Board considers allowing pharmacies to dispense cannabis products
The Georgia Board of Pharmacy is considering allowing medical cannabis products to be sold at independent pharmacies.
The logic is that there are only two dispensaries — one each in Macon and Marietta — and four more might open in places including Newnan and Pooler. That leaves a lot of the state uncovered and only half of the 12 allowed dispensary licenses in use. Independent pharmacies could fill the gap.
Next stop: The June 14 Board of Pharmacy meeting.
Stop the poppers
The FDA would really like it if you didn’t use or sell “poppers”. They’re packaged like energy drinks, sold as solvents or other household chemicals (wink, wink), might work like vasodilators, and they can really — to use the scientific phrase — mess you up.
“These chemicals can be caustic and damage the skin or other tissues they come in contact with, cause difficulty breathing, extreme drops in blood pressure, decreases in blood oxygen levels, seizures, heart arrhythmia, coma, and death. Do not ingest or inhale under any circumstances.”
They might have names like “Super Rush” and “Jungle Juice,” but they’re more drain cleaner than drug.

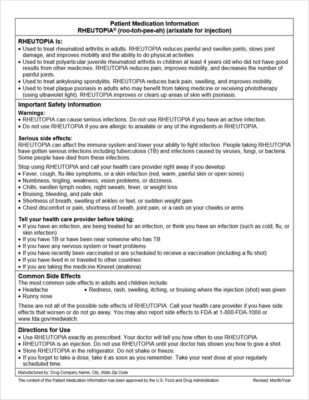
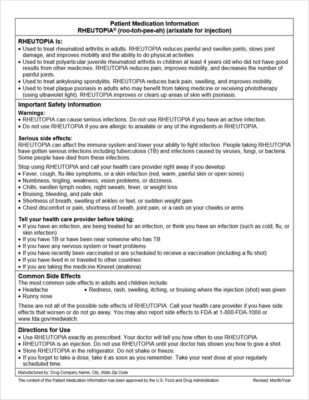
Simpler info sheets
The patient-information sheets that come with medications are full of information, but they’re not particularly useful to the people who are supposed to make sense of them. So the FDA is proposing a change: new, easier-to-read guides for patients.
“Studies have found that the current system for written information for prescription drugs and certain biological products can be confusing, conflicting, incomplete, or repetitive,” the agency wrote. (Apparently they needed studies to figure this out.)
The new proposal, called Patient Medication Information sheets, would be single-page documents (presumably not in 6-point type) that would include the drug name, a “Concise summary of the indications and uses” and safety information, the most common side effects, and of course directions for use.
They would replace and simplify the two types of prescription drug information currently in use. Well, mostly. It’s not as if the sheets won’t be overwhelming to a lot of folks — just a bit less overwhelming. (Click to expandify.)
Diabetics at risk
If you have patients with type 2 diabetes, take note: A new study out of Johns Hopkins finds that 1 in 3 of them are likely to have biomarkers for cardiovascular disease without having any signs of heart trouble … yet.
“What we are seeing is that many people with Type 2 diabetes who have not had a heart attack or a history of cardiovascular disease are at high risk for cardiovascular complications.”
Better to deal with that now than later, doncha think?
A faster way to classify narcotics
New synthetic drugs, especially cannabinoids, hit the streets faster than regulations can keep up: Restrict 1,3,4-polydichloric euthimal and someone develops 1,3,5-polydichloric euthimal. You can’t just ban “any related substance” without causing a huge headache.
It’s not just a US problem — Europe is grappling with it too. Now, though, a group of Swedish biomed researchers have developed what they say is a standard method to classify new drugs that’s all about measuring the chemical’s effect on the appropriate cell receptor.
It’s actually pretty simple: They expose cultured cells that have (for example) the cannabinoid receptor on their surfaces, then measure how much the receptor is activated, if at all. That measurement tells them immediately whether the drug is akin to a street drug, how strong its effect is, and whether it’s dangerous. Then, in theory, public health officials could ban, say, “Any drug that has this much of an effect on this receptor.”
The researchers have further developed the method so as to also measure effects on the cellular systems affected by substances similar to for example amphetamine, cocaine, heroin, morphine and fentanyl.
Going postbiotic
The benefits of pre- and probiotics aren’t just in the bacteria themselves, they’re in what those bacteria produce: metabolites.
It’s those metabolites, Aussie researchers explain, “like short-chain fatty acids, certain vitamins (Vitamin B and K), amino acids and antimicrobial peptides” that give the -biotics their good reputation.
So why not skip the pre- and pro- and go right to the postbiotics?
[T]he beauty of postbiotics is they can provide these benefits even without any side effects that probiotics and prebiotics may have. For example, some people might experience discomfort because of a temporary increase in gas and bloating after intake of probiotics and prebiotics.
And as a bonus it seems that there’s a feedback loop — having those good postbiotics can help the growth of the bacteria that produce them. The benefits are widespread, too, from boosting the immune system to helping prevent cancer, and even to improving mental health.
The big downside: Postbiotics have only been played with in the lab, so “there will be a lot more to discover in the coming years.”
Now we know who to blame
“40% of US foodborne restaurant outbreaks traced to sick workers”

This item has very little useful information about ketamine and migraines
It seems that, based on a retrospective look at a clinical trial, ketamine nasal spray might help relieve chronic migraines.
Ah, but the caveats: The study considered was small. Eighty percent of the participants were female and most were white, with an average age of 44. The women also took other meds. Still, among that narrow cohort it seemed to work:
Overall, the patients said they used the nasal spray six times over an average of 10 days a month. Nearly half (49%) said the spray was “very effective,” while 39.5% found it “somewhat effective.” More than one-third (35.5%) said their quality of life was “much better.”
But there are downsides, most notably the chance for dependency. And even the researchers who did the study said it didn’t necessarily show ketamine was a useful treatment.
Short (non-pharma) Takes
When no one gives up
That social media is bad for health — mental and even physical — is kind of obvious at this point. But what about quitting it? How much will that improve your health? Researchers don’t know because “Almost nobody can log off long enough to find out.”
A night to remember
Gentlemen between about 56 and 68: If you’re not satisfied with your, um, personal life, you might want to write it down: “Low sexual satisfaction linked to memory decline later in life, study finds.”