January 20, 2024 ✒ Andrew Kantor
GPhA is one of dozens of state* and national pharmacy organizations that signed a letter expressing their concern about Florida’s plan to import some drugs from Canada. The program, they say, “could open the door for harmful and counterfeit drugs to enter our nation’s drug supply, with no evidence that this will result in cost savings for our patients.” How could Canada’s drug supply be harmful, you ask? Aside from the maple flavoring added by law, the issue is the US’s Drug Supply Chain and Security Act — aka “Track and Trace” — that essentially creates a closed drug-distribution system here. It means a bottle’s pedigree can easily be checked, and counterfeiting is much harder. “Canada does not have a similar law,” the letter points out, “leaving our drug supply chain at risk under Florida’s program.” * 43 states plus DC and Puerto Rico, and including our friends at the Georgia Society of Health-System Pharmacists It’s a small advance, but it’s a critical one: Duke researchers working on HIV vaccines have confirmed that their vaccine designed for monkeys can “induce broadly neutralizing antibodies” against HIV. The “broadly neutralizing” is the important bit; it indicates that the antibodies aren’t necessarily monkey-specific. The “antibodies generated in the animals were structurally and genetically similar to the antibodies needed in humans.” The next steps will involve developing it into a vaccine candidate for human testing. Men taking Cialis, Levitra, or Viagra along with a nitrate “had a higher risk of heart failure, early death, and other negative health outcomes” than those taking just the nitrate, according to a Swedish study of more than 60,000 men with a history of heart issues. The issue, it seems, is that both meds can cause a drop in blood pressure, although the study didn’t look at the details. The blood-pressure issue was known, but now there’s Swedish confirmation that yes, taking them both can kill you. But perhaps you’d die happy. There’s a silver lining to the push to vaccinate seniors during respiratory virus season: After they shuffle into the doctor’s office, they tend to stay to get a checkup. “These are seniors, many of whom have not been to the office for a long time, they’ve come back in, they’ve now got vaccinated, their physicians have picked up other things while they’ve been there.” This came from a report by UnitedHealth Group that explained in part why health insurers’ stock prices took a hit — they’re having to pay for all that extra health care. (Of course, it’s an ounce of prevention that’s going to save them in the long run, so everybody wins.) “Seniors Who Smoke Weed & Drive Are Road Hazards: Study” Score one for the anti-vax crowd: More measles outbreaks are happening in the US — the latest are in New Jersey, DC, and Philly* — and experts are expecting more to come as local vaccination rates dip below the level needed for herd immunity. Currently measles is officially “eliminated” in the US, but if outbreaks continue for more than a year we could lose that designation. Our prediction: Eventual lawsuits against anti-vax organizations. * Think that’s up north and Georgia is safe? Think again. It’s not news that marijuana can lead to the munchies. (Just ask the Girl Scouts selling cookies.) But until Washington State University researchers took it upon themselves to, you know, research the issue, we didn’t know why. Now we do. After trying to get mice to smoke tiny joints, the neuroscientists settled for using vaporized cannabis, then scanned their brains. (The mice’s, not their own.) Cannabis, they found, activates certain neurons that are normally dormant. [T]he cannabinoid-1 receptor, a known cannabis target, controlled the activity of a well-known set of “feeding” cells in the hypothalamus, called Agouti Related Protein neurons. […] When these neurons were turned off, cannabis no longer promoted appetite. Quick! Justify this research! It “could pave the way for refined therapeutics to treat appetite disorders faced by cancer patients as well as anorexia and potentially obesity.” But first, more research is needed…. * Agouti Related Protein neurons, since you asked A gastroenterologist at the University of Washington explains how the right foods (and the right gut biome) can let your body make its own GLP-1. Free Ozempic!Why pot causes munchies, Viagra-nitrate danger, Florida plan gets national pushback, and more
Pharmacy orgs: Don’t trust Canadian drugs
Step towards an HIV vaccine
Don’t mix ED and chest pain meds
They come for the vax and stay for the checkup
Captain Obvious avoids the left lane
More measles are coming
Munchies explained

The Long Read: How gut bacteria help with weight
January 18, 2024 ✒ Andrew Kantor
Here’s one way to nudge doctors to be careful how they prescribe opioids: Send them a letter every time one of their patients dies from an opioid overdose, and — and this is important — include “a plan for what to do during subsequent patient visits.” USC researchers already knew that a letter informing prescribers about the death of a patient was effective in cutting prescriptions, but now they found it’s even better to give some advice, too. (Kind of like telling a child, “Don’t give the new puppy a chocolate bar. Give him a dog cookie instead.”) Compared to just a notification… … physicians who received notifications with additional planning guidance reduced prescriptions of opioids by nearly 13%. They also reduced prescriptions of the anxiety medications benzodiazepines by more than 8%. (Side note: You know you can trust the research because the lead author is Doctor Doctor.) Medical University of South Carolina medical researchers found that giving spinal surgery patients a dose of N-acetylcysteine (NAC) during surgery reduced their need for post-surgery opioids. In the 48 hours after surgery, patients who were administered NAC via IV infusion received 19% fewer opioid doses on average than patients who received saline. They had less pain, too, and waited longer to request pain meds. Side note: Some early studies have shown the NAC can keep heroin addicts from relapsing. “Can we stop giving opiates completely?” asked the lead researcher. “Likely not. Can we decrease the amount patients need? We should try.” If you have patients with COPD, they shouldn’t be taking gabapentinoids. Drugs like gabapentin and pregabalin already have a warning about the potential for severe breathing difficulties, but there wasn’t a study on the effects on patients with COPD. Now there is. Researchers at Canada’s McGill University combed through the patient data of more than 13,500 patients with COPD and found that gabapentinoid use was associated with almost a 40% increase in “severe COPD exacerbation.” Notably, problems surfaced on average about 6 months after beginning gabapentinoid treatment, so the association might not come to mind. This coming Friday, January 19, is the deadline for submitting nominations for the 2024 Georgia Pharmacy Association Awards. You have two days to tell us who’s the best pharmacist, technician, or student you’ve ever met. Nominate someone for one, two, or more awards that’ll be presented at the convention on Amelia Island. You haven’t waited too long … yet. It takes just a few minutes to describe why someone is deserving, so please take a few minutes and tell us about that awesome pharmacy pro! University of Iowa biomedical engineers found a surprising thing: Smokers did better on autophagy-inhibitor cancer treatment than non-smokers did. Huh. What was one difference between the two? Carbon monoxide; smokers have a lot more of it in their systems. “[T]his suggested that elevated carbon monoxide might improve the effectiveness of autophagy inhibitors.” So how can they deliver carbon monoxide to test their idea? Sticking mice into an exhaust pipe from a ’72 VW Beetle is one way, but a cooler idea is to concoct a drinkable, gas-entrapping foam where the trapped gas is carbon monoxide. (They went with plan B.) When mice with pancreatic and prostate cancers were fed the carbon monoxide foam and simultaneously treated with an autophagy inhibitor, tumor growth and progression was significantly reduced in the animals. It also worked on human cancer cells in the lab, so maybe “safe, therapeutic levels of CO” can be given to patients taking autophagy inhibitors — via a foam or a few hours on I-85. Flu activity dropped a bit for the first time in a while, according to the CDC. It might be a one-week blip or — hopefully — a sign that the season is finally fading. The disturbing news: 13% of kids (especially girls) have tried a nonprescription drug or supplement for weight loss, and the percentage has been going up over the years. The kids have been using whatever they can — diet pills, laxatives, and diuretics, none of which is good for them (unless, you know, they actually need them). “Not good for them” meaning that using these products actually leads to “low self-esteem, depression, poor nutritional intake, and substance use.” Do we need to explain why they’re doing this? Fine. It’s a combination, say the Aussie researchers who did the study, of … ”. . . low self-esteem, parental influence to lose weight or parental dissatisfaction with weight, self-body dissatisfaction, peer groups who value thinness, and media or social media influences promoting unrealistic beauty standards.” Oh, social media, what haven’t you done for us? Antibiotics, it seems, can lead to little kids turning into, shall we say, ‘larger kids.’ Actually it’s a combo of antibiotics and a high-fat diet. If young kids are exposed to both, they run a greater risk of obesity, adiposity, and metabolic dysfunction. The reason, found Vanderbilt University microbiologists, is good ol’ gut bacteria — specifically, the phenyllactic acid that one Lactobacillus bacteria produces. Phenyllactic acid normally tells the epithelial cells of the intestine to ease up on packaging and secreting fat, but when the bacteria aren’t there to produce it, more fat enters circulation. So could you give kids some phenyllactic acid or Lactobacillus bacteria when they get antibiotics? Maybe. But that, as you can imagine, will require some more research.Who should drink carbon monoxide, the combo that fattens kids, tough love for opioid prescribers, and more
How to cut opioid prescribing
Speaking of opioid use…
Gabapentinoids and COPD don’t mix
Last chance to submit a nomination!

Unexpected cancer-drug booster
Quickie flu update
Kids are all about weight loss (and that’s bad)
Guts, bacteria, fats, and kids
January 16, 2024 ✒ Andrew Kantor
This is a Big Deal: It seems that there isn’t a single “Alzheimer’s disease” but rather multiple versions — five of them, to be specific. That’s what an international team found after examining the cerebral-spinal fluid of 600 people (and publishing in Nature Aging.) Those different subtypes have variations in how they present themselves and — critically — they react differently to treatment, including having different side effects. That might explain why treatment seems to be so hit-and-miss. This could mean some drugs only work in one Alzheimer’s type. Amyloid focused medication, for instance, may treat a subtype with increased amyloid production but potentially harm a subtype with decreased production. Obviously more research is needed, but if these findings are accurate it could upend the entire Alzheimer’s-treatment landscape. GPhA’s VP of public policy, Melissa Reybold, has penned the latest of her 2024 legislative updates. The legislative session is just getting started, so she had time to check out the Georgia Board of Pharmacy meeting, too. Read all about it! Scientists from the FDA and the National Institute on Drug Abuse have written a 250-page review and now recommend “that the Drug Enforcement Administration make marijuana a Schedule III drug, alongside the likes of ketamine and testosterone, which are available by prescription.” The DEA still considers marijuana a schedule-I drug — as dangerous as heroin or LSD and without any medical use; clearly that’s not the case. (GPhA has no official position on the legalization of marijuana, but that doesn’t mean certain facts aren’t obvious.) The review by federal scientists found that even though marijuana is the most frequently abused illicit drug, “it does not produce serious outcomes compared to drugs in Schedules I or II.” Marijuana abuse does lead to physical dependence, the analysis noted, and some people develop a psychological dependence. “But the likelihood of serious outcomes is low,” the review concluded. Still, the DEA’s position makes marijuana illegal to possess on the federal level, even though 24 states have made it legal for recreational use and 38, including Georgia, have legalized it to some extent for medicinal use. Even parts of Georgia have decriminalized it (Atlanta, Clarkston, Forest Park, Savannah, South Fulton, Statesboro, as well as unincorporated Fulton County and Macon–Bibb County), meaning possession of certain amounts is subject to the equivalent of a traffic ticket. Will this be the impetus for a federal change? We’ll see. The folks from GPhA’s Academy of Independent Pharmacy are still on their statewide “DIR Hangover Preparation Tour” — now in North Georgia. That’s where they met with Will Crowley, owner of Crowley Drug Company in Calhoun. Here we’ve got (l to r) AIP VP Jonathan Marquess; Will Crowley, PharmD; and Member Service Rep Ashton Sullivan Fun fact: Will started Crowley Drug nine years ago — from scratch! Stopping the flu virus from getting in (or getting hold) protects one person, but why not find a way to stop the virus from getting out, too? NYU researchers think they’ve found a way to do just that, which could lead to treatments that not only protect the patient, but prevent the virus from spreading. There’s been plenty of talk about viruses’ spike protein, but this research looked at the other side — the sialic acid (SA) receptors on cells that the spike protein attaches to. They used an enzyme that makes those receptors less receptive, thus keeping the virus from attaching even when it got past the immune system. [K]eeping virus particles from attaching to SAs limits more than just the entry of influenza A viral infections, but also hinders their exit (shedding) and transmission from mouse to mouse. This could keep a small outbreak from becoming large, and a large outbreak from spreading further. (Or farther. I always mix those up.) Finding a totally new use for an existing drug is always good news (because it means a shorter path to approval). One of the latest: epilepsy drugs might slow down the joint degeneration that comes with arthritis. It seems there’s a sodium channel called Nav1.7 that produces electrical impulses in muscles (and is thus related to epilepsy) but — and here’s the kicker — “the same Nav1.7 channels are also present in non-excitable cells that produce collagen and help maintain the joints in the body.” So maybe a drug that blocks Nav1.7 to treat epilepsy might also help slow the progression of osteoarthritis. In fact, Yale researchers found, it does just that: [D]rugs used to block Nav1.7 — including carbamazepine, a sodium channel blocker currently used to treat epilepsy and trigeminal neuralgia — also provided substantial protection from joint damage in the mice. Omega 3 fats, like those in fish and nuts (and, you know, supplements) keep turning out to do some serious good for people. The latest: They seem to slow the progression of pulmonary fibrosis. A study out of UVA looked at the health records of 300 people with interstitial lung disease. The researchers found… … that higher levels of omega-3 fatty acids in the blood plasma were associated with better ability to exchange carbon dioxide and longer survival without the need for a lung transplant. This did not vary much regardless of smoking history or whether the patients had cardiovascular disease. Why does it work? Dunno, so you know the mantra: More research is needed. If we were a tabloid, the headline would be “Frankincense treats breast cancer!” But we’re not. The actual story is that an extract from the tree that produces frankincense seems to slow the spread of breast cancer cells — in a small study in the lab. The extract — Boswellia — has some interesting anti-cancer properties, according to researchers at the Medical University of South Carolina. Why it works and how important this discovery is, is still up in the air. But it’s these small breakthroughs that eventually lead to the big ones. Despite it coming for our jobs here at GPhA Buzz, we kinda like playing with AI. A lot of new tools are coming out using the same technology as ChatGPT but with different data sets in their libraries. One that caught our attention is called Consensus, which lets you ask questions about research on a particular subject to see what conclusions have been reached (and the papers describing them). Essentially, Consensus has read a gadzillion research papers for you, so rather than just do a keyword search like some kind of ranch hand, you ask your question in plain English. Just for fun, we used the previous story as a test. “Can Boswellia extract affect breast cancer?” we prompted. Consensus found 10 papers that suggested that yes, it might. The summary: These studies suggest that Boswellia extracts, containing boswellic acids and their derivatives, can potentially affect breast cancer by reducing inflammation, targeting molecular pathways, and exhibiting cytotoxicity against treatment-resistant and triple-negative breast cancer cells. It’s free, so perhaps worth a gander….FDA likes C-III marijuana, plus Alzheimer’s isn’t one thing, frankincense in the lab, and more
Five kinds of Alzheimer’s
The latest legislative update
Federal scientists: Make marijuana C-III
AIP on the road

Stopping flu’s spread
An epilepsy drug — for arthritis
Omega-3s vs lung fibrosis
Frankincense is more than a perfume

Nifty research tool
January 13, 2024 ✒ Andrew Kantor
When someone over 50 gets a shingles vaccination, the second shot is supposed to come about 6 months after the first. But a new study out of Kaiser Permanente (based on records of 2 million people) found that it’s okay to wait longer — the effectiveness doesn’t change. The caveat: The study doesn’t say how much longer you can wait, just “not to panic if your second dose ended up being delayed beyond 6 months.” That second dose is important. The study found 2 doses were 76% effective against shingles, while 1 dose was 64% effective. Over the 4-year period, the 2-dose regimen waned little while the single dose waned more, dropping to 52% after the third year. With STDs on the rise in the US, it’s a bad time for a penicillin shortage. That’s what we have, though, with Pfizer’s Bicillin hard to find. That’s why the FDA is allowing a French version from Laboratoires Delbert to be imported. While not officially FDA approved, this penicillin G benzathine (called Extencilline) is pretty much the same as Pfizer’s drug, plus it’s French so it’s all fancy. Laboratoires Delbert noted that it will import 1,200,000 units of its powdered Extencilline and 2,400,000 units of the diluent version for reconstitution for injection. The meds are manufactured in Italy and both lots have an expiration date of 2025. Woo-hoo! GPhA is offering “APhA’s Pharmacy-Based Immunization Delivery: A Certificate Program for Pharmacists” for the first time in 2024: Sunday, February 25 from 8:00 am to 5:00 pm at the GPhA World Headquarters in Sandy Springs. This is the big kahuna of immunization training — it gives you a total of 23 hours of CE. The live portion (8 hours) is being held in GPhA’s classroom. The rest is self study — easy peasy. At the end you get a spiffy certificate for your wall and the important line on your CV to impress your patients and your boss. The whole shebang is $349 for GPhA members ($499 for non-members). Note: This is always a popular course, so the sooner you sign up the less your chance of being left out and being laughed at behind your back. Get to GPhA.org/immunization for the details and to register. Now! No, not just with mindfulness or by telling you to skip the party-size bag of M&Ms. The hypothalamus, it seems, sends signals to white (adipose) fat tissue: burn, baby, burn*. When mice get older, though, their hypothalami produce less of a molecule called Ppp1r17†, making the brain-fat signalling loop less effective. So scientists at Washington University School of Medicine in St. Louis found a way to activate the neurons that cause Ppp1r17 to be produced. When they gave this treatment to mice, those mice lived about 6 to 7% longer than controls — that’s the equivalent of five years longer for humans. Obviously this is in the early stages, but heck, it can’t hurt to dream about what you might do with five extra years. * The details are a lot more complex, but that’s the gist. Pregnant women only need about 500 mg of calcium a day to reduce their preeclampsia risk. “Only” because that’s a third of what the WHO currently recommends. That’s big news, especially for women in poorer countries; governments there provide supplements to pregnant women but can’t afford to give out that much calcium. A study out of India, Tanzania, and the US found that 500 mg and 1,500 mg daily were equally good at keeping blood pressure lower (although the higher dose was slightly better at reducing the risk of preterm birth). That means those countries might be able to afford to supplement women after all. Side note: It’s not clear why calcium has that effect — it might reduces contractions in the uterus to lower blood pressure — but the study included 22,000 women, so it clearly does work. Give blood. The Red Cross is appealing to everyone to take some time and donate blood — there’s a national shortage at the moment, and it’s going to get worse with so many people getting sick. The number of people volunteering to donate blood is at the lowest level in 20 years, and over the past two decades, the number who donate through the Red Cross has fallen about 40. It’s reached the point that some smaller blood centers are working with a supply that might only last a day. Click here or call 1-800-RED-CROSS to find a donation site and make an appointment. Apparently the “M” in DSM stands for “May not be objective.” It turns out that an eye-bulging 60% of the physicians who helped put together the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders “received payments from industry totalling $14.24 million.” Because of the enormous influence of diagnostic and treatment guidelines, the researchers say their findings “raise questions about the editorial independence of this diagnostic manual.” Bayer says its elinzanetant — a drug candidate designed to reduce hot flashes and improve sleep — has done well in two phase-3 trials “reducing the frequency and severity of vasomotor symptoms, also known as hot flashes, in postmenopausal women.” The company could be asking for FDA approval soon. It’ll be in the footsteps of Astellas’s fezolinetant (Veoza to its friends), which was approved last year. For the week ending December 9, 2023, 163 Americans died from the flu. And 1,614 died from Covid-19. Yes, that’s about 1/7th the weekly deaths as during the worst of the pandemic, but with fewer than 1 in 5 Americans having received the latest vaccine, a lot of those deaths were preventable. Perspective: Imagine if five airliners were crashing in the US every week — people would be pretty darned concerned, wouldn’t they? At first the headline seemed rather, well, obvious: “Reduced drug use is a meaningful treatment outcome for people with stimulant use disorders.” Of course reducing drug use by drug over-users is a good thing. But what the article is actually saying is that if someone is addicted to stimulants, just getting them to cut back is a win — you don’t have to have them quit entirely: “[A]bstinence should be neither the sole aim nor only valid outcome of treatment.” Your brain controls your fat, DSM-5 shenanigans, French penicillin is coming, and more
Shingles vax — timing doesn’t matter
La France envoie de la pénicilline
The super-popular APhA immunization course is back!
Your brain can make you live longer
† Also the name of Elon Musk’s second childCalcium vs preeclampsia
ICYMI: Blood drive

Can you trust the DSM?
Good news about hot flashes
Today’s Covid update
Captain Obvious … actually, the captain sits this one out
January 11, 2024 ✒ Andrew Kantor
Of kids taking two or more medications, what percentage do you think have drug-drug interactions? How about 21.4%? Yep, more than 1 in 5. Researchers at Children’s Mercy in Kansas City (Mo.) looked at the health data of more than 780,000 children who were taking two or more outpatient meds and had at least one trip to hospital. Of those, 21.4% “experienced one or more major DDI [drug-drug interaction] exposures.” The biggest culprits were clonidine as well as psychiatric and asthma medications, and the most common problems were “increased drug concentrations, central nervous system depression,” and irregular heartbeat. So maybe keep an eye out. Yesterday we wrote about hospitals in some states reinstating mask requirements. “None of those states are among those with the highest level of respiratory virus activity,” we said. WRONG. If our geography knowledge had been better, we would have realized that North Carolina has both the highest level of activity and some hospitals requiring masks. Some US senators are Not Happy at All with the prices of asthma inhalers — specifically, how companies are gaming the patent system to keep generics out of the market. So they’ve written a strongly worded letter (13 pages!) to let AstraZeneca, Boehringer Ingelheim, GSK, and Teva know how they feel. “It is unacceptable that Teva is charging Americans with asthma $286 for its QVAR RediHaler that costs just $9 in Germany. It is beyond absurd that Boehringer Ingelheim charges $489 for Combivent Respimat in the United States, but just $7 in France.” They gave the companies until Jan. 22 to explain how they set their inhaler prices. While we’re on the subject of asthma, read about how even a boxed warning on a drug didn’t get patients the information they needed. The F.D.A.’s handling of Singulair illustrates systemic gaps in the agency’s approach to addressing troubling side effects from medicines approved long ago — and to warning the public and doctors when serious issues arise. Flu and Covid cases are still rising and will probably do so for at least several more weeks. That is all. Loud music can hurt your hearing, and you may have assumed it was due to physical damage of the bits inside your ears that can’t be undone. Guess what? It turns out the damage is more complex, but there could be a pharmaceutical treatment. UC San Francisco researchers were investigating mutations in a gene called TMTC4 that can lead to hearing loss. What they found was that loud noises caused the same effects as the TMTC4 mutation. In both cases, hair cells in the inner ear were flooded with excess calcium, which activates what’s called the unfolded protein response (UPR) killing the hair cells and leading to hearing loss. In other words, it’s not simply physical damage to the ear that causes hearing loss, it’s this unfolded protein response. And that means, “that the UPR is a genuine target for preventing deafness.” Even better, there are already several drugs that block the UPR and can stop genetic hearing loss in animals. But no one bothered to test those for noise-related hearing loss in humans. That might change…. After listening to public comments, the FDA has finalized its guidance for direct-to-consumer drug ads. The goal is to make sure that warnings aren’t in tiny print or a rushed voice over — that they’re presented in a “clear, conspicuous, and neutral manner.” No more technical jargon. And for audio ads… FDA asks that [manufacturers] take into consideration the volume level, articulation and pacing of the audio to ensure the information is understandable. Similarly, when presenting ads on TV ads the agency states any accompanying text needs to be displayed long enough so it is easily read and that it remains on screen for as long as the corresponding audio. (Obligatory reminder that only the US and New Zealand allow direct-to-consumer drugs ads.) In the wake of the FDA’s granting Florida the right to import (some) drugs (under some conditions) from Canada, the Canadians have weighed in. Innovative Medicines Canada — which represents most of the Great White North’s pharmaceutical industry — is sorry to say … no. “Canada simply can’t supply drugs to Florida, or any other U.S. states, without significantly increasing the risk and severity of drug shortages nationwide. The U.S. market is nearly 10 times bigger than Canada’s, and allowing drugs that were intended for Canadians to be exported to the U.S. would harm Canadian patients and disrupt our health-care system.” Americans pay the highest prices in the world for brand-name drugs, but when it comes to generics, the opposite is true. They’re super cheap — and that’s a big reason behind drug shortages. Competition has driven the prices so low, there’s simply not enough profit to be made, at least in the US. As one boffin* put it, “There’s been a lot of offshoring because there is a drive to get the drugs made as cheaply as possible, so the manufacturer has a large incentive to go seek lower-cost environments.” Those environments are usually China and India, which are sorta-kinda fine for now, although…. “It’s a potential future risk. But it’s a potentially massive risk.” * Word of the day!Potential deafness drugs, FDA limits drug ads, multiple-med dangers, and more
Polypharmic kids
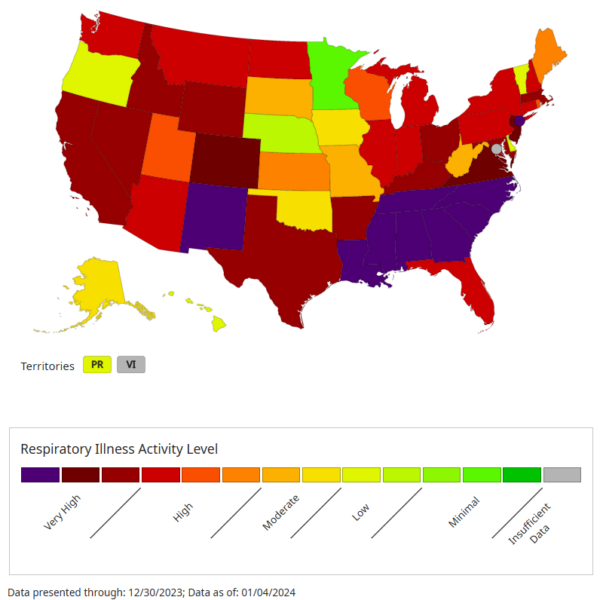
A small correction
Senators target inhaler prices
The Long Read: Unheard Warnings edition
Respiratory update
Drugs to fall on deaf ears
No more fine “print”
Drug pricing news
Canada on Florida’s import plan
America’s low prices (!)
January 09, 2024 ✒ Andrew Kantor
If you have a mouse with acne, you know how embarrassing it is for the little guy. The good news is that UC San Diego researchers have created a vaccine that reduces the inflammation of mouse acne, allowing Mickey and Minnie to feel a lot less self-conscious on prom night. We all have the Cutibacterium acnes bacteria on our faces, and it all produces an enzyme called hyaluronidase. While the friendly version of C. acnes produces hyaluronidase A, its evil, acne-causing cousin produces hyaluronidase B, and it’s HylB that causes inflammation. So the UCSD folks developed a vaccine that helps mice’s bodies neutralize just that HylB, while leaving the “good” bacteria intact. “[W]e can now have more directed and effective anti-acne therapies while preserving the healthy skin microbiome, and that is a significant advancement in acne therapy.” Who’s the best pharmacist you ever saw? How about technician? Or a student deserving recognition? You only have until January 19 to tell us — to nominate them for one, two, or more 2024 GPhA awards that’ll be presented at the 2024 Georgia Pharmacy Convention on Amelia Island. If you think, “No way he’ll win,” don’t be so sure — let the awards committee decide! It takes just a few minutes to describe why someone is deserving, and you (and they!) might be surprised. Head over to GPhA.org/awards and tell us about someone special! Head over to chat.openai.com and create a free account (it takes seconds). Then try this prompt for ChatGPT: I want to nominate someone for a pharmacy award called the [award name] given by the Georgia Pharmacy Association. Please help me write a 300-word explanation of why they deserve it. Here is the description of the award: [paste description from GPhA.org/awards here]. The person is [name] and they’re a [title at pharmacy or school]. Here are a few phrases I would use to describe them: [Type in a few sentences] Then let the AI do the work — just be sure to read over the response and make any edits. You’re welcome! Georgia’s flu levels are “very high” according to the DPH, and more than 1 of 10 doctor visits is now for a respiratory problem. It was only about 7.6% last week, and it’s also higher than at the same time in the last three Januaries. Covid hospitalizations are also up (but not as bad as the last couple of years), and continuing to rise. The only bit of good news is that RSV cases are declining. Yay. The latest data on the latest Covid vaccines show that they’re about 71% effective in keeping older people (60+) out of hospital. That figure comes out of the Netherlands, but — aside from their odd language — Dutch people are very similar to Americans. Interesting tidbit: This is actually a bit better than the last round of vaccines, which were only about 64% effective against hospitalization. Some hospitals in California, Illinois, Massachusetts, North Carolina, Pennsylvania, Washington and Wisconsin have reinstated face-masking requirements in light of the surge of respiratory illnesses. Which makes so much sense it shouldn’t be news, but here we are. The requirements vary — e.g., some require them for all patients, visitors, and staff, while others only require them in certain situations, like when interacting with patients. As one health official put it, it’s not just about the patients: “What we don’t want is staffing shortages, right? When we saw the omicron wave in 2022, the biggest issues were not only people getting sick, but that we had a lot of frontline health workers, they were out with Covid.” Interesting tidbit: None of those states are among those with the highest level of respiratory virus activity: Paxlovid — when taken quickly — can stop Covid-19 from getting worse, but it has limitations. For one, it can actually increase the risk of “Covid rebound” (we wrote about this in November). Now UC San Francisco researchers found that it doesn’t reduce the risk of long Covid. So Paxlovid is good for one thing: Keeping people from getting really sick or being hospitalized. When the immune system attacks pancreatic beta cells it leads to type 1 diabetes; the injured or dead cells can’t produce insulin. One research path focuses on replacing those dead cells or growing new ones. But what if they weren’t dead dead, but only mostly dead? Could they be brought back to life? Why yes, yes they could, at least according to Aussie researchers. They found a technique for “regenerating damaged pancreatic cells so they can produce insulin and functionally respond to blood glucose levels.” Yep, they brought the beta cells back to life. In fact their technique — which uses two existing EZH2 inhibitors (cancer treatments) — can “reprogram” pancreatic cells so they return to their progenitor state. It’s less like bringing grandpa back to life, and more like making him a kid again. And it worked: After 48 hours of stimulation with the drugs, the reprogrammed cells produced and secreted insulin in response to a physiological glucose challenge. Although they tested this on humans, it’s still in the preclinical stage. They’re hoping it can become the first treatment for type 1 diabetes that actually treats the disease itself rather than just the symptoms. Like most people, you’ve probably laid in bed wondering “Why is pee yellow?” Fun fact: No one knew … till now. A shout out to molecular biologists at the University of Maryland who took the time to figure it out. In short: Red blood cells die, releasing an orange pigment called bilirubin, which ends up in the gut. There it’s broken down into urobilinogen, which is colorless. And then the magic happens: “Urobilinogen then spontaneously degrades into a molecule called urobilin,” which happens to be “buttery yellow*.” They hope this discovery not only makes for fun last items in newsletters, but might open avenues of research into conditions like jaundice. “Our team is excited to be able to explain it,” said the lead researcher, who is undoubtedly a hit at parties. * The most disturbing use of “buttery” we’ve ever heard.Why yellow snow is yellow, resurrecting insulin cells, a vaccine for acne, and more
Acne vax?
STOP, take a moment, and nominate a pharmacy pro for a GPhA award
Want a little AI help writing something?
Respiratory virus updates
Georgia among hardest hit
Covid vax data
Elsewhere: Masks are back
One Paxlovid question answered
Beta cell resurrection
You can sleep easy now
January 06, 2024 ✒ Andrew Kantor
A new open letter from Eli Lilly makes it clear that the company doesn’t want its GLP-1 inhibitors — Mounjaro and Zepbound — to be used for cosmetic purposes: “Lilly does not promote or encourage use of Mounjaro, Zepbound, or any Lilly medicines outside of a medicine’s FDA-approved indication.” (Mounjaro and Zepbound are only approved for treating diabetes and obesity, respectively.) In unrelated news, Eli Lilly has launched a new direct-to-consumer effort, partnering with telehealth company Form Health to offer online diagnosis and prescriptions for diabetes, migraines, and obesity. With LillyDirect Pharmacy Solutions you can enjoy the ease and convenience of getting select Lilly brand medicines delivered directly to you. CVS (the PBM) has removed AbbVie’s Humira from most of its formularies, replacing it with cheaper biosimilars beginning April 1. That is all. As new weight-loss drugs gain popularity, more side effects are coming out. Most people know about the, er, gastrointestinal issues that can occur, as well as “Ozempic face” and even the sulfurous “Ozempic burp.” Now the FDA is looking at some new issues that have arisen in reports: suicidal thoughts, hair loss, and aspiration, “a condition often associated with surgery in which people breathe food, liquids, vomit or saliva into their lungs.” But here’s a twist A new study in Nature Medicine finds that “Weight loss and diabetes drugs Wegovy and Ozempic are not linked to an increase in suicidal thoughts.” So the FDA’s concerns and the actual data may have crossed paths. GPhA member Buffy Gougelmann (left), presents Georgia State Representative Michelle Au with a PharmPAC check this week at Buffy’s store, Premier Compounding Pharmacy in Johns Creek. Representative Au, a member of the House Public Health Committee and a practicing anesthesiologist (aptly pronounced ow), bridges the worlds of medicine and legislation and is a good friend to GPhA. Burn after reading? Here’s a cool member tidbit: If you go to Buffy’s compounding pharmacy, you might get your compounded medication shaken, not stirred. Buffy’s dad, Tucker Gougelmann, is represented by the 78th star in the CIA Book of Honor in Langley. Says Melissa Reybold, GPhA’s vice president of public policy: I’ve known Buffy since the ’90s when we worked together at Costco Pharmacy. One night I saw Buffy on the History Channel being interviewed about her dad on a documentary about CIA agents. Of course, I made her tell me all about it the next day. Her dad’s story would be a great movie. With the Georgia legislative session kicking off next Monday, January 8, stay tuned for Melissa’s full reports here. For quick updates, follow her on Twitter @melissareybold. The FDA has given approval to Florida’s request to try to import drugs from Canada at those lower Canadian prices. “Try” because for one thing there are still US hurdles to jump. Among other things, [Florida] has to specify which drugs it wants to import, verify that they meet FDA’s standards and relabel them. A major stumbling block? Canada isn’t keen on exporting its limited drug supply to the US because their supply is limited, plus there’s a bit of “Solve your own problems, eh?” And one thing we’ve learned is that you don’t want to get on Canadians’ bad side. (Also: US drugmakers are already planning to sue, claiming that Canadian and other imported drugs are somehow not safe.) But, you know, good luck! Obviously different doses of meds have different effects. Duh. It seems, though, that even the placebo effect can be dose dependent. In other words, patients’ reaction to a placebo will vary depending on how big a dose they think they’re getting. In the case of the Mount Sinai researchers who discovered this, they gave e-cigarettes to nicotine addicts, telling them the vapes contained either low-, medium-, or high-strength nicotine. Those e-cigs were actually all the same, but the scientists found that brain scans indicated “that the thalamus, an important binding site for nicotine in the brain, showed a dose-dependent response to the subject’s beliefs about nicotine strength.” And if it works for placebos, maybe it could work for actual medication, too. “The finding that human beliefs about drugs play such a pivotal role suggests that we could potentially enhance patients’ responses to pharmacological treatments by leveraging these beliefs.” It’s that time again — time to play the latest version of everyone’s favorite pharmaceutical game! This time, five of these are new drugs approved by the FDA in 2023, and five are named craters on the moon. Do you know which is which? Check (or get) your answers here.Placebos can have dosages, Lilly’s mixed messaging, our latest quirky drug quiz, and more
Mixed messages
We currently offer select Lilly diabetes, migraine, and obesity medicines.CVS boots Humira
FDA looks at GLP-1 side effects
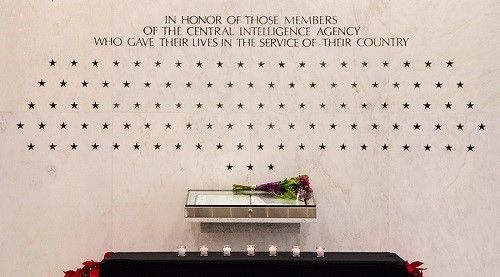
Burn this item after reading

Elsewhere: Florida’s plan (and Canadian hurdles)
The placebo effect has nuance
New drug … or moon crater?
You can play previous versions of the game!
January 04, 2024 ✒ Andrew Kantor
It’s not just pharma companies and pharmacies who have paid big bucks for their roles in pushing opioids onto patients — at least one marketing consultant who helped tell them how to push the drugs is also being hit in the wallet. After paying more than half a billion dollars to various governments for its role, consultant McKinsey & Company has now agreed to pay $78 million more to the health insurers and benefit plans that actually paid for the drugs. (The money will “establish a fund to reimburse third party payors for some or all of their prescription opioid costs” assuming it’s approved by a judge.) Here’s an official GPhA Buzz welcome to Dawn Randolph, who’ll take the reins as the new CEO of the Georgia Pharmacy Association starting February 5. [insert fireworks and marching band here] She’s got a huge list of accomplishments and an awesome résumé, including a ton of work in the healthcare and mental health spaces. She’s got energy and enthusiasm, plus a lot of experience with healthcare policy, and … heck, for all the details read GPhA President Joe Ed Holt’s letter to members. Welcome aboard (almost), Dawn! Under political and financial pressure, all the major insulin manufacturers are now offering insulin with copays of $35 or less, and lowering list prices as well. Don’t give them too much credit, though. They were facing serious bi-partisan wrath for jacking up the price and playing patent games over the years, all for a drug whose discoverers specifically wanted it to remain affordable, even writing in 1922… “The patent would not be used for any other purpose than to prevent the taking out of a patent by other persons. When the details of the method of preparation are published anyone would be free to prepare the extract, but no one could secure a profitable monopoly.” But it took the Inflation Reduction Act a century later, with its threats of costing them hundreds of millions in rebates, to get pharma companies to lower their prices. Trigger warning: This item concerns abortion, but let’s all remain calm. Demand for mifepristone and misoprostol has skyrocketed, especially among women who aren’t pregnant but are “stockpiling” it just in case — we’re talking about almost a 10-fold increase in requests. Sure, AI is coming for all our jobs sooner or later, when we’ll be able to spend our days relaxing in comfort, letting our robot overlords do all the heavy lifting. This Golden Age of Leisure is still a few years away, at least for physicians. At the moment, ChatGPT is hit and miss. WebMD and Doctor Google are now on the sidelines, as people turn to Doctor GPT. Smart people, though, are also seeing a medical professional who’s made out of meat. That means a survey can tell us how well the AI did in its diagnosis. The answer, per a study of about 2,000 adults in the US: This is, of course, self-reported. Still, 84% is pretty darned good, and a lot better than asking on TikTok or Facebook. Pediatricians in New York (publishing in JAMA Pediatrics) found that the latest version of ChatGPT (4.0) “incorrectly diagnosed over 8 in 10 selected pediatric case studies.” The chatbot misdiagnosed 72 of 100 cases selected and delivered too broad a diagnosis to be considered correct for another 11, the researchers wrote. A couple of caveats. First, these were complex cases, not “Jimmy has a cough.” Second — and this bodes well for pediatricians looking forward a life of foot rubs and margaritas — “[O]ver half of the incorrect diagnoses (56.7%) belonged to the same organ system as the correct diagnosis.” So … close, but no cigar. A few years ago, Zika was all over the news — the virus poised to become a mosquito-borne pandemic, causing millions of birth defects and bringing the world to its knees. While Zika ravaged parts of South America, it never became the global crisis, thankfully. Still, the Atlantic (World’s Most Depressing Magazine™) wants you to remember that it could have … and still might. Zika cases dropped precipitously after 2016. And just a few years later, COVID ravaged the planet, giving us all something new to worry about. But that doesn’t mean Zika is gone. The disease is still out there, infecting people every day. There is still no Zika vaccine, and experts say another outbreak is likely before too long.AI’s hits and misses, inexpensive insulin arrives, GPhA’s new CEO, and more
Opioid ripples continue
Welcome, Dawn!

$35 insulin is here
Pill hoarding
Doctor ChatGPT — yes and no
Hit: Good on general diagnoses
Miss: Not great with complex kids’ conditions
Remember Zika?
January 02, 2024 ✒ Andrew Kantor
GSK’s Flovent is gone, and in its place is GSK’s identical (but non-branded) fluticasone. And that’s gonna be a problem. Yes, it’s the same medication; only the box has changed. Yet not every insurer that covered Flovent will cover the version without the fancy box. Insurers get kickbacks from drug makers on branded meds but usually not generics, so they often steer patients toward brand-name drugs. If those insurers aren’t up-to-date on what happened with Flovent, patients could face … let’s call them “coverage hurdles.” Prepare for a lot of conversations. Oh, and why is GSK making the switch? Experts who follow the industry […] point out GSK is making the switch at precisely the time a change in Medicaid rebates could cause the company to have to pay large penalties because of price increases on Flovent over a number of years. […] Or, put another way, it’s the same product without the branding and also without the history of price increases that would leave the medicine vulnerable to such large rebates to Medicaid. Remember, you only have until January 19 to nominate someone for one of GPhA’s 2024 awards! Sure, we’ve all seen the warnings about driving after taking certain types of medication, but when you get down to brass tacks what are the real risks? Researchers at Washington University’s School of Medicine found out the hard way — with a 10-year study of older folks. They tracked their meds, gave them driving tests, and figured out which drugs really presented the most danger. Biggest risks: Antidepressants, sleep aids, and to a lesser extent NSAIDs. Not risky after all: Antihistamines* and anticholinergic meds. Scary stat: “35% received a failing and marginal road test grade at some point.” * The newer, non-drowsy kind So you know about insulin pumps — technology that monitors glucose levels and automatically injects insulin as needed. Pretty cool. But what if you could modify the insulin itself to release depending on a person’s (or at least a minipig’s) glucose levels? That’s just what a team of scientists in China and at UNC have done. In broad strokes, they modified normal insulin with gluconic acid, which in the body reacts with blood and forms a polymer around the insulin molecules. That polymer will then react with blood glucose in such a way that it releases insulin based on glucose levels. So far it’s been tested on minipigs and mice, where it worked as well as standard insulin injections. More animal tests are planned, then they’re moving on to humans. Rather than let mRNA vaccines hog the spotlight, there’s another new kind of vaccine technology that could allow the development of targeted, safe, and cheap vaccines. Where mRNA uses a virus’s messenger RNA to trigger an immune response, these vaccines use protein fragments called epitopes. The good: They can be made quickly and cheapy, and they’re safe. The bad: Different people’s immune systems will react differently to proteins, so an epitope might only trigger an immune response in some people. But now German researchers have found a way to only include the important bits of the protein fragments, so one vaccine can include a whole lot of epitopes and thus work for just about everyone. [The lead researcher] compares the problem with a chef who needs to create a new dish for a large event: “Some guests have allergies, while others do not like certain ingredients, so the chef needs to select ingredients that as many of the guests as possible can eat and will enjoy.” Testing the technology on (of course) a SARS-CoV-2 virus, they think “we would be able to reach — and immunise — more than 98% of the world population.”Self-releasing insulin, inhaler trouble a-comin’, the drugs that affect driving, and more
Impending inhaler kerfuffle
17 days left!
Seniors, driving, and drugs
Automatic insulin
Making a new vaccine tech work
December 30, 2023 ✒ Andrew Kantor
Women should probably avoid taking benzodiazepines while they’re pregnant. Why? Looking at the data for almost 2 million women (and 3 million pregnancies), Taiwanese researchers found that there was a notable increase in the risk of miscarriage — 69% higher than women who didn’t take benzos. The authors wrote, somewhat unnecessarily, “These findings suggest that caution is warranted when using benzodiazepines during early pregnancy.” Indeed. 2024 is almost upon us, and you know what that means: Drug price hikes! Drugmakers including Pfizer, Sanofi and Takeda Pharmaceutical plan to raise prices in the United States on more than 500 drugs. Part of that is because of inflation, although that’s only been about 3%. Part is “because we can.” Part is because they’re going to have to cut prices on insulin. And part is because they know that they’re going to have to negotiate prices on 10 drugs starting in September. (As much as we’re willing to take them to task, even when inflation was high a couple of years ago, pharma companies still kept annual increases to below 10%, and an average of 5% overall. So kudos where they’re due.) But wait! Other companies are lowering prices. GlaxoSmithKline is planning price cuts for on some asthma, herpes, and anti-epileptic drugs, and then there are those insulin price cuts (although that’s kind of because they have to now). Sure, statins and PCSK9 inhibitors are great for lowering LDL cholesterol, but why not take it a step further? That’s what University of New Mexico researchers did, creating a vaccine that gets your body (well, the bodies of mice and monkeys) to attack PCSK9 itself. How, you ask? They “stuck tiny pieces of the PCSK9 protein to the surface of [non-infectious] virus particles” : “So your immune system makes a really strong antibody response against this protein that’s involved in controlling cholesterol levels. In the animals that we vaccinated, we see strong reductions in cholesterol levels — up to 30%.” They’ve actually been working on this for 10 years (!) and are now hoping to start human trials. The goal, said the lead researcher, is to have a cholesterol vaccine available within 10 years at less than $100 per dose. (The one question that wasn’t addressed is whether this is a once-and-done shot, or something that has to be taken regularly. I guess we’ll know in 2034.) Bonus: Yes, it’s a “game-changer”! We wouldn’t ask if the answer wasn’t Yes. The thing about peptides is that they have to be injected — the large molecules tend to fall prey to the acid bath that is the human gut. But Swiss researchers say they’ve developed a cyclic peptide that can be taken orally without being shredded by the digestive system. The first step was, of course, obvious: “synthesizing linear peptides and subjecting them to cyclization so they formed ring-like chemical structures connected by a metabolically stable thioether (carbon-sulfur-carbon) bond.” Naturally. Then came a bunch more science, with the result being “a comprehensive library of 8,448 cyclic peptides” that were small enough to be absorbed by the body before being destroyed. They showed an oral bioavailability of up to 18%, meaning that 18% of the drug entered the bloodstream and had a therapeutic effect when administered orally. While it might not sound particularly impressive, consider that orally administered cyclic peptides generally show a bioavailability of below 2%. So that’s the major step — creating small, tough peptides. Next up will be using the technique to target more diseases. “They’re confident they can develop orally administered cyclic peptides for at least some of them.” So there’s a new antibiotic called omadacycline that’s based on good ol’ tetracycline. But only now did someone think to see how well it would work against Clostridioides difficile, the bacteria that causes a lot of hospital-acquired infections. That someone was a University of Houston pharmacist researcher, and he found something surprising: Not only did omadacycline work a treat against C. diff, but it worked better than the current last-line of defense, vancomycin. Omadacycline was well tolerated by patients, but the key was that it “caused a distinctly different effect on the microbiome than Vancomycin” — it didn’t hurt the beneficial gut microbes nearly as much as vancomycin does, which allowed the good gut bacteria to maintain a resistance to C. diff. (Vancomycin often doesn’t kill enough of the bacteria, so it bounces back.) Says he: “I would hope that this becomes a normal part of the antibiotic drug development process.” A vaccine for LDL, a slick new C. diff fighter, pharma preps its price hikes, and more
Benzos and pregnancy
Here come the price hikes
Cholesterol vaccine?
Could oral peptides be coming?
Omadacycline beats vancomycin for C Diff