July 23, 2024 ✒ Andrew Kantor
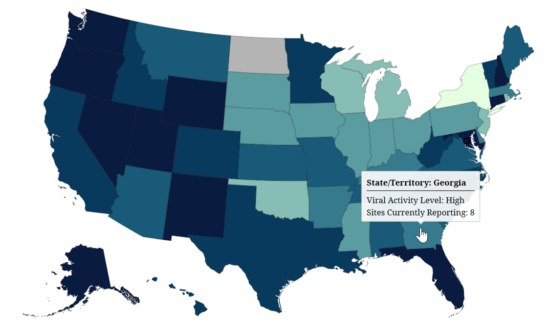
Everyone know how much trouble it is to push through a wall of mucus, and it’s even tougher if you’re a drug molecule. That’s why Spanish researchers developed hydrogen peroxide-powered nano-robots that carry drug molecules though that wall. The peroxide not only propels the ’bots, it also breaks down the mucus barrier long enough for the drugs to slip through “helping them sneak through the mucus defenses like a Trojan horse.” [In the lab] The bots passed through the model’s mucus layer within 15 minutes, without significantly harming the cells underneath. Then they tried it on mouse colons, and it worked there as well, with 28% of the nanobots successfully crossing the mucus barrier. That may not seem like a lot, but 1) it’s the first test of this technique, and B) “that 28% is a 60-fold increase over passive diffusion of particles.” People with Medicare prescription drug coverage will have a new payment option next year, and CMS wants to be sure they’re aware of it. Starting in 2025, Medicare patients can opt to be billed monthly by their plan provider rather than pay at the pharmacy counter. What’s the difference? As part of the Inflation Reduction Act, annual Medicare prescription drug costs will be capped at $2,000 per patient starting in 2025. The new payment option will be good for people who have typically had high out-of-pocket costs — they won’t have to shell out that $2,000 in the first few months of the year; it’ll be a ‘smoother’ payment system for them, as insurers’ monthly charges are also limited by the IRA. Scientists at Oregon Health & Science University and Pitt may have killed 11 monkeys to make their point, but that point was the latest potential universal flu vaccine. In fact, it could be a universal [insert-virus-name-here] vaccine if their technique works outside the lab. Their vax uses a mild herpes virus to carry small pieces of the target virus to activate effector memory T cells. The advantage is that this type of T cell will attack a target based on its internal structure, rather than its outer shell. In other words, the virus can mutate all over the place, but the T cells still recognize it. For an added twist, they tested this not against the current H5N1 virus, but the super-deadly one that caused the 1918 flu pandemic*. And it worked pretty well for a proof of concept: Six of the 11 monkeys exposed to the 1918 flu survived, while all six of the control group died. * Don’t worry, they worked in a “highly secure biosafety level 3 laboratory” so there’s no chance of a virus escaping and causing a pandemic. Good news: The H5N1 vaccine in the US Strategic National Stockpile, which was designed to work against the variant that circulated in the early 2000s, also seems to work against the current clade. It’s not perfect, but it’s good enough to work as a “bridging vaccine” while a new one is developed. It’s been a while since we’ve written about anything controversial, so here you go: A pediatric dermatologist at Penn State is recommending that her peers prescribe emergency contraception along with isotretinoin (aka Accutane). Why? Because isotretinoin presents a serious risk to a fetus, and “Not all teens taking isotretinoin can be trusted to be sexually abstinent.” Making sure those teens have Plan B or something similar available can save a lot of heartache later. (And, of course, levonorgestrel and ulipristal acetate are essentially birth control, not abortifacients, so they avoid that thorny issue.) Q: Can drinking olive oil prevent a hangover by coating the stomach? A: No. Obviously we all worry about cobra bites, especially because the antivenom is expensive and, while it can save your life, probably won’t save the limb that got bit. (Can you say “necrosis”?) We can all rest a little easier thanks to some Aussie researchers. They led a team that made a breakthrough — they found that cobra venom targets a human enzyme that produces heparan and heparin. So they gave the venom another target: good ol’ heparin — yep, the blood thinner. By flooding the bite with heparin, it binds to the venom before it can attack the cells. This means that cheap, plentiful heparin can be added to existing cobra-bite treatments to help prevent the second-worst effect of the bite. (The first being, obviously, death.) Wastewater surveillance shows that SARS-CoV-2 is gaining ground across the country.(Georgia is reporting “High” levels — 7 out of 10 on the CDC’s scale.) The latest data show that almost one percent of all deaths in the country are from Covid-19 — that’s not insignificant. Should acne meds come with birth control? Plus mucus-breaking robots, good flu news, and more
The only mucus-and-nanobot story you need to read today
Medicare drug option coming
The latest universal flu vaccine

Speaking of H5N1…
Birth control with acne meds?
Home treatment Q&A
If it was a snake, it would’ve bit me … but now I have a better anti-venom
Covid update
July 20, 2024 ✒ Andrew Kantor
Rite Aid reported that 2.2 million of its customers’ personal information was stolen in June in a data breach … sorry, a “data security incident.” The theft occurred this year, but the data is a few years old: “This data included purchaser name, address, date of birth, and driver’s license number or other form of government-issued ID presented at the time of a purchase between June 6, 2017, and July 30, 2018.” The company halted ransom negotiations, and the hackers — a group called RansomHub — said they’ll leak the information by the end of the month if they aren’t paid. If you want patients to stick with their treatment for opioid addiction, it’s better for them to use telehealth visits than go to the ER. That’s what University of Buffalo researchers found when they looked at the records of people referred to a local opioid treatment network. Those who came from the ER didn’t stick with the program nearly as well as telemedicine referrals. 65.1% of those referred via a telemedicine call showed up at their first clinic appointment versus 32.3% of those referred via an in-person emergency department visit. Buddy Carter, the Georgia pharmacist — who also happens to be a US congressman — takes it to PBMs in an editorial in the Atlanta Journal-Constitution: “It’s time to bust it up the PBM cartel.” (Bonus: GPhA member Nikki Bryant is featured in the photo.) A new report from the US Agency for Healthcare Research and Quality concludes that about 7% of the US population (18 million people) has had long Covid. That’s based on a survey of 17,000 adults across the county. A different study out of the VA Saint Louis Health Care System found even more detail. Long-Covid rates have been declining to the point that only 3.5% of people vaccinated “during the Omicron era” — i.e., later in the pandemic — have long Covid, compared to 7.8% for unvaccinated patients. (That’s based on data from more than 5 million veterans.) The conclusion: “Vaccines Significantly Reduce the Risk of Long Covid”. Looking at longer-term trends, German researchers found that later variants of the virus were less likely to result in long Covid; “An Omicron infection was substantially less frequently associated with post-Covid-19 condition than earlier virus variants.” Interesting: The more times someone was infected, and the more boosters they had, the lower their risk of long Covid. Conclusion: Expect rates of long Covid to decrease over time. Vermont’s attorney general is suing CVS Caremark and Express Scripts, alleging they “pushed patients toward more expensive drugs even when cheaper ones were available, and pocketed the extra cost through an opaque system of fees*,” which violates Vermont law. Pennsylvania’s governor signed a bill that requires PBMs to reimburse all pharmacies equally and gives the Pennsylvania Insurance Department more oversight over those PBMs. Critically it reads: A PBM registered with the department and conducting business on behalf of a health insurer client in this commonwealth may not: * We’re shocked. Just shocked. A seventh person has been cleared entirely of HIV. (We say “cleared” because we’re talking about the virus being removed from his system, even though the news says “cured.”) In this case, a German man who developed acute myeloid leukemia after an HIV diagnosis needed a stem cell transplant. His treatment team found a donor with a rare mutation (“homozygous delta-32 CCR5”) that provides natural resistance to HIV. The transplant not only treated his cancer but also cleared the HIV from his body — it’s been almost six years now. The detailed science is interesting: The donor was heterozygous with that mutation, meaning they had one copy of the gene … but the treatment still worked. People with heterozygosity for that delta-32 mutation are a lot more common than those with two copies of the gene, meaning there is more hope for a broad treatment.Long Covid is fading, states attack PBMs (and so does Buddy Carter), Rite Aid gets hacked, and more
ICYMI: Rite Aid hacked
Telemed works for opioid treatment
And 53.2% of telemedicine patients were still in treatment at the 30-day mark versus 22.2% of those referred from an emergency department visit.High-five to Buddy
Short takes: Long Covid
The 7 percent
Vaccines cut risk
… and so does repeat infection
Elsewhere: PBMs under fire
(1) reimburse a retail pharmacy an amount less than the amount that the PBM reimburses a PBM-affiliated retail pharmacy located in this commonwealth for providing the same pharmacist services. (Emphasis ours.)Another HIV cure
July 18, 2024 ✒ Andrew Kantor
Senior women who had hormone therapy as part of breast cancer treatment had “a 7% lower risk of developing Alzheimer’s disease and related dementias later in life,” according to a study out of the universities of South Carolina and Pittsburgh. The effect is particularly strong in younger women— ages 65 to 69, and even more so in Black women; those aged 65 to 74 had a whopping 24% reduction in relative risk of developing dementia. (White women in that age group had an 11% reduction.) “The benefits of HMT [hormone therapy] decreased for women aged 75 and older, particularly in those who identified as white*. This suggests that the timing of HMT initiation is crucial and treatment plans should be tailored to a patient’s age.” In fact, once a woman is over 80 the risk of dementia increases with hormone therapy, meaning care needs to be taken to weigh benefits and risks. There are other nuances, including that different types of hormone therapy have different risk profiles, and the mechanism at work isn’t understood. So, as always, more research is needed. * I admit I’m getting old — I didn’t realize you could ‘identify as white.’ Maybe it just means they checked the box marked “White,” but it still sounds odd. Can how you identify affect how a treatment works? By the way, thanks for reading this long footnote. How often you poop is a pretty good indicator of your overall health. There’s a Goldilocks zone between too often and not often enough, according to Institute for Systems Biology researchers. In one sense, frequency reflects health: “Specifically, younger people, women, and those with a lower BMI tended to have less frequent bowel movements.” But too infrequent isn’t good either, as gut microbes will start to ferment proteins rather than fiber, producing toxins. Pooping once or twice a day is that Goldilocks zone (they left that out of the fairy tale) — that’s where the good gut bacteria thrive, which both helps with and indicates good health. Did you know that drug companies get a tax deduction for their direct-to-consumer ads? That’s right — they’re rewarded by the government for running those interminable commercials. That’s because the law considers ad spending to be a deductible business expense just like research and development. “In 2022, the total pharma ad spend topped $8 billion,” meaning that’s $8 billion that wasn’t taxed* and $8 billion worth of ads we all had to watch. Lawmakers have been trying to close that loophole, but fierce lobbying by the pharma industry has meant that there are never enough votes. Still, they’re trying yet again. * Math! The US corporate tax rate is 21%. So that’s almost $1.7 billion per year we could’ve had to spend on, oh, fixing roads, buying school books, cutting taxes on small business…. Healthcare pros don’t think pharma companies are using social media enough … according to a survey by a company called Medfluencers that supplies social media marketing. CBD cream reduced damage from UV-A rays according to a small study out of George Washington University. Big caveat: This didn’t compare CBD creams to other sunscreens — it just showed that CBD creams can help. Santa might not be as jolly as the news reports suggest. It seems that people who are overweight or obese not only tend to have more depressed moods, they’re also more likely to engage in risky behavior. German researchers investigated how metabolic factors, including glucose metabolism, affect both mood and risk-taking. They hypothesized that when glucose metabolism is impaired, so is mood — and then the brain doesn’t get all the signals it needs to control risk-taking. To test this, they put 62 people with severe obesity on an intense 10-week diet and measured their mood and willingness to take risks. After the diet… … there was a significant reduction in the body mass index and the HbA1c level as a marker for glucose metabolism, as well as a significant improvement in mood. In addition, the scientists were able to demonstrate a positive change in behavior, as the weight loss led to risk-avoiding decisions. Choosing supplements can be tough for consumers — not just which ingredients to take, but also which brands they can trust. Because they’re not FDA-regulated, you never know how good Prol-E-Fine™ brand will be. (And if it’s something for long-term health, you might never know.) The closest thing to regulation is USP verification, which is a pretty good indicator that the supplement contains what it says it contains. So now USP has created a product finder at quality-supplements.org/usp_verified_products that lets you look up a supplement or brand to see what’s got the seal. Use it yourself to see what to stock or what to recommend, or point your patients to it to help them shop. q Of course, the lack of a USP seal doesn’t mean a supplement isn’t good, just that it hasn’t been tested (and for some supplements there are no USP Verified products).The right number of poops per day, hormone therapy vs dementia, obesity leads to risk taking, and more
Hormone therapy can reduce dementia risk — sometimes
Our number 2 story
Pharma tax break under fire — again
Short Takes
Just what we need
CBD blocks UV-A
Obesity, mood, and risk taking
USP launches product finder
July 16, 2024 ✒ Andrew Kantor
The US Senate unanimously passed a bill that will limit drugmakers’ ability to create patent thickets — a “complex web of intellectual property that’s hard for generic or biosimilars developers to navigate.” That’s right, unanimously. The US Senate. I know, right? How do they do it? By literally limiting to 20 the number of patents that can be used to defend a product from competition — not more than 10 of which were issued after another company filed to make a generic. (In other words, when they see generic competition coming pharma companies can’t suddenly file for 50 new patents.) We’ve reported a couple of times about Novo Nordisk’s weekly insulin icodec candidate, Awiqli. Not surprisingly, though, the FDA has declined to approve it — at least not without getting more info from the company. (We wrote back in May how an FDA committee recommended against approval because it thought “the weekly insulin icodec’s benefits do not outweigh the risks.” Novo hoped to get around the criticism with better labeling, but that didn’t fly.) About 40% of cancer cases — and almost half of all cancer deaths — are attributable to “modifiable risk factors” like smoking, obesity, smoking, poor diet, smoking, over exposure to the sun, alcohol consumption, and smoking, according to a study by the American Cancer Society. In order of risk: Here’s everything you want to know about the status of oral versions of GLP-1 drugs, courtesy of CNBC. Colorado has reported three new (presumptive) cases of H5N1 bird flu in humans. They were all poultry workers and all had mild symptoms, so nothing to worry about. No sirree. A group of researchers say they’ve found the root cause of lupus: Too much of a particular type of interferon that leads to a “fundamental imbalance in the types of T cells that patients with lupus make.” Looking at the blood of 19 people (i.e., this was a small sample), they found that those with lupus have too much type I interferon. That ends up blocking the aryl hydrocarbon receptor — “which helps regulate the body’s response to bacteria or environmental pollutants.” Because that receptor is blocked, two bad things happen. First, the body can’t make enough wound-healing T cells. Second, it “stimulates the production of T cells involved in creating autoantibodies, which attack healthy cells and are a hallmark of lupus.” There’s that “fundamental imbalance.” The researchers (from Northwestern Medicine and Brigham and Women’s Hospital) think this is going to hold true for all lupus patients, but others aren’t so sure — “Until they study 100 patients prospectively, how are we going to know?” “Adolescent Boys Show Aggression When Masculinity is Threatened”USP supplement finder, Senate tackles pharma patents, lupus’s cause discovered (maybe), and more
Patent pruning shears
Weekly insulin nixed … for now
ICYMI: Ounces of prevention
Short takes
Weight loss in a pill
A little more H5N1
Found: the cause of lupus
Captain Obvious thinks you throw like a girl
July 13, 2024 ✒ Andrew Kantor
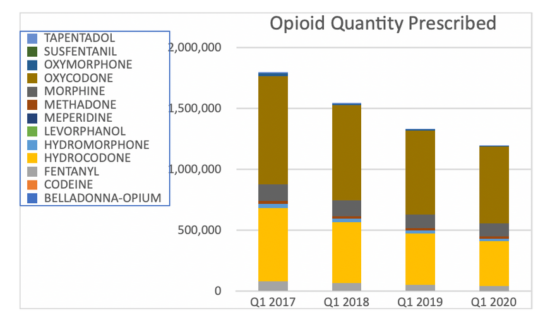
A couple of simple, over-the-counter products can prevent colds, chest infections, and even the flu from taking hold. We won’t bury the lede. The products are Vicks First Defence* gel-based nasal spray or — get this — a simple saline nasal spray. According to British researchers… [B]oth sprays were shown to reduce the overall illness duration participants experienced by around 20 per cent, and resulted in a 20-30 per cent reduction in the days lost of work or normal activity. That’s based on a study of 13,800 adults who either got one of the two sprays, or “an online resource promoting physical activity and stress management.” Tidbits: * Bad news: As you might guess from the misspelling, Vicks First Defence is a British product, but we did find it on Amazon in the US as “Vicks Prèmiere Défense” — at $28 a bottle. Insurers: We’re using AI to automatically deny treatment claims and prior authorizations. Doctors: Fine. We’ve got AI too, and we’re going to use it to draft requests and appeals with a heck of a lot of detail. With the help of ChatGPT, [one doctor] now types in a couple of sentences describing the purpose of the letter and the types of scientific studies he wants referenced, and a draft is produced in seconds. Then he can tell the chatbot to make it four times longer. “If you’re going to put all kinds of barriers up for my patients, then when I fire back, I’m going to make it very time consuming,” he said. They’re actually using a product called Doximity GPT (based on ChatGPT), which is HIPAA-compliant. It uses not only scientific studies to make its case, but also patient medical records and the insurer’s coverage requirements. And it works. Side effects are a big downside to GLP-1 agonists, and nausea is a big one. It’s kind of a “you take the good, you take the bad” situation. But researchers at Philly’s Monell Center found something interesting. It seems that GLP-1 inhibitors affect two types of neurons. Some neurons affect satiety, i.e., feeling full, while some affect nausea. (Want more Latin? The GLP-receptive neurons that affect satiety tend to be in the hindbrain’s nucleus tractus solitarius, while the ones that are more “aversive” are in the area postrema.) All this means, the Monellites figure, that it might be possible to target just one set of neurons, so people felt full without the side effect of nausea. This is all in the early stages, but they’re really into the idea of “separating therapeutic and side effects at the level of neural circuits.” CAR-T cancer treatment works by taking a patient’s own T cells, modifying them to attack cancer, and reintroducing them to do their killing. But there are serious side effects — including death. Enter CAR-NK therapy, which uses natural killer cells instead of T cells. Those don’t need to be taken from the patient’s own body (making them easier to get) and they don’t have CAR-T’s side effects. The downside is that while they work well against leukemia, they can’t work against solid tumors like breast cancer. Yale researchers, though, might have a way around that. They were able to disable some of the CAR-NK cells’ “brakes” — the cellular-checkpoint genes that keep them from becoming too active, notably a gene called CALHM2 that, when knocked out, “made natural killer cells more potent in terms of cancer-killing, more efficient in terms of infiltrating the tumor, and more efficient in producing anti-tumor cytokines.” Now they’re looking at the details of why this works, with a plan to develop a treatment for clinical trial. How well do prescription drug monitoring programs work? In Pennsylvania at least, really, really well. Researchers there looked at a simple metric: opioid prescription rates. They found that prescriptions for opioids dropped 38% from 2017 to 2020; the PDMP took effect January 1, 2017. Side note: The biggest percentage drops were in meperidine (Demerol; down 89%) and fentanyl (down 51%). The big limitation/missed opportunity is that they didn’t look at records before the PDMP was required, to see if opioid prescribing was already decreasing. Here at Buzz we’re big fans of bacteriophages and their potential to treat infections when antibiotics fail. Phages have a few problems, though. They have to be matched to specific bacteria, for one. And to be transported they need to be suspended in liquid and refrigerated or frozen, so labs around the world don’t share as much as they could. Now Canadian researchers have developed a way to help solve those problems — they can store the phages at room temperature in trays that also serve as a testing medium to match phages to bacteria. That means, in principle, that a hospital looking to fight an infection could receive a tray of candidate phages and know within an hour or two if any of them could fight the bacteria they’re facing. It also means they could save those phages in their own library for the future. “If everything moves forward to commercial application as we anticipate, this could revolutionize the way we use phages for different purposes.”$3.00 flu prevention, giving insurers a taste of their own medicine, improving GLP-1s, and more
Easy infection prevention
Sauce for the (insurance) gander

GLP-1 v2?
Natural killers: the sequel
Elsewhere: Penn’s PDMP
Phage breakthrough
July 11, 2024 ✒ Andrew Kantor
On Tuesday, the Federal Trade Commission released a scathing, two-years-in-the-making report about PBMs — a report that concluded, “This vertically integrated and concentrated market structure has allowed PBMs to profit at the expense of patients and independent pharmacists.” Then on Wednesday, the agency followed up, saying it’s going to sue the biggest PBMs (Caremark, Express Scripts, and OptumRx) over their tactics for negotiating prices for drugs including insulin.” In case you missed it, that report didn’t pull punches: [PBMs’ power] can have dire consequences, with nearly 30 percent of Americans surveyed reporting rationing or even skipping doses of their prescribed medicines due to high costs. The interim report also finds that PBMs hold substantial influence over independent pharmacies by imposing unfair, arbitrary, and harmful contractual terms that can impact independent pharmacies’ ability to stay in business and serve their communities. The lawsuit news was breaking at press time, so there isn’t much detail. Still, you’re allowed a big smile knowing that it’s happening. Side note: Georgia’s Buddy Carter weighed in, too: I’m proud that the FTC launched a bipartisan investigation into these shadowy middlemen, and its preliminary findings prove yet again that it’s time to bust up the PBM monopoly. People taking Mounjaro lost more weight than people taking Ozempic, according to a new study from data-analytics company Truveta. Based on the health records of more than 18,000 overweight or obese adults, it found that… Side note: More than three-quarters of GLP-1 drug users quit within two years, according to the latest study of pharmacy claims data. When some Now the FDA has released draft guidance that loosens the leash on those companies when they want to combat misinformation*. Essentially, the companies will be allowed to refute specific claims that are “false, inaccurate, and/or misleading” (but not statements that are someone’s “own experience, opinion, and value judgments”). As long as the companies’ responses target a specific claim, they don’t need to meet all the usual labeling and advertising requirements. The guidance itself is full of boring legalese, but you can skip to the more interesting stuff — the FDA’s examples — on page 13 of the PDF by clicking here. * We used to call it “lies.” Giving losartan to mice with acute myeloid leukemia makes the cancer more sensitive to chemotherapy. The science: Losartan inhibits the AGTR1 receptor in blood cells, which is critical for cell reproduction — and it’s overabundant in leukemia patients. “This disrupted cancer growth, slowing the development of leukemia and led to longer survival.” A lot of people with severe acne (98.3%!) are deficient in omega-3 fatty acids, found German researchers. So … what if you fixed that? It makes a big difference. Over 16 weeks, a Mediterranean diet and algae-derived omega-3 supplements led to sizable reductions in inflammatory and non-inflammatory skin lesions in 60 people with mild to moderate acne. This was a small study, of course, but the Germans hope it will lead to a larger, more comprehensive one. People with autism have different gut microbes* than people without, and that fact has led Chinese researchers to develop an autism test using biomarkers from stool samples. Their test was 82% accurate in identifying autistic children, which could be incredibly useful for earlier diagnosis. (They don’t know if the changed microbiome is the cause of the autism or the result of it — either way, it serves as a useful tool.) * “In all, 51 types of bacteria, 18 viruses, 14 archaea, seven fungi, and a dozen metabolic pathways, were altered in autistic children.” Like Kardashians, Covid-19 still lurks in the shadows. Just when you think it might be gone for good, it reminds you that it’s still out there … and still mutating. Right now it seems that the new FLiRT variants (KP.2 and KP.3 mostly) are surging. [E]mergency room visits due to Covid-19 from June 16 through June 22 […] were up 23.3% from the previous week. Also, Covid-19-related hospitalizations during the week of June 9 through 15 were 13.3% higher than they were than the week before. “Surging” might be a strong word, as the numbers are still low. But keep in mind that Covid surveillance has pretty much shut down, so there’s probably a lot circulating that health officials don’t know of. “I’ve got a cough, so I’ll stay home today.”FTC suing PBMs, pharma can fight online lies, omega-3s vs acne, and more
After report, FTC to sue PBMs
Mounjaro beats Ozempic
Pharma allowed to combat online misinformation
chucklehead influencer on TikTok says something stupid about a drug (“Adderall makes your earlobes shrink!”) drug companies have trouble refuting it because of the regulations about what they can say online.Short takes
Losartan boosts chemo (in mice)
Fighting acne with omega-3s
A simple autism test?
Covid is still FLiRTing
July 09, 2024 ✒ Andrew Kantor
Yet more info shows that STDs are rising fast among seniors — we’re talking a 24% jump during the pandemic, which makes us wonder if grandma misunderstood what “lockdown” meant. One of the issues is that symptoms of some STDs can look a lot like other age-related conditions, which means they can easily be misdiagnosed; no one expects Aunt Shirley to have gonorrhea. Speaking of which, the number of men with gonorrhea jumped higher than the number of women with it, but the reverse was true for syphilis. Go figure. Germany is reporting the first case of the H7N5 bird flu. Not just the first case in Germany — the first case ever. (Well, since 2005 when this stuff started being tracked.) “The outbreak killed 6,000 out of a flock of 90,879 birds in the town of Bad Bentheim in Lower Saxony.” But no worries — it hasn’t jumped to other animals. What could go wrong? What was that saying about ‘Doing the same thing over and over and expecting different results?” Yet another pharma company — this time Boehringer Ingelheim — challenged Medicare’s authority to negotiate drug prices. And yet another pharma company lost that challenge. BI argued (just like the others) that it was essentially forced to participate in Medicare/-caid because it wouldn’t make as much money if it didn’t participate. Thus it should be allowed to charge taxpayers whatever it wants for its drugs, and being forced to negotiate violated its First Amendment rights. Once again (the 5th time), a federal judge disagreed. “[C]ompanies remain free to withdraw from Medicare or Medicaid and can decide not to participate in the drug price negotiations.” Some tampons — even big name-brand ones — have some nasty stuff in them, including lead and arsenic. That’s what UC Berkeley researchers found after testing 30 tampons from 14 brands in the US, the UK, and Greece. The analysis looked for concentrations of arsenic, barium, calcium, cadmium, cobalt, chromium, copper, iron, manganese, mercury, nickel, lead, selenium, strontium, vanadium and zinc. All 16 metals were detected in one product. What they don’t know is whether those metals leech out of the tampons or if they’re absorbed by the body (“Further studies are necessary”). As to where the metals come from, they might have originated in the soil the cotton grew in. Canadian researchers used CMS’s Open Payments database to see just how the pharmaceutical industry was targeting prescribers. Some highlights: It’s a smart investment in dry chicken and iced tea: Receipt of industry payments, including low-value payments for food and beverage, is often associated with physicians prescribing higher quantities of promoted and higher cost drugs, such as brand name drugs over generics. Inflammation caused by the flu can add complications to pregnancy, notably reducing blood flow to the placenta. But there might be a simple solution: low-dose aspirin. It’s already used against inflammation from preeclampsia, so Aussie researchers wondered if it would also help with other causes. So they tested the idea on mice, and yep “mice treated daily with low-dose aspirin had less inflammation and improved fetal development and offspring survival.”Pharma suit fails again, questionable tampon ‘ingredients,’ seniors and safe sex, and more
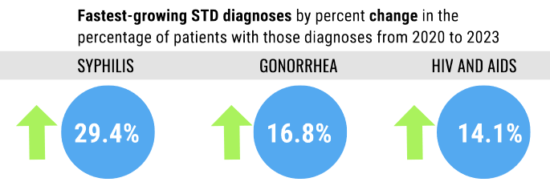
Senior STDs jumped
The next bird flu
Once more with … failure
Metal in tampons?
Fun facts about pharma-sponsored dinners
Flu, pregnancy, and aspirin
July 06, 2024 ✒ Andrew Kantor
Out of the blue comes the first generic GLP-1 drug. It’s liraglutide, a generic form of Teva’s Victoza, and as it’s actually made by Teva it is Victoza but in a different box. Teva is reportedly planning to charge $470 for a two-pack of pens or $700 for a three-pack (a $5 discount!), which is 13.6% lower than the brand-name price. Victoza is officially approved only for diabetes, but we all know how much of a difference that’ll make. Side note: It’s a daily injection rather than a weekly one, which patients won’t be thrilled about. A new study out of Case Western Reserve University found that people taking GLP-1 agonists “have a lower chance of developing 10 types of obesity-related cancers than those taking insulin and other diabetes drugs.” Interestingly, they weren’t funded by the drug makers. If you’re sleep deprived, you can start to forget things; sleep deprivation affects the hippocampus. There might be hope, though. Dutch researchers have found that the drug roflumilast (Daxas or Daliresp to its friends) can help restore mice’s social memories — “Have I met him before?” — that were lost thanks to lack of sleep. And lost spatial memory — “Was that chair always there?” — can be restored with vardenafil, aka Levitra. Why does this work? They don’t know. As usual, more research is needed. It’s not surprising when you think about it: In areas where more people were vaccinated against Covid-19, kids had fewer asthma symptoms during the pandemic. Asthma rates during the pandemic dropped all over because of school closures and social distancing, but researchers at Nemours Children’s Health found that high-vax states saw an asthma reduction three times higher than lower-vax states. They found that for each 10-percentage-point increase in Covid vaccination coverage, there was an average 0.36 percentage point decrease in childhood asthma symptoms. If you have mice who have gained weight after menopause, there might be a way to help them: a sauna. UMass-Amherst researchers found that “daily time in a warm environment such as a sauna might help older adults, especially women, combat age-related obesity and insulin resistance.” (To simulate menopause, they removed the mice’s ovaries. To simulate being American, “the mice received a Western diet that contained 45% calories from fat.”) Compared to the mice not receiving the treatment, those that underwent heat therapy showed significant improvements in insulin sensitivity and insulin signaling as well as reduced fat accumulation in key areas such as the liver and in brown fat. Of course that’s not nearly science-y enough, so they looked into what was going on at the molecular level. Heat, it seems, activates a protein called TRPV1, which… …kicks off a process known as futile calcium cycling where the body uses up energy (in the form of ATP) to pump calcium ions across cell membranes. This process helps increase the amount of energy the body burns. Questions: Will that translate to humans? And if so, can it be made into a pill? When someone is overdosing on opioids, naloxone works wonders — but sometimes it takes several injections (or sprays) to be effective. When fentanyl is involved it can be even more. Now, though, a group of American researchers say they’ve got a way (a proof of concept, anyway) to boost naloxone’s effectiveness. It’s a compound called, memorably, 368, and it works by sorta-kinda plugging opioid receptors while they have naloxone in them, making that naloxone last longer. Tests found 368 made naloxone 7.6 times more effective at inhibiting the activation of the opioid receptor, in part due to naloxone remaining in the binding pocket at least 10 times as long as when it was given on its own. Bad news: It could take 10-15 years to turn the finding into an actual drug.Drugs restore memories, generic GLP-1 debuts, saunas for menopause, and more
First generic GLP-1
Speaking of GLP-1 drugs….
Bringing back memories
Covid-asthma connection
Mice, menopause, and saunas

Potential Narcan booster
July 04, 2024 ✒ Andrew Kantor
Semaglutide use has been linked with a higher risk of an eye condition that can cause blindness — nonarteritic anterior ischemic optic neuropathy or NAION. In other words, the Mass Eye and Ear researchers who did the study found that … After taking patients’ other risk factors for the condition into account, such as high blood pressure and obstructive sleep apnea, use of semaglutide was associated with a more than four times higher risk of NAION in those receiving it for diabetes and a more than seven times higher risk in patients taking it for obesity. Some antidepressants can lead to more weight gain than others, and some can even help lose weight. But researchers at the Harvard Pilgrim Health Care Institute wanted to get the details, so they turned to the health records of more than 180,000 adults who were new users of antidepressants. They compared the subjects’ weight after six months, one year, and two years and cross-referenced with the drugs they were using: bupropion, citalopram, duloxetine, escitalopram, fluoxetine, paroxetine, sertraline, or venlafaxine. They found that patients taking escitalopram (Lexapro), paroxetine (Paxil), or duloxetine (Cymbalta), “had a higher risk, 10 to 15 percent, of gaining a clinically significant amount of weight” compared to people on sertraline (Zoloft). And those on bupropion (Wellbutrin) were less likely to put on the extra pounds. (The link above goes to the press release; here’s a news article on the story.) A British study found that about 40% of patients who’ve used antidepressants more than a year can stop taking them without major side effects — just being in touch with GPs or even online therapists was enough for them to get off and stay off the drugs. The FDA has approved Lilly’s Kisunla, aka donanemab, to slow the progression of Alzheimer’s. It’s another drug that targets amyloid plaques, and another drug that has a limited but notable effect — it can delay the onset of cognitive decline by about seven months. Lilly has set the price at $32,000 for a year, but unlike the other anti-plaque drug that’s been approved, Eisai’s Leqembi, patients can stop taking Kisunla once plaque levels decline. Like Leqembi, though, there’s a risk of brain swelling and bleeding. A Lyme vaccine is in late-stage trials (yay!), but Northeastern researchers think they can do one better. They’re working on a vaccine against ticks, period — not just Lyme, but other tick-borne diseases like Rocky Mountain Spotted Fever. The idea is simple, actually. People can naturally develop resistance to ticks if they get bitten enough. In a win for simplicity, it’s called acquired tick resistance. “[H]ost animals that ticks have fed on ‘develop an immune reaction to the saliva and possibly to other tick parts’,” the lead researcher explained. Kind of like the little brother who keeps poking you. At some point he’s gonna get smacked upside the head. The Northeasterners now want to see if they can use this fact to create a vaccine that would have the same effect — perhaps using tick saliva — without requiring anyone to get bitten over and over. “If the tick cannot feed and falls off prematurely, then the pathogens don’t make it into the vaccinated host either.” How well do statins work in people 75 or older? Pretty darned well according to a joint US-Hong Kong research team that looked at the medical records of more than 80,000 older individuals over 11 years. The robust evidence demonstrated that continuous statin therapy resulted in a substantial relative risk reduction in cardiovascular diseases (CVDs) of 21% for those aged 75–84 and 35% for those aged 85 or above, without any heightened safety concerns. Weight gain with (some) antidepressants, a vaccine against ticks, vision loss with Ozempic, and more
Vision loss with semaglutide?
Antidepressants and weight gain
Short Takes
Good news … for 40%
New Alzheimer’s drug approved
Fun fact about ticks
Statins work for older folks
July 02, 2024 ✒ Andrew Kantor
The Atlanta Journal-Constitution has a front-page story about how independent pharmacies are — to put it mildly — unhappy with Governor Brian Kemp’s veto of Senate Bill 198, which would have required independent pharmacies to be reimbursed by the State Health Benefits Plan at the same rate as chain pharmacies. The bill passed the Georgia House and Senate almost unanimously, but the governor said it would be too expensive to pay small pharmacies as much as the chains get. Meanwhile, at least three independent pharmacies in the state have gone out of business so far this year, as have many more in the last few years. The State Health Benefits Plan is managed by CVS Caremark. Kemp said earlier that the 2025 state budget “includes one-time funding for a dispensing fee of $3 per prescription for independent pharmacists.” Some people with compromised immune systems can’t get the measles vaccine. This wasn’t too big a deal, as we’ve virtually eliminated measles in the country. Until, that is, the anti-vax movement, which has brought measles back and put those people at risk. (Herd immunity requires 95% of people to be immune, and in the US that number is down to 85% for measles.) Now, though, there might be a breakthrough. Researchers from Columbia University and the La Jolla Institute for Immunology have found different proteins (“fusion proteins”) that trigger an immune response to measles, but that don’t need to be delivered via a weakened version of the virus — that’s what makes the standard MMR vaccine dangerous for the immunocompromised. They’re now looking at stabilizing those fusion proteins into a vaccine Cisplatin is no longer in shortage. The 2022 Modernization of Cosmetics Regulation Act begins to take effect this week. It “bestowed on authorities the power to recall a product and to make companies report serious adverse events, from hair loss to birth defects.” The effect will most likely be seen in fewer claims being made for products (no, that cream won’t make you look like a 16-year-old), and manufacturers looking more closely at the ingredients they’re using — and possibly reformulating. People with chronic migraine sometimes overuse pain drugs, looking for a way to relieve the pain. The problem (besides the obvious) is that it can lead to rebound headaches. It turns out that the migraine drug atogepant might help. A British study found that even when atogepant doesn’t prevent every migraine, by reducing the amount of meds someone needs, it can reduce rebound headaches. Fewer rebound headaches then mean less medication, leading to a positive feedback loop and less overuse. [F]or participants with medication overuse, those taking atogepant twice daily had an average of three fewer migraine days a month and three fewer headache days when compared to those taking placebo. Even better, atogepant cut the number of people overusing medication by 62% (if they took it twice daily) or 52% (if they took it once a day). When we talk about drug prices in the US, it gets confusing: There’s the list price, the (secret) price PBMs actually pay, and what patients actually shell out either by paying cash or via their co-pay. GoodRx is now tracking the latter, which is what most people are concerned about (aside from business owners, who are looking at premiums). What it’s found in its Prescription Cost Tracker is that…. At least it’s better in the US than in the rest of the world, where government bureaucrats decide what medications they’ll cover — here we’ve got the PBMs looking out for us*. * Sarcasm? You decide. In the next step toward crafting our forthcoming robot overlords, scientists have developed a lifelike skin to cover robots. It’s made of living human skin cells. Not creepy enough? They made it smile. Veto angers pharmacists, new kind of measles vax, FDA takes on cosmetics, and more
Indy pharmacies ‘shaken’ by governor’s veto
Protection from the unvaccinated
A bit of good news for cancer patients
The FDA will be regulating cosmetics ingredients
Preventing rebound migraines
Tracking OOP drug prices
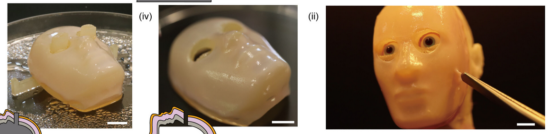
A creepy little non-pharma science story