September 07, 2024 ✒ Andrew Kantor
Pfizer and Valneva are very happy about the results from a phase-2 trial of their Lyme disease vaccine. Specifically, it was for a booster given a year after the initial shot. Not only did subjects show “strong immune responses” from the booster (good for patients), but the trial shows that they’ll probably need an annual shot to keep up with the disease (good for the bottom line). At-home sphygmomanometers* are great for the home-health kit, but cuff sizes can be a big issue. How big? A new study out of Johns Hopkins found that “the standard arm-size ranges for these devices won’t appropriately fit millions of U.S. consumers.” Yes, yes, mostly the cuffs are too small, but it points to a potentially bigger issue: Patients may not realize the fit is a problem and thus get erroneous readings. Some products come with multiple cuffs, while others (like one at Buzz HQ) include a coupon for a free larger cuff. If you’re selling them, it might be worth a word about accuracy. * I have to brag. I spelled that right on the first try. People with type 2 diabetes who take SGLT-2 inhibitors are less likely — 35% less likely — to develop dementia than those who take DPP-4 inhibitors. (That’s what came out of a Korean study of 220,000 people with type 2 diabetes who were followed for about 2 years.) Why would this be the case, though? What’s the connection? An Australian dementia expert looks into it. When it comes to uncomplicated respiratory infections, a shorter course of antibiotics is probably all you need. There’s been mixed evidence supporting these shorter courses, so Dutch researchers decided to find the answer once and for all (until the next study, anyway). What they found, in broad strokes, is that previous studies showed “moderate-quality evidence that 5 days of antibiotics is clinically non-inferior to a longer course” for either mild community-acquired pneumonia or acute exacerbation of COPD. The number of the counting shall be five, though — ‘evidence for shorter durations was scarce.’ Potential big caveat — the source material the Dutchies used wasn’t great: “[T]he quality of the reviews was generally low and the quality of evidence varied between type of infection.” Some kids are still given first-generation antihistamines — think chlorpheniramine maleate, hydroxyzine hydrochloride, or piprinhydrinate — usually for runny noses, itching, or, you know, to get them to fall asleep. But that might not be a good idea. According to a study out of Korea, because these drugs cross the blood-brain barrier, they affect brain waves and result in a higher risk of seizures. In particular, they can induce symptomatic seizures, affect electroencephalographic (EEG) activity and seizure thresholds in adults with inherent seizure susceptibility, and alter resting EEG activity. An editorial accompanying the paper highlights the questions this study brings up, from “How should a relatively small risk translate into clinical practice?” to questioning whether newer antihistamines have similar effects and “Should antihistamines be avoided altogether in younger children?” We’ve often said that 95% of all diseases are either caused by inflammation or gut bacteria. Now Mayo Clinic scientists have developed a way to check #2. It can’t diagnose a specific disease, but it can analyze the bacteria and determine healthy vs. not so healthy with about 80% accuracy. The process was simple in the age of AI: analyze 8,000 samples, tell the computer which belong to healthy people, and let it learn. The tool, called Gut Microbiome Wellness Index 2, could detect even subtle changes in gut health, identifying whether a person may be progressing toward or recovering from a disease. Because it’s AI-based, the researchers themselves don’t necessarily know what constitutes a healthy gut biome, just that the computer can sort it out for them.BP cuff problems, fighting diabetes (and dementia), annual Lyme vax boosters, and more
Lyme vax update
Goldilocks and the BP cuff
The Long(ish) Read: Diabetes and Dementia edition
5 is enough
Old antihistamine, new seizures?
Gut check
September 06, 2024 ✒ Andrew Kantor
The FDA has approved Novavax’s updated non-mRNA Covid shot for the FLiRT variants circulating nowadays. While there’s a good argument for waiting on this year’s flu shot — the season doesn’t peak for a couple of months — getting the latest Covid shot now makes sense, what with cases continuing to tick up across the country. It’s gotten worse, not better, for supplies of Novo Nordisk’s Ozempic, the company said, especially for lower, starter doses. The company also expects intermittent shortages for all strengths to continue “into the final quarter of 2024 due to increased demand and along with capacity constraints at some of its manufacturing sites.” In other words, while there’s plenty of semaglutide out there (as compounding pharmacists know), Novo can’t seem to get the filling and manufacturing of its spiffy Ozempic pens on track. It is — well, was — one of the weird bits of medical trivia: Scientists knew that morphine worked, but they didn’t know how. And now they do. Apparently, Swedish scientists found… … morphine affects a selected set of neurons in the brain in the part called the rostral ventromedial medulla (RVM). Together, these neurons form a kind of ‘morphine ensemble’. This is a group of neurons whose change in activity leads to pain relief. They’re hoping that knowing exactly how morphine works can lead to a similar type of pain reliever that doesn’t come with morphine’s baggage. (If you want more details, the paper’s abstract is available here.) It’s possible — now hear me out here — it’s possible that PBM executives lied in their testimony before Congress when they defended their business models. I know, shocking, right? Apparently what the PBM CEOs said turns out to contradict what the committee learned on its own, as well as Federal Trade Commission research. Ruh-ro. James Comer (R-KY), the chair of the House Committee on Oversight and Accountability, is Not Happy At All about this. During the hearing, [PBM CEOs] Conway, Kautzner and Joyner testified that their PBMs treat affiliated and unaffiliated pharmacies equally when setting rates, negotiating contracts and telling patients where to dispense their medications. Those statements were lies, suggests Comer’s letters, which cite committee and FTC evidence to argue that PBMs increase revenue at their own pharmacies at the expense of other businesses. Comer has threatened them with fines (i.e., “the price tag for lying to Congress”) or even jail time. So how can they avoid a trip to the Big House? By … correcting their statements. The first cluster of cases has been reported. It’s among workers at two poultry facilities in Colorado. Still no human-to-human transmission, though, and the workers are all doing fine. As you were. The AARP is very happy about upcoming annual caps on Medicare out-of-pocket drug costs. The association had the numbers crunched and found that the Biden administration’s $2,000 cap “will lower prices in 2025 for more than 3.2 million people, or around 8.4% of Part D beneficiaries who do not receive other subsidies.” Even better, more than a million older people will save more than $1,000 a year. Before the Inflation Reduction Act, beneficiaries who did not qualify for low income subsidies were required to pay 5% of drug costs regardless of how much they had already paid.PBMs caught with their pants on fire, Ozempic to stay in shortage, understanding morphine, and more
Third Covid vax approved
Ozempic shortage to continue
How morphine works
Say it ain’t so, PBMs
Bird flu watch
Seniors poised to save big
September 05, 2024 ✒ Andrew Kantor
The DEA is increasing the production limit for brand-name Vyvanse and generic lisdexamfetamine by 24%. That’s good news for a lot of people who’ve been having trouble getting their ADHD drugs. The new production limit is also good news for the 11 companies that make lisdexamfetamine, which has been in shortage since October 2022. For reasons unknown, people taking Wegovy didn’t die from Covid complications as often as the rest of us according to a big international study led by Harvard Med. People on Wegovy still got Covid, and at the same rate as people randomly assigned to take a placebo. But their chances of dying from the infection plunged by 33 percent, the study found. In fact, the study found that treating obesity reduced death from all causes, suggesting “that lower life expectancy among people with obesity is actually caused by the disease itself.” Still, Wegovy had a much bigger effect on Covid deaths — “It’s something more than just losing weight,” said one cardiologist. Like the headline says, as neffy hits the shelves as an alternative to EpiPens, what do you need to know? Glad you asked; a pediatric allergy and immunology specialist has your answers. When’s the right time to take hypertension meds? That depends on who you asked and which study you read last. Now Canadian researchers say they have the answer: It doesn’t matter. The Canucks ran a two-part trial, one with 3,400 adults out in the wild, and one with 776 older patients in nursing homes, all of whom were taking BP meds. Result: No difference in major cardiovascular events. There did seem to be an advantage in older folks taking their meds at bedtime — a 26% lower rate of “all-cause unplanned hospitalisation/ED visits.” Despite that last bit, the lead researcher said that timing isn’t important. “We can now dismiss the treatment timing as being important and advise patients to take their BP medication when they are least likely to forget.” (Why he would say that, considering the lower all-cause hospitalizations, isn’t clear. Maybe he doesn’t like old people.) Quietly, so as not to disturb predators, Rite Aid is emerging from Chapter 11 bankruptcy, naming former exec VP and CFO Matt Schroeder as its new CEO. “I am honored to lead Rite Aid on its journey as we continue serving our customers and communities,” Schroeder said, reading from a boilerplate press release prepared by the marketing team. How can you tell when an idea is probably deeply stupid? When it starts with, “I saw on TikTok….” In this case, the American Academy of Ophthalmology is warning people not to believe claims that there are drops that can change your eye color. In short, there’s no evidence that they work (before-and-after photos of strangers don’t count) and plenty of reason to think they “could potentially harm the eye, causing light sensitivity, eye inflammation, and eventually vision loss.” As Forbes’s Bruce “No Relation” Lee points out, destroying melanin is a bad idea anyway: Melanin can help protect your eye cells against light. Plus, other parts of your eye like your retina can use melanin to function properly. Eye drops typically won’t stay in only one part of eye even if you tell them to do so. Previously, the AAO has warned people not to put food coloring or castor oil in their eyes, rub their eyelids with menthol lip balm, or use a hairdryer as an eyelash curler. Seriously. Remember way back when, when there was a fear that keeping a mobile phone glued to your ear could cause cancer? According to a review of 63 studies by the Australian Radiation Protection and Nuclear Safety Agency, you don’t have to worry*. “We concluded the evidence does not show a link between mobile phones and brain cancer or other head and neck cancers.” The review found no overall association between mobile phone use and cancer, no association with prolonged use (if people use their mobile phones for 10 years or more), and no association with the amount of mobile phone use (the number of calls made or the time spent on the phone). * Even though a lot of folks either text or hold their phones in front of them to make sure everyone in the restaurant can hear both sides of the conversation.The right time for BP meds, how to make yourself blind, Vyvanse and Rite Aid return, and more
Vyvanse is coming back (a bit)
Wegovy vs. Covid
Neffy: What you need to know
Time to take your BP med
Rite Aid returns

It don’t make my brown eyes blue
Call me, maybe (but really, you can)
August 31, 2024 ✒ Andrew Kantor
A study funded by AbbVie found that its CGRP inhibitor Ubrelvy (aka ubrogepant) can stop a migraine from progressing if you take it as soon as the early warning signs appear. About 24 hours after taking the pill, 65% of those who took ubrogepant reported that they had little to no migraine symptoms, compared to 48% of those who took a placebo. Because today, August 31, is, like, technically the deadline. Head over to GPhA.org/renew if you haven’t, lest someone have to take … measures. Here’s a surprising correlation: Giving older people antidepressants (specifically bupropion or escitalopram) can reduce their risk of falling — that is, if they have depression. A study out of the University of Pittsburgh of 100,000 Medicare patients found that those given bupropion (Wellbutrin) had a 26% lower risk of falls, while those given escitalopram (Lexapro) had a 17% lower risk. Sure there were concerns of drowsiness as a side effect, but the researchers say the risk of untreated depression is worse. And yes, it’s the meds — psychotherapy didn’t help with falls. Cigna’s Express Scripts PBM won’t pay for Humira starting next year. Following CVS Caremark’s lead, it’s “removing branded Humira from its largest commercial formularies come 2025 in favor of biosimilar options from Teva, Sandoz, and Boehringer Ingelheim.” The newest entry (that we know of) into the world of wearable health-monitoring devices is a smart mask that monitors your breath for respiratory ailments like asthma, COPD, and post-Covid infections. In case you were unaware that you had asthma, COPD, or a post-Covid infection. What the Caltech engineers who made it say makes this mask different is that it actually “can analyze the chemicals in one’s breath in real time.” Snark aside, obviously it’s not meant to detect whether you have one of those conditions, but rather whether it’s acting up or if your medication is working. It’s currently in proof-of-concept stage, but the materials to make it cost about a buck per mask. While not called a game-changer, the Caltech folks do call it “a new paradigm.” ICYMI, the FDA has a new mandate: Retailers must verify the age of anyone under 30 when they try to buy tobacco products — until now it was under 27. That means you have to look at someone and think, “Do they look under 30?” rather than “Do they look under 27?” They might reduce the risk of glaucoma. A study out of the University of Utah found that after 1–3 years “Patients treated with a GLP-1RA agonist had a 41-50% lower risk of developing primary open-angle glaucoma or ocular hypertension than those taking metformin. (Earlier this year a group of those shifty Danes found something similar.) Want some science? Here you go: The agents have been shown to reduce inflammation and oxidative stress, improve neuronal survival and function by activating signaling pathways to enhance cellular resistance and reduce apoptotic cell death, and mitigate inflammatory responses in the retina. Sandwiched neatly between type 1 and type 2 diabetes is … anyone? That’s right — type 1.5 diabetes. Two Aussie boffins explain what that means.Migraine-blocking pill, breath-analyzing mask, the diabetes you might not know, and more
Stopping migraines before they start
Have you renewed your GPhA membership yet?
Keeping the elderly upright
Express Scripts pulls Humira
A different kind of breathalyzer
Under 30? ID, please
GLP-1s’ next trick
The Long Read: Stuck in the Middle
August 29, 2024 ✒ Andrew Kantor
Taking a cue from compounding pharma, Eli Lilly is going to offer Zepbound direct to cash patients. It won’t be in the fancy injectors, but in standard vials with plain ol’ needles … and at a deep discount: $399 for a month of the 2.5 mg dose and $549 for a month of the 5 mg. The decision is likely because Lilly can’t supply those injectors right now (hence the shortage), so this way they can cut into the compounding marketplace. So much for “lower prices will kill innovation.” Side note 1: Lilly raised the cash price of its Zepbound pens from $550 to $650. Side note 2: Like Taylor Swift tickets, Zepbound is technically “available,” but officially still in shortage — good luck actually getting it. Pfizer is launching its own direct-to-consumer platform called PfizerForAll. It has coupons for Pfizer meds and then uses online pharmacy Alto Pharmacy to fulfill orders. Need a prescriber? No problem — telehealth company UpScriptHealth is part of the deal. Need a consultation to help you make decisions? Not sure how to use your meds properly? Will that Pfizer drug interact with your other prescriptions? Having a side effect? Well … good luck with that. Are you ready for 2024’s biggest event for Georgia pharmacy technicians? Mark your calendar for Saturday, October 19 — it’s a day of socializing, networking, and learning — developed by pharmacy techs for pharmacy techs. One low price* gets you breakfast, lunch, 4 hours of CE, a professional headshot, and the networking event at the 57th Fighter Group restaurant in Atlanta! Back in March we told you that the FDA has approved Dexcom’s Stelo — the first OTC continuous glucose monitor. Now the Stelo is available at stelo.com “for adults 18 years and older who are not taking any insulin therapies.” Dexcom has pitched the Stelo as a more “health-focused” version of its top-of-the-line CGM, the G7, which made its debut early last year. Though built on the same sensor platform, the Stelo will operate without the low blood sugar alerts or software features needed by people with Type 1 diabetes. The FDA has approved Insulet’s Omnipod 5 automated insulin delivery system for people with type 2 diabetes. (It has previously been approved for people with type 1.) [A] wearable, tubeless product provides up to three days of nonstop insulin delivery without the need to handle a needle. The Omnipod 5 integrates with a continuous glucose monitor to manage blood sugar with no multiple daily injections, zero fingersticks and can be controlled by a compatible smartphone or by a controller. “Knowing you have a brain aneurysm may raise anxiety risk” Old idea: Most cases of pancreatic ductal adenocarcinoma (PDAC) don’t trigger an immune response, making immunotherapy ineffective. New news: Scientists at Cold Spring Harbor Laboratory found that PDAC does trigger a response, but there’s no point as the immune cells can’t actually get inside the tumors to do any good. (Science: The tumor has a “defensive wall” made of two proteins—CXCR4 and CXCL12.) Breakthrough (literally): Using folinic acid causes the body to produce more type-I interferons. Those interferons then … “…acted like trail markers, highlighting a way past PDAC’s defenses. Cancer-killing immune cells that had been kept outside the wall were able to slip into the tumor and start fighting back. Now knowing about that defensive wall (and how to break it), they hope to develop therapies to take advantage of it. Bird flu, m It’s bad enough that, even with pollinator populations crashing, Massachusetts is doing mass spraying of insecticide. Yikes.Automated glucose management, Captain Obvious is worried, drugmakers go DTC, and more!
Lilly sells Zepbound DTC
Pfizer says “I’m in, too!”
TechU is back!
* Just $40 for GPhA members, $65 for non-members
Glucose automation
OTC CGM goes on sale
Automate the insulin
Captain Obvious has enough to worry about
Breaking pancreatic cancer’s ‘wall’
Here, something else to worry about
onkeypox, sloth fever, election stress … not enough for ya? How about human cases of eastern equine encephalitis? It’s about 30% fatal, and there’s no vaccine and no treatment. So far it’s just in the Northeast, but how long will that last?
August 27, 2024 ✒ Andrew Kantor
A couple of weeks ago we told you about neffy, the nasal-spray epinephrine alternative to EpiPens that was approved by the FDA. Apparently there was one liiiiiiitle bit of info left out — info that has prescribers a bit unsure about it. “[S]tudies have not yet been done on people who are in the throes of life-threatening allergic reactions, known as anaphylaxis.” That makes sense — although the FDA approved neffy for anaphylactic shock, that wasn’t tested. (You can’t ethically trigger an anaphylactic reaction, even in grad students.) And it’s possible someone’s nose could be clogged, preventing the med from getting in. And then there’s American exceptionalism: “[D]octors say they may avoid prescribing the new spray just after it hits the market, in part because they would need to devote employee hours to getting on the phone to press insurance companies to cover it.” Still, neffy has a lot going for it. It has a longer shelf life (two years!). The cold doesn’t bother it anyway. Neither does the heat; no special storage is required. Nor is training beyond “Find your nose,” which studies have shown most people can do*. Got it in one * “[neffy maker] ARS found no harm to the eyes if the user accidentally squirts the medicine into them.” The latest universal flu vaccine candidate comes from [puts on blindfold, spins globe] the Cleveland Clinic’s Lerner Research Institute. Their tack: Go big. First, they used a database to look at thousands of strains of the flu and (using the scientific version of Ctrl-F) found which amino acids are present in every strain of the influenza virus. With that info, they identified eight proteins from the H1, H2, H3, H5, and H7 types — “It’s like creating a greatest hits album” — that they used to create a whopper of a vaccine. They called the process COBRA, for Computationally Optimized Broadly Reactive Antigens. Then they tested the vax on mice, and it worked. Which means they’re looking at beginning human testing; they’re hoping to launch clinical trials within the next few years. They’re also hoping their protein-finding technique can be used for other viruses. Two Georgia hospitals that have closed — the urban Atlanta Medical Center and the rural Southwest Georgia Regional Medical Center — might have a new lease on life thanks to bipartisan legislation that eased the certificate of need rules for building new hospitals. Speculation has already begun for which 15 drugs CMS will mark next for price negotiations. It’s required to release that list by February 2025, and the negotiated prices will take effect in 2027. Topping the list (and keep in mind this is all speculation) is Ozempic. Remember, it’s only approved for diabetes, and it’s been on the market since at least 2017. Other possible 2027 candidates include Pfizer’s cancer drugs Ibrance and Xtandi, GSK’s asthma and chronic obstructive pulmonary disease (COPD) treatment Trelegy Ellipta, Teva’s Huntington’s disease treatment Austedo, and Abbvie’s irritable bowel syndrome drug Linzess, according to five analysts as well as researchers and company executives. These are what taxpayers, via Medicare, spend the most on. Ozempic alone costs so much that it has a noticeable effect on the deficit: “Medicare spent over $4.6 billion on the drug in 2022.” Covid’s picking up, so HHS is renewing the ‘free tests by mail’ program. Starting next month, people will be able to order four free tests via covidtests.gov. “CVS Health has recently overtaken Walgreens as the most popular drugstore retailer among drugstore/pharmacy shoppers.” (But “It’s not clear whether CVS will be able to sustain this lead.”) What’s with semaglutide and suicidal thoughts? The current answer is “There might be a link, but there might not be.” During trials of another GLP-1 agonist, liraglutide, researchers found a tiny increase in suicidal ideation among patients (0.3% compared with 0.1% of those taking placebo). But when semaglutide hit the mainstream, more reports came in — back in January we told you that that the FDA was looking into some reports. The latest is … dueling studies, both based on worldwide health data, albeit from different sources. One in January did “not support higher risks of suicidal ideation with semaglutide.” But another, which came out this month, found there was a disproportional amount of suicidal thoughts among semaglutide users. So what’s to be done? Keep an eye on patients, everyone says, especially those with depression or an anxiety disorder. And, of course, do more research. Nasal epinephrine questions, negotiating Ozempic?, CVS takes top spot, and more
Neffy iffyness

Always a few years away
The Long Read: Local (non-pharma) hospital news
What’s next for drug-price negotiations?
Short takes
Free Covid tests are back
In case you care
GLP-1s suicide connection?
August 24, 2024 ✒ Andrew Kantor
As expected, the FDA has given emergency use authorization to update Covid-19 vaccines from Pfizer and Moderna. They should be available within the next few weeks. For people five and over, a single dose of the new vax will do the trick, but for kids 6 months to 4 years old the number of shots is based on whether they’ve been vaccinated before — see the FDA release for details. Getting the Covid vaccine after infection seems to protect patients — at least primates — from hyperglycemia, one of the (many) issues faced by people who develop long Covid. Tulane University researchers “found that administering the Covid-19 mRNA vaccine four days after infection showed a significant positive effect on blood sugar levels that was sustained over time.” They’re thinking that the Covid vaccine might be indicated for treatment for at least some of Covid’s long-term issues, although it’s not clear yet how quickly you would need to get the shot for it to be effective. GPhA is offering its top-of-the-line immunization course for techs — the aptly named “GPhA’s Immunization Delivery Training for Pharmacy Technicians” — twice in the next couple of months. Techs, you want this training (and the spiffy certificate it comes with). Respiratory virus season is coming up fast, and immunizations will be in demand. What does it cover, you ask? The latest info on flu and Covid-19 vaccines, how to give those jabs the right way (of course), the legal details of tech vaccinations, a bit of background on vaccines and immunology, practical stuff like ordering vaccines with inventory management standards, billing and reimbursement, and the documentation you need to use. (Whew!) The course will also help you sit for PTCB’s Advanced Skill Exam, and yes, it’s ACPE accredited for 8 hours of CPE, which includes 5 hours of self-study. Two sessions to choose from: Saturday, September 21, 2024 Jekyll Island Convention Center, Jekyll Island, Ga. 9:30am – 12:30pm — or — Sunday, October 20, 2024 GPhA World Headquarters, Sandy Springs 9:30am – 12:30pm Cost: GPhA Members: $199; non-members: $235 (which includes a full GPhA membership through December 31, 2025 … but only if you live in Georgia) More info: Hit up GPhA.org/techimmunization. If you’ve thought to yourself, “I wonder which exotic fruit might help treat non-alcoholic fatty liver disease,” a group of researchers in Quebec has got your back. The answer, they say, is the camu-camu — or at least its extract. The Quebecois did a basic test: Over 12 weeks they gave 30 participants either some camu-camu extract or a placebo, then used an MRI to measure their liver fat. Scientists observed a 7.43% reduction in liver lipids when study participants took camu-camu extract. With the placebo, they noted an 8.42% increase in liver fat. (Emphasis ours for clarity.) They think it’s because the camu-camu’s polyphenols boost certain gut bacteria, and that bacteria “metabolizes the large polyphenol molecules that cannot be absorbed by the intestine, transforming them into smaller molecules that the body can assimilate to decrease liver fat.” Next up: seeing whether camu-camu and cranberries can work together to get even better results. You want to be a pharmacist, but your mother has her heart set on your becoming a lawyer. Well there’s good news from UGA — you can do both. Starting this fall, UGA will offer a Pharmaceutical Sciences and Juris Doctor (BS/JD) degree program, “for students with a passion for pharmaceuticals and law, offering an accelerated pathway to earn both degrees in just six years.” A real-world test of Merck’s Ebola vaccine in the Democratic* Republic of the Congo “was 84% effective against infection during the country’s 2018-2020 Ebola outbreak,” according to a study by French and DRC researchers. Previously the vaccine had only been tested in clinical trials. * Uh-huh. We’ve talked about all the benefits of drinking coffee (i.e., not just caffeine, but coffee in particular), and now a British biomedical professor puts it together in “All the reasons a cup of coffee really can be good for you.” The latest life expectancy numbers show that Georgia ranks #41 in the country, with a life expectancy at birth of 74.3 years. (Hawai’i is #1 at 79.9 years, while Mississippi is at the bottom at 70.9 years.) “Study reveals best exercise for diabetes patients” is the headline. Annoyingly, the story takes more than 200 words to get to the answer(s): moderate aerobic exercise. For men, either continuous or interval aerobic exercise will reduce blood glucose, while for women only continuous exercise showed the same benefit. You’re welcome.Who needs camu-camu, post-infection Covid vax, UGA’s double degree, and more
Covid vaccine news
In other vaccine news, though…
Technicians! Get your immunization training now!
The deets
Fruit for the liver

Two degrees above zero
Short Takes
Ebola vaccine worked
Coffee compilation
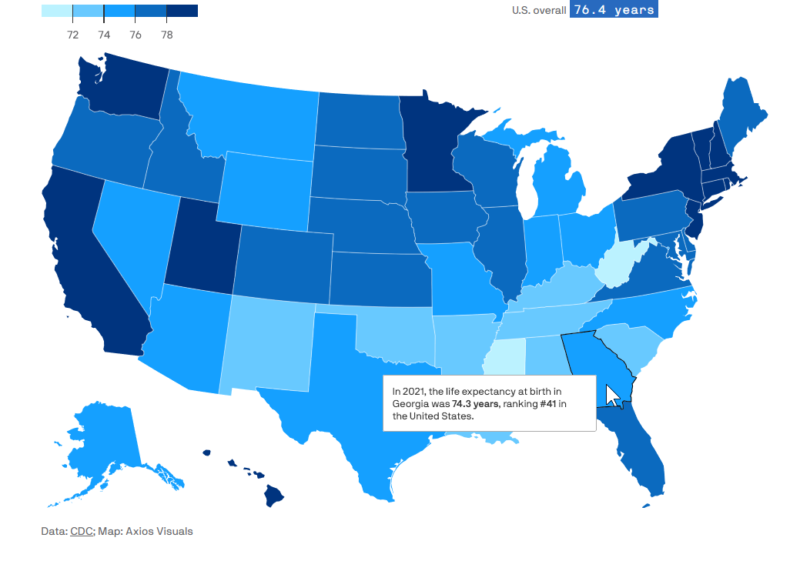
Live long and prosper (but maybe in Hawai’i)
Saving you a click
August 22, 2024 ✒ Andrew Kantor
By the time you read this, the FDA may have approved this year’s Covid-19 vaccines. These will be targeting the KP.2 variant — one of the FLiRT clan. Pfizer’s and Moderna’s seem to be on track for approval, but Novovax’s non-mRNA shot is still up in the air. ICYMI, Covid has been … well, “surging” might be a bit strong, but “picking up steam” is a good description, so the sooner the better. Researchers at the University of Colorado think they’ve found another clue to what causes long Covid. The disease leaves behind antigens that can stick around for a year after the infection is cleared. Those antigens, the Coloradoans say, cause cortisol levels in the brain to drop and even stay down. Their hypothesis, based on a rat study: Covid antigens lower cortisol, which serves to keep inflammatory responses to stressors in check in the brain. Once a stressor arises—whether it be a bad day at work, a mild infection or a hard workout—the brain’s inflammatory response is unleashed without those limits and serious symptoms come screaming back. They don’t think cortisol treatment would help (“they would not get at the root cause and come with a host of side effects”), but finding where those antigens are hiding and eliminating them could be an effective treatment. The Georgia Department of Public Health reports a fifth case of measles this year — this one’s in the Atlanta. In a shock to no one, the patient wasn’t fully vaccinated. “DPH is working to identify anyone who may have had contact with the individual while they were infectious.” Not only can a placebo work, it can work even if the patient knows it’s a placebo. Not only can a known placebo work, it can even work (to reduce stress, at least) when administered remotely — i.e., when patients’ only interaction with the prescriber is via Zoom. That’s what Michigan State researchers found when testing the non-drug’s effect during the pandemic to help reduce stress. Half the 64 participants got no treatment, while the other half (“non-deceptive placebo group”) got education about placebos and then the placebos themselves, which they were instructed to take by an online practitioner. Result: “[T]he non-deceptive group showed a significant decrease in stress, anxiety, and depression in just two weeks compared to the no-treatment control group.” To protect the newborns of people with opioid use disorder, it’s better to treat the pregnant moms with a combo of buprenorphine and naloxone rather than buprenorphine alone. That comes from a study of 8,700 pregnant women over 18 years. “According to the authors, buprenorphine/naloxone exposure during pregnancy was associated with a lower risk for neonatal abstinence syndrome” as well as NICU admission. Eli Lilly claims “slashed the risk of developing type 2 diabetes by 94% in adults with prediabetes who also are obese or overweight” in a three-year study. What’s interesting is that once they stopped, although the patients gained back the weight they lost, their risk of developing diabetes was still cut by 88%. Per the American Society of Health-System Pharmacists:Placebos keep working, measles comes home, when tirzepatide keeps working, and more
Here come the Covid vaxes
Long Covid clue
Measles in Georgia
Good news about nothing

Naloxone, opioid abuse, and pregnancy
Tirzepatide’s newest trick
Latest drugs in shortage
August 20, 2024 ✒ Andrew Kantor
Several companies are working on a combination flu/Covid-19 vaccine, but now another candidate seems out of the running. The Pfizer/BioNTech shot worked great against Covid and influenza A, but it failed to work against influenza B in a phase-3 trial. CureVac and GSK had the same problem with their mRNA flu vax, as did Sanofi. Interestingly, though, both Pfizer and Moderna have separate mRNA flu vaccines that do seem to work against influenza B, but for whatever reason they can’t be combined with the Covid shot. The companies are now back in the lab, thinking about what they’ve done. It’s that time of year — GPhA membership dues are up for renewal! Great news: As a part of our 150th anniversary next year, we’re extending membership benefits for an extra three months! That means when you renew your membership by September 1, 2024, your membership won’t expire until December 31, 2025 — that’s three months of membership FREE. Zilch. Nada. Bupkis. Not enough? How ’bout this: Dues are the same for 2024–25 — no increase. Watch your email and snail mail for your renewal information and invoice. Or you can pop over to GPhA.org/renew to renew there. We’re glad you’re a member, and we’re counting on you to continue being one, and to be a part of all of the celebrations in store to commemorate GPhA’s 150 years as the Voice of Pharmacy in Georgia! Some people get Covid or the flu and barely notice, while some end up in hospital or even dying. It feels like a crapshoot, but that might not be the case. A new Australian study looked at what the sickest people had in common. What they found is high levels of one enzyme called oleoyl-ACP-hydrolase — Olah to its friends — in the sickest patients. As one immunologist put it: “[I]n some patients who develop life-threatening disease, Olah is produced at substantially higher levels, whereas we find very low levels in healthy individuals and patients with mild disease.” What can be done with this info isn’t clear yet, but just finding the correlation is worthy of, as always, more research. The current outbreak of mpox might be worth keeping an eye on. This clade (clade I) is a lot more infectious than the one that spread last time (clade II). Perhaps more importantly, it’s already been seen in at least a couple of patients outside of Africa — and authorities in Pakistan lost track of the one guy there. You may have seen that the FDA has given approval to the first at-home test for syphilis, but what you may not have caught is the big caveat that comes with it. The test won’t actually tell you if you have syphilis — it’ll tell you if you (probably) don’t have it. That’s because “positive test results from this test alone are not sufficient to diagnose syphilis infection and should be followed by additional laboratory testing.” One big reason: “Results of this test will be positive for individuals previously diagnosed with syphilis, even if they were successfully treated.” So it’s useless if you’ve ever had syphilis before. If it’s negative it means you’re probably okay. And if it’s positive it doesn’t mean you have syphilis, just that you need to get tested for real. Gabapentin is technically supposed to be used for seizures and diabetic nerve pain, but lately it’s being used for … well, for a lot of conditions, even if there’s hardly any evidence that it works. (And some older patients just keep taking it, even if they don’t remember why.) You might think of ustekinumab as a psoriasis treatment, but a new British study found that it might also help children diagnosed with type-1 diabetes by protecting the function of pancreatic beta-cells and slowing the disease’s progression. The science-y detail: “Ustekinumab was associated with a 49% higher C-peptide AUC at week 52 [vs placebo].” One way to help a chronic wound heal more quickly is to use an electric current, but that’s an expensive proposition. People with diabetes dealing with those are at risk of amputation. If only someone could create a cheap, disposable bandage that produced a small electric current. Hearing that call were engineers at NC State*. They created a tiny, flexible, water-powered electrical wound dressing. The dressing is applied to a patient so that the electrodes come into contact with the wound. A drop of water is then applied to the battery, activating it. Once activated, the bandage produces an electric field for several hours. Because they’re flexible, they can fit over irregularly shaped wounds, and when tested on mice the bandages healed wounds 30% faster than regular dressings. And the cost? A couple of bucks apiece. * As well as Columbia, Beth Israel Deaconess Medical Center, UNC, Georgia Tech, and Korean researchersSyphilis test limitations, Covid/flu shot fails trial, healing with electric bandages, and more
Combo shot setback
Dues are due!
File under: “Huh, that’s interesting”
What to know about mpox
Syphilis test reality check
The Long Read: Gabapentin edition
The X for Y Files
Do androids dream of electric Band-Aids?
August 17, 2024 ✒ Andrew Kantor
So many ripples: Snack food companies were looking at sales losses because of GLP-1 drugs. Medicare/-caid worried about how they were going to afford them. Orthopedic surgeons were looking at fewer patients. Now those drugs are getting so popular they’re affecting the kinds of buildings healthcare companies are considering building or buying. Health facilities are rethinking bariatric surgery and even cardiology and orthopedic centers and in favor of consumer-friendly “facilities focused more on lifestyle and metabolic health.” UGA just onboarded 146 new Doctor of Pharmacy students at its White Coat Ceremony. Here they are, looking all fresh-faced and innocent, not knowing yet what awaits: Fun fact: The female to male ratio of the class of 2028 is 3:1. People paying out of pocket for Mounjaro found that — because a high-dose pen costs the same as a low-dose pen — breaking one open and splitting the dose can save a lot of money. Sure there are risks, but if you can split a high-dose pen into six doses, as some patients do, you’ve cut the price by [does math] 83%. As one splitter put it: “For me, that’s really just a harm-reduction principle. There are so many people this drug could be so life-changing for, but it’s just utterly, ruinously expensive.” If you have low levels of magnesium, you’re at risk for DNA damage that can make you “more susceptible to Alzheimer’s and Parkinson’s disease, gastrointestinal diseases, a range of cancers, and diabetes.” That’s according to Aussie molecular biologists who found that when magnesium levels were low, patients had higher levels of homocysteine, an amino acid that happens to damage DNA. “Our study showed a direct correlation between low magnesium levels in blood (less than 18mg/L) and increased DNA damage, even after adjusting for gender and age.” Next step: Figure out the optimum levels and dietary intake. Getting shingles just once can raise someone’s risk of “long-term confusion and memory loss” — and thus a career as a politician — by 20 percent. That comes out of a 17-year meta-study of almost 150,000 participants (25 to 75 years old) by researchers from Brigham and Women’s Hospital. They aren’t sure why this is happening, but they speculate it could be because of “neuroinflammation, direct neuron injury, or the activation of other herpesviruses.” You’ve obviously heard the news that the Medicare price negotiations will be saving taxpayers something like $6 billion a year (and seniors “should save $1.5 billion in out-of-pocket costs when the price changes take effect in 2026”). If you’re curious about the nitty-gritty details of the drugs, the prices, and the process, CMS has a 4-page PDF that explains it all. One of the ways the Inflation Reduction Act helps seniors is by capping how much they have to spend on prescription drugs. But that means insurance companies have to spend more, and they aren’t going to take that sitting down. So they’re raising Medicare premiums. In response, to stick to the original goal (keeping seniors’ costs down), CMS is planning to give those insurers $15 per month for each patient to keep those premiums down, which will cost the government $5 billion the first year. That said, the numbers from the price negotiations are still in taxpayers’ favor: The nonpartisan congressional scorekeeper Congressional Budget Office estimated that the drug pricing negotiation provisions in the IRA will reduce Medicare spending by $98.5 billion over 10 years. Shingles and dementia, Medicare money in and out, GLP-1s and real estate, and more
GLP-1 drugs hit real estate
Congrats to UGA’s new coat-wearers!

Hacking Mounjaro
Have you checked your magnesium?
Luckily there’s a vaccine
How Medicare saved billions
6 billion forward, 5 billion back