research team found after studying long Covid and cognitive impairment in about 766 people, most of whom tested positive for Covid-19. The connection became clear. “All the subjects that had a severe cognitive impairment also had anosmia. We established an association between olfactory dysfunction and cognitive performance and impairment.” And their analysis showed which way the cause-effect went: “[S]everity of anosmia, but not clinical status, significantly predicted cognitive impairment.” Why this is the case, well, that’s not clear. Yet. At the moment, though, maybe you shouldn’t let someone make major life decisions if they’ve lost their sense of smell. The body uses a hormone called aldosterone to regulate salt and water (this is good). Too much of it, though, like any good thing, is a problem. For patients with chronic kidney disease, it can lead to kidney failure. It gets worse. The Boston University researchers who discovered this also found that “aldosterone plays a role in the progression not only of [chronic kidney disease] but also heart and blood vessel problems*.” [E]ach doubling of aldosterone concentrations in the blood was linked to an 11% increased risk of CKD progression. […] The risk was similar regardless of whether or not patients also had diabetes. The good news is that the existing kidney drug finerenone can counteract the overabundance of aldosterone and help prevent that kidney disease from getting worse. Good news! A combination of aspirin and an anti-platelet agent (e.g., ticagrelor) works a treat to prevent clotting after coronary artery bypass surgery. Bad news! A combination of aspirin and an anti-platelet agent (e.g., ticagrelor) “carries a significant risk of clinically important bleeding” after coronary artery bypass surgery. “So,” said the cardiothoracic surgeon and lead author of the study, “the benefit comes at a price.” The advice: “Physicians should base their decisions on patients’ individual circumstances.” Charlotte’s Web could’ve had a very different ending. (Psst: Soviets did it.) Pfizer is getting ready to start phase-3 trials of the Lyme disease vaccine it bought from Valneva (soon to be called the “Pfizer vaccine,” of course). Millions of hikers and lawn-mowers across the country await the results. They tested both two- and three-dose regimens and found that three doses works better — that’s what they’ll be testing now. (Doses two and three are given two months and six months after the first, in case you’re interested.) Obligatory: There was once a Lyme vaccine (Lymerix), but thanks to a combination of anti-vaxxers, hypothetical side effects, price, and a bit of sensationalism, it was pulled from the market in 2001. The retailer got itself a strongly worded letter because some third-party sellers — whose products were fulfilled by Amazon — were selling mole-removal products. And that’s a no-no. “There are no over-the-counter (OTC) drugs that can be legally sold for mole or skin tag removal,” the agency said, wagging a metaphorical finger. Despite the letter, at press time a GPhA Buzz investigation* found you could still buy the stuff: “Eating grapes could hold remarkable potential for health benefits” … according to a study funded by the California Table Grape Commission.When long Covid means dementia, clot-busting dangers, zombie pigs, and more
Pharmacists are #25
PBM to provide $35 insulin
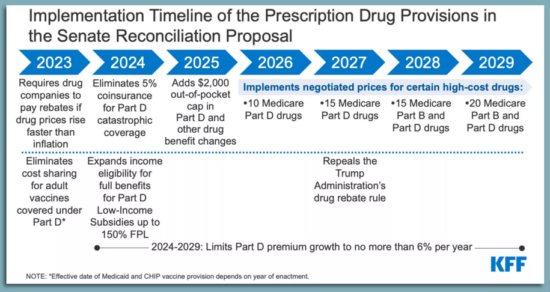
Medicare changes in a chart
Stop. Can you smell the roses?
The kidney disease hormone
* Because aldosterone activates the mineralocorticoid receptor, which can lead to high blood pressure, among other issues. But you knew that.
Should you call the clotbusters?
ICYMI: Some (zombie) pig
Lyme vax almost ready for prime time
FDA slaps Amazon
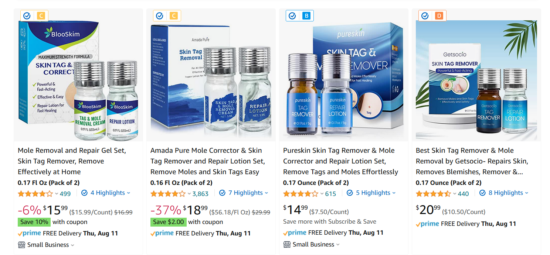
* I searched on “mole removal” on Amazon
It annoys me that these stories get press coverage without a disclaimer
August 09, 2022 ✒ Andrew Kantor
Current wisdom: Insulin resistance (through unknown-as-yet mechanisms) causes changes in the endothelial cells lining blood vessels, and that leads to fat buildup and cardiovascular disease. But what if that’s (as the headline says) backwards? That’s what researchers at Boston’s Joslin Diabetes Center are suggesting. Their finding: That it’s the endothelial cells in control and driving metabolism, rather than being on the receiving end. In a reversal of scientific dogma, the findings suggest that vascular dysfunction may itself be the cause of undesirable metabolic changes that can lead to diabetes, not an effect as previously thought. And then, to complicate matters, there’s a sort of feedback-ish loop in effect. Problems with the endothelial cells lead to insulin resistance (they found). That’s problem one. Problem two: Insulin is also what comes back to those same endothelial cells and causes them to produce nitrous oxide. Nitrous oxide triggers the production of brown fat cells — the good fat. So … 1) problems in blood vessels lead to 2) insulin resistance, then insulin resistance 3) means those blood vessels produce less nitrous oxide and 3) that means less calorie-burning brown fat. Or, as the chief researcher put it, “Everything is connected.” With demand for the Jyenneos smallpox vaccine skyrocketing, the FDA is considering allowing one dose to be split into fifths, quintupling the supply. How can that work? By giving it intradermally instead of subcutaneously. “There’s some advantages to intradermal administration, including an improved immune response to the vaccine,” [FDA commish Robert] Califf said. “It’s important to note that overall safety and efficacy profile will not be sacrificed with this approach.” The American Society of Health System Pharmacists is asking HHS to allow pharmacists to deliver the smallpox/monkeypox vaccine (via a PREP Act declaration, like with Covid vaccines) to make it easier for people to get it. You know the reasons; no word from HHS yet. If you’re a gang member or mob boss, scars are good. If you’re trying to pump insulin, no so much. The problem: Implantable insulin pumps are a great idea, but the immune system will attack them, form scar tissue around them, and eventually clog the pump. MIT engineers came up with an unusual solution: They surrounded the pump with a balloon that could be inflated and deflated. It doesn’t need to be often, either — just every 12 hours, in testing, was enough to drive away the immune cells that lead to scar tissue formation, like trying to paint a balloon that inflates before the paint can dry. And while scar tissue did form eventually — you can only fool Mother Nature so long — the collagen fibers were aligned, which (they believe) allowed the meds to get through anyway. It’s been tested on mice and cadavers, so (live) human tests are next. The big news this weekend was the passage of the Inflation Reduction Act of 2022. Despite the headlines, there were actually wins on both sides of the aisle when it comes to the pharma-related portion of the bill. For Democrats, CMS will finally be able negotiate drug prices like the rest of the world … on 10 older drugs that don’t yet have a generic version. That’s all. (The bigger deal is that it’s a foot in the door of drug-price negotiation.) But Republicans got wins too, although they’re being overshadowed by the press around the price-negotiation news. The GOP prevailed by preventing the imposition of a $35 out-of-pocket cap on insulin on private insurance plans, as well as in other, non-pharma parts of the bill (e.g., there will be no requirements for paid family leave, nor funding for universal preschool or an expansion of the child tax credit). As for price negotiations, despite one side saying it will mean unicorns and rainbows and the other predicting angry dragons and rains of despair, chances are the effects will be, like the weather, partly cloudy or partly sunny. Cats predicting death. Dogs detecting Covid. They are sooooo last year. Now we have the world premiere of “Locusts Detecting Cancer.” Locusts, it seems, can distinguish between cancer cells and normal cells and even distinguish different kinds of cancer. And as tempting as it may be to send swarms of locusts through doctors’ offices*, the reality is boring: “[T]his work could provide the basis for devices that use insect sensory neurons to enable the early detection of cancer using only a patient’s breath.” This’ll be a Big Deal soon enough: In an effort to get their hit of nicotine, teens are turning to gum, lozenges, and gummies, often flavored just for them (mmm, “fruit medley”!). They contain plenty of drug, are easier to hide in school than vapes, are entirely unregulated, and are now second in popularltiy only to e-cigarettes , according to research out of USC. It’s almost as if companies want to hook them on an addictive drug while they’re in middle school. Latest on the list of “what can vitamin D do for you” is … reduce inflammation. Maybe. The whole cause/effect thing isn’t entirely clear. When you’ve got chronic inflammation, the liver produces more C-reactive protein. But (say Aussie researchers), if you take vitamin D, the levels of that protein go down. Their conclusion: “[T]he findings suggest that boosting vitamin D in people with a deficiency may reduce chronic inflammation.” But note the weasel words “suggest” and “may.” That’s because there’s a black box in operation here. Does vitamin D affect the inflammation, or could it be affecting the protein? Or maybe it’s backwards — low C-reactive protein means lower vitamin D? Right now there seems to be a connection, but more work is needed to figure out just what it is. A problem with many vaccines is that they don’t last long once they warm up. That’s why the whole cold chain thing is such a big issue. The result, say Swiss researchers, is that half of vaccines go to waste. So, being Swiss, they came up with an elegant solution. It’s a hydrogel — “a biocompatible, synthetic polymer known as ‘PEG’ that serves as a protective, ‘cloaking device’” for large molecules like vaccine proteins. So instead of wrapping the vial in a blanket of cold that has to be maintained, the Swiss wrap the individual molecules in the polymer, which can keep the proteins safe up to about 150°F. And to remove the coating? Just dissolve it with a sugar solution. It’s still in the lab phase (i.e., “more research is needed”) but the Swiss Federal Institute of Technology is already flinging around Buzz’s favorite phrase: “game changer.”What the locusts smell, splitting the pox vax, hot nicotine candy, and more
Could we have the diabetes/heart disease connection backwards?
Monkeypox vaccine update
Five-for-one split
What about you?
Pump it up (the implant, that is)
Everybody wins … sort of
A useful plague of locusts
* Especially during Passover
Next in nicotine
Can D do this too?
Making vaccines last
August 06, 2022 ✒ Andrew Kantor
Here’s a weird one: People who have a high level of the protein prostasin in their blood are significantly more likely to have diabetes. Why? The Swedish and Chinese researchers who discovered the connection aren’t sure. Is it somehow helping cause the diabetes? Is it a marker for a different cause? Regardless, “those with the highest levels of prostasin […] were almost twice as likely to have diabetes than those with the lowest levels.” But wait, there’s more. Those who also had a high level of blood sugar (perhaps the were already diabetic) were at much higher risk of dying from cancer. For every doubling in prostasin concentration, the risk of cancer death rose by 24% in those without high blood sugar, and by 139% in those with high blood sugar. The diabetes-cancer connection was already known, but this might give insight into the mechanism. And it certainly makes for a blood test to pay attention to. Wondering which animals around the world have been infected with Covid-19? There’s now an interactive dashboard for that. As adding fentanyl to street drugs becomes passé, the latest deadly additive is … xylazine. Yeah, the animal tranquilizer is showing up (ironically) as an additive to fentanyl and cocaine. It started being reported in Puerto Rico, Philly, and now Massachusetts (in anywhere from 28 to 90% of the drugs tested — but we all know it won’t be long before it’s everywhere. The danger is not that someone might OD on xylazine, but that, as a sedative, it will make an opioid overdose worse by slowing the heart. There’s a lot of speculation about how and why xylazine is on the rise. It may be added to fentanyl or heroin to help extend the effects of an opioid high. Dealers also may be using this relatively inexpensive and easy-to-order sedative because of supply chain gaps with other drugs. Oh, yeah, and it’s not easily detectable with a test strip (like fentanyl) nor affected by naloxone. Moderna says it’s considering turning its mRNA-vaccine muscle toward making monkeypox vaccines. It depends, of course, on whether cases continue to rise and spread and, presumably whether those deep government pockets will be where the payment comes from. “Our platform is pretty well established and our ability to rapidly scale has been demonstrated. If we were to go after a monkeypox clinical development program, it would be to very quickly progress toward an approvable set of endpoints in a clinical study.” But can the mRNA tech handle that large monkeypox viral protein? Perhaps we’ll find out. People who have an opioid-abuse problem aren’t getting the meds they need to quit. In fact, say NYU researchers, “Almost 90 Percent of People with Opioid Use Disorder [are] Not Receiving Lifesaving Medication.” Part of the problem is obvious: More than 70% of residential treatment programs don’t offer methadone, buprenorphine, or extended-release naltrexone — drugs that can cut (or potentially eliminate) half or more of overdoses while helping people quit. “We need to rethink how treatment for opioid use disorder is delivered, eliminate stigma, make it easier for people to enter and remain in treatment, as well as ensure that all treatment programs provide and encourage use of evidence-based medications that we know save lives.” The most reliable info to date on long Covid: 1 in 8 people infected end up with it. That’s based on a Dutch study of more than 76,000 people and 23 symptoms that are officially (or semi-officially) associated with persistent symptoms. What makes this study different is that the Dutchies took into account that some of these symptoms existed before Covid infection, so they can’t really be attributed to long Covid. (“Symptoms such as fatigue and headaches might be worsened during the pandemic also in people without Covid-19, for example.”) There are lots of ways to try to tackle the issue of antibiotic resistance including phages (see below) and augmenting or repurposing old drugs. But Aussie researchers have an new idea: proteins. Specifically, they’re looking at guanylate-binding proteins, which the human immune system uses as one of its weapons to kill bacteria. By themselves or combined with antibiotics, GBPs could be — after much more research of course — another new weapon. Resistance may eventually be futile after all. “We are now finding more and more GBPs that can kill different types of drug-resistant bacteria. This includes bacteria that can cause meningitis, pneumonia and sepsis. […] The ultimate goal is to use these proteins to eliminate meningitis, pneumonia and sepsis entirely.” Bacteriophages — bacteria-killing viruses — are one of the most promising tools against drug-resistant germs. But once you introduce them to kill the bacteria, you start an arms race between the good viruses and the bad bacteria. Israeli and German microbiome researchers have a possible solution, and it almost seems obvious: One phage good? More phages better! Looking to fight gut inflammation, they’re “using a cocktail of phages that use multiple lines of attack against Klebsiella pneumonia bacteria, preventing them from evolving resistance to the mixture.” And because phages target a single bacteria (unlike broad-spectrum antibiotics) this cocktail doesn’t affect anything else in the gut. The downside? Phages have to be found, and it took them five years (“a a painstaking fishing expedition”) to isolate phages that attack K. pneumonia. Congress is set to pass the “Inflation Reduction Act” which would allow Medicare to negotiate the prices of [insert drumroll] a whopping 10 drugs … in 2026. That would go up to a staggering* 20 drugs by 2029. (For comparison, the rest of the world can negotiate the prices of every drug.) The pharmaceutical industry is against the bill, of course, threatening to stop trying so hard to develop new drugs if their executives and shareholders face lower paychecks.Move over, fentanyl; 12.5% long Covid; a flag for diabetes, and more
A marker for diabetes (and cancer)
What else has Covid?

After fentanyl
mRNA for monkeypox
The addiction drugs they can’t get
Quickie Covid data
Killing bacteria
A new kind of germ killer
You can’t fight the phage cocktail
A tiny change to drug pricing looms
* This is sarcasm.
August 05, 2022 ✒ Andrew Kantor
It’s 3:00 am and you’re not in a Denny’s mood. How about getting a Covid test instead? Good news: The Georgia Department of Public Health has opened a bunch* of 24/7 kiosks throughout the state offering free tests. (Here’s the map.) Fill out the quick form and the kiosk dispenses a kit. Swab, dip, etc., and put it back in the kiosk. The next day it’ll be picked up and given a super-accurate PCR test — you’ll be notified of the results by email or text. Pharmacists, do you have enough continuing ed under your belt to renew your license? If not, no worries — GPhA has ways of Gives you 23.0 hours of CPE (in person plus home study)! In-person sessions: Sunday, August 21 —or— Sunday, December 11 (8:00 am – 5:00 pm) in GPhA’s Sandy Springs classroom Click here for details and to register. Gives you 21.0 hours of CPE (in person plus home study)! Live via Zoom; Sunday, September 18 (8:00 am – 5:00 pm) Click here for details and to register. Gives you 20.0 hours of CPE (in person plus home study)! In-person session: Sunday, October 2 (8:30 am – 12:30 pm) in the GPhA Sandy Springs classroom Click here for details and to register. A big GPhA Buzz shout-out to GPhA member Al Dixon of Richmond Hill Pharmacy in Bryan County, who was featured in a WSB-TV story on rising drug prices. Specifically, it was based on AARP of Georgia s reminding everyone that drug prices have risen “73% in the last seven years, hurting Georgia’s seniors.” And who’s to blame? PBMs. (Yeah, the article misspelled his name. Over and over. ) The CDC is expected to update it’s don’t-get-Covid guidelines in the next few days “to ease quarantine recommendations for people exposed to the virus and de-emphasize 6 feet of social distancing.” It’s also going to “de-emphasize regular screening testing for Covid-19 in schools” and stick with its test-to-stay strategy. All this, of course, assumes that there won’t be a major surge when students return to school and an unexpected definition of “cultural studies.” It’s now officially a public health emergency in the US. That just means more hyperactive news stories … and more importantly, “Federal health officials can now expedite preventative measures to treat monkeypox” and have some more flexibility in how they do it. Luckily, it’s rarely fatal (but very uncomfortable) and only spread through intimate skin-to-skin contact. There’s a monkeypox vaccine (although it can be hard to get), but what about treatments? One that’s out there is TPOXX (aka tecovirimat) which is approved to treat monkeypox’s nasty cousin, smallpox. And while TPOXX has been tested for monkeypox on animals, it’s still officially an investigational drug when it comes to humans. So if you want to use it here in the US of A, that means paperwork. Lots of paperwork. Will that change now that this is an emergency? Should it? Read on. The Brits have identified new symptoms of the disease. Upon reading the headline, I thought to share those new symptoms with you. Upon reading the article, however, I prefer to simply provide the link. For those of you who clicked and read, here’s a picture of a bunny and a kitten: Some moles don’t know their place. Rather than sit still and maybe be the subject of an awkward glance, they start to grow until they become melanoma, the really bad skin cancer. Why do some have to be that way? Who hurt them? Who did this to them? Boston University researchers think they know. If they’re right, it could open the door to treatments not only for melanoma (and pre-melanoma) but potentially other types of cancer. It’s all about the Hippo tumor suppressor pathway which, to oversimplify, tells cells when to stop growing. When the Hippo tumor suppressor pathway is itself suppressed, “those cells rapidly go on to form melanoma in multiple experimental models.” Keep it working properly, and moles stay moles. Next up, as always, more research. CVS announced that it’s joining Amazon, Walgreens, and that group of hobos under the bridge and getting into the primary care business. The company wants to offer longer hours at its doctor [sic] offices so people can visit as early as 6 a.m., as late as 9 p.m., or on the weekends. Completely unrelated, America’s physician shortage continues to the point that Time magazine is offering solutions. Also unrelated, a new study out of the University of Chicago found that “It would take a primary care physician 26.7 hours per day to follow national recommendation guidelines for preventative, chronic disease and acute care for an average number of patients.” The Brits are simply not satisfied with how well bleach works to kill germs. It’s just too slow. A northern-England hospital had an idea: a disinfectant based on hypochlorous acid, a natural compound that also comes from chlorine and is used in the U.S. as a disinfectant. They call their product Pathisol, and researchers at Teesside University (home of Barry the Beaver) are testing it in a clinical environment for the first time, misting entire wards with the stuff. The benefit, if it pans out: “Pathisol can disinfect a surface in two minutes, which is five times faster than bleach. It can also kill 99.99% of pathogens, including hospital superbug Clostridium difficile.” It’s also cheaper to make than bleach and more environmentally friendly — and you get to apply with a cool spray gun.CDC relaxes (for now), CVS has big plans, Georgia gets Covid-testing kiosks, and more
Covid kiosks
* We didn’t bother to count.
It’s a license renewal year
making you talk helping you meet your requirements tout de suite, and get some spiffy certificates for your wall while you’re at it.APhA’s Pharmacy-Based Immunization Delivery Certificate Training Program
APhA’s Delivering Medication Therapy Management Services Certificate Training Program
NASPA’s Pharmacy-based Point-of-Care Testing Certificate Program
You can call him Al
CDC say relax
Monkeypox updates
Urgent, urgent, emergency
Whither TPOXX?
Eeew

When moles go bad
CVS on the bandwagon, but who’ll drive it?
Disinfecting: Better, stronger, faster



