July 06, 2023 ✒ Andrew Kantor
Chances are you’ve got female patients in the 12–21 range. Fun fact: There’s a good chance they’re iron deficient. A new multi-university study found that the CDC-recommendation of screening non-pregnant women every five to 10 years for anemia isn’t nearly enough. Anemia takes years of iron deficiency to build up. What they found is that among women who had hit puberty, “27.1% had iron deficiency when using the 25-μg/L ferritin level threshold,” but when you add in the younger ones it reaches 38.6% deficient. “Given the high prevalence of iron deficiency,” the authors wrote, “…current screening guidance may miss many individuals with iron deficiency.” Something bugging you about Georgia’s pharmacy’s legal landscape? Should something be outlawed or in-lawed? That’s what GPhA is all about! Each year, the GPhA Legislative Committee takes ideas submitted by members about what laws need to be enacted or changed, and that’s where our legislative priorities come from. It’s that time of year again. If there’s a law or policy issue you want to see changed — something that will improve patient care or the practice of pharmacy — tell us about it! E-mail a brief explanation of the issue to our VP of public policy, Melissa Reybold, at mreybold@gpha.org. Yes, it’s that simple — just give as much detail as you can about how it affects you. Oh, and do it by the deadline of Friday, July 21 at 5:00 pm. Time to change the world … or at least the state! Well look at the time! It’s time to take another look at whether legalizing cannabis has an effect on pain-med prescriptions. And the latest answer is [insert drum roll] … nope, legal pot (medical or recreational) doesn’t affect painkiller prescriptions for patients with chronic pain. See you in a few months for the next study! Did you happen to catch the story about the WHO deeming aspartame a carcinogen? That’s actually not what the announcement said at all, but that didn’t stop it from being reported that way. In fact, all the WHO did was move aspartame from unclassified to possibly carcinogenic — a catch-all category that just means the data don’t rule out the sweetener being unsafe. (The other two categories are probably carcinogenic and carcinogenic.) As one journalist put it, “It’s a bloated category, essentially one big epidemiological shruggie.” So before you think about giving up that sweet, sweet Diet Dr Pepper, check out “Being Alive Is Bad for Your Health,” which gives more detail about what the WHO really said. Whether you’re working or studying, Aussie researchers have proven that the anecdotal life hack of taking a five-minute break really does reset your brain. There is no need for a walk along a river, or a lengthy video of bamboo forests swaying in the wind (although that could be nice). A five-minute total break will do the trick. The important thing is that it has to be a real break — “unstructured,” as they put it. No computer or phone, no switching to another task. Turn your brain off. “[D]o some breathing or just sit quietly to rest your brain from the task.” The result will be better concentration and problem-solving when you get back on task. I won’t say anything if you don’t, but for patients with diabetes, getting a “prescription” for fresh produce — i.e., “which would provide free or discounted fruits and vegetables to eligible Americans living with diabetes” could save the current cohort of diabetic Americans $40 billion in medical bills by preventing cardiovascular problems. That’s the result of a Tufts University data analysis. But fruit and veg ain’t cheap — it would cost a bit more to pay for it (and administering a program). The net price would be about $18,000 per “quality-adjusted life year”: This is on par with other “best buys” in health care, like blood pressure screening and control, cholesterols screening and control, and cancer screening. (In comparison, the new GLP-1 weight loss medications cost about $200,000 per quality-adjusted life year gained). The headline reads “Being overweight may not be associated with early death,” but the details aren’t nearly as interesting. So no, you can’t just rush out to hit the Oreo aisle. What the Rutgers study found was that a high body-mass index by itself doesn’t mean you’re likely to die earlier. It’s the various problems with being overweight — diabetes, heart issues, etc. — that’ll do you in. (And there’s also the issue of BMI no longer considered a good indicator of obesity, raising the question of why they used it in the first place.) As one reader of the study put it, “The main hazard of overweight and moderate obesity is a three times greater risk of developing diabetes which contributes to cardiovascular disease, renal failure and blindness.” Five minutes for your brain, obesity-study confusion, aspartame reality check, and more
Girls need iron
It’s that time: What oughta be a law?
Cannabis laws and painkillers
Aspartame: What’s the real deal?
Take 5 for your brain

An ounce of (non-pharma) prevention
Why you need to read past the headline
July 04, 2023 ✒ Andrew Kantor
Georgia (and Florida) is the epicenter of a national outbreak of cyclosporiasis, probably from raw imported broccoli and other veggies. The worst part is that the main symptom is explosive diarrhea. It can take a week or two for the symptoms to appear (they also include “nausea, a loss of appetite, cramping, bloating, increased gas, and fatigue”). The treatment, luckily, is simple: trimethoprim/sulfamethoxazole, aka Cotrim. If a patient is allergic to sulfa drugs … well, there’s nothing to do but wait it out. [T]he CDC recommends that the “best way to prevent cyclosporiasis” is “avoiding food or water that may have been contaminated with feces.” That is important news if all along you’ve been seeking food or water contaminated with feces. More than 1.5 million Americans have been “disenrolled” from Medicaid since the end of June. The worst part: 71% of them were disenrolled for “procedural reasons,” not because they weren’t eligible. (Of those, 35% were children.) Procedural disenrollments are cases where people are disenrolled because they did not complete the renewal process and can occur when the state has outdated contact information or because the enrollee does not understand or otherwise does not complete renewal packets within a specific timeframe. In response to so many people losing coverage, the Biden administration has given states more options to slow the disenrollment flow, including allowing states an extra month “to conduct more targeted outreach to individuals” and — notably for Buzz readers — “allowing pharmacies and community-based organizations to reinstate coverage for some individuals disenrolled for procedural reasons.” Michigan is taking advantage of that offer and will pause disenrollments until the end of July while it works to help its citizens complete the paperwork. South Dakota became the 40th state to expand Medicaid under the Affordable Care Act; it will cover people earning $20,120 per year for an individual or $41,400 for a family of four. Australia has become the first country to legalize psychedelics to treat some mental health conditions: “MDMA to those suffering post-traumatic stress disorder and magic mushrooms for some types of depression.” It’s by prescription only and “Use of the psychedelics would be carefully monitored and not a case of ‘take a pill and go away’.” Bonus: Includes the phrase “game changer” twice. A blood condition called clonal hematopoiesis of indeterminate potential (CHIP) has an odd association: People who have it are significantly less likely to develop Alzheimer’s. Unfortunately, they’re also much more likely to develop blood cancers and heart conditions. CHIP is caused by a mutation in the bone marrow’s blood-producing cells. It results in mutant blood cells that outcompete normal ones. The twist is that some of those cells slip into the brain and can replace the brain’s immune cells — the microglia. Those are supposed to do trash pickup in the brain. So … could these mutant cells be boosting the microglia so they fight Alzheimer’s? You know the mantra: More research is needed. Sure, Americans want to lose weight, and we love an easy way to solve a problem. But when it comes to all those new weight-loss drugs, a poll shows there’s a limit to how much people are actually willing to spend. Ozempic, Mounjaro, Wegovy — they all cost big bucks, and many insurers aren’t covering them. With a list price of $900 to $1,600 per month, even with insurance that’s a lot of co-pay. It’s also co-pay that keeps on taking, because you can’t just use these drugs to hit a goal; you have to take them forever. “Can you really ‘address’ annoying eye floaters with a supplement?” No. Don’t be. They’ll do just fine.Explosive GI infections, Aussies legalize psychedelics, Medicaid changes coming, and more
The worst kind of outbreak
Medicaid news
Disenrollment troubles
Elsewhere
A trip down under
Blood mutation-Alzheimer’s connection
The cost of weight loss
Short Takes
Saving you a click
Worried about health insurance companies’ profits?
July 01, 2023 ✒ Andrew Kantor
Semaglutide: “I can help people lose 15% of their body weight!” Tirzepatide: “Pshaw! I can help them lose 21% of their body weight!” Retatrutide: “Hold my beer.” After 48 weeks, Eli Lilly’s new, still-in-phase-2-testing drug, retatrutide, led to an average weight loss of more than 24% — we’re talking 57.8 pounds (14,797 drams). How? By not just targeting GLP-1 (like semaglutide), and not just GLP-1 and GIP (like tirzepatide), but by targeting those two plus activating of glucagon receptors, which help regulate blood sugar. Next up: Four different phase-3 studies. In what’s not entirely a surprise, it turns out that higher doses of semaglutide do a better job helping with blood sugar and weight loss. [O]nce-daily oral semaglutide taken at 25 milligrams and 50 mg did a better job in lowering blood sugar levels and promoting weight loss than the lowest dose of 14 mg. Lots of people lose hair where they want to keep it, but sometimes you get hair where you don’t want it. Say, for example, on a hairy mole. It takes a special kind of person to look at such a hairy mole and think, “I wonder if the secret to treating hair loss lies within?” And yet that’s just what some UC Irvine researchers did … for a decade. All because they realized that some of those ugly moles — called nevi — can “induce luxurious hair growth.” Over some 10 years of work, the researchers identified a chemical released by a mole’s pigmented cells that “potently stimulates hair follicle stem cells for robust hair growth.” That molecule is osteopontin. […] The secreted osteopontin interacts with a molecule on the stem cells called CD44, apparently flipping the hair-growing switch to “gonzo.” Tests continue with a hope of creating, say, a biannual injection that would cause hair to pop out where it’s wanted — but sans the mole part. Bonus: Includes the phrase “game-changer.” You wouldn’t think there could be “An Unexpected Doorway into the Ear,” but here we are. And the good thing about this particular door is that it can be used (Rochester University researchers found) to “deliver a gene therapy that repairs inner ear hair cells [and] restore hearing in deaf mice.” Using gene therapy this way isn’t a new idea, but the problem was reaching the cochlea without surgery. But now with the cochlear aqueduct, they were able to do that, injecting a virus that carried a gene therapy into the inner ear. That therapy was able to fix the ear’s hair cells and restore hearing … to mice, at least. The EU has made a deal with Pfizer (and others) to reserve vaccine-making capacity for the next pandemic — whatever that pandemic might be. “The agreement covers mRNA, vector-based and protein-based vaccines [and] ensures that companies are ready to respond to a crisis by keeping their facilities up to date and monitoring their supply chains, ‘including stockpiling where necessary’.” mRNA vaccines work great, as we’ve learned, and are being used to treat other diseases, notably cancer. But they could be better. mRNA vaccines are very good at getting muscle cells to generate an antibody response, but what you really want is a longer-lasting T cell response. To do that you need to activate dendric cells — the ones that teach T cells to attack … well, whatever you want attacked. Muscles are low on those dendric cells, but the spleen has plenty, and now Johns Hopkins researchers have developed an intricate little nanoparticle wrapper for mRNA that that can find its way to the spleen where it “was taken up by primary dendritic cells at levels about fifty-fold higher than mRNA by itself.” This means they may have found a way to make mRNA vaccines more effective by creating not just antibodies, but (in this case) “an army of T-cells that can recognize cancer-linked antigen.” We can cure hepatitis C, and treating it is expensive. So why haven’t we ended it? The cost (at least in the US) is a big part, but it’s not the only issue. Read on, MacDuff. Israeli researchers found that adding a “natural” molecule called 3,3´-Diindolylmethane (bisindole to its friends) to toothpaste will kill the biofilms formed by bacteria that cause plaque and cavities, reducing it by 90%. “The molecule, which was found to have low toxicity, could be added to toothpastes and mouthwashes to greatly improve dental hygiene.” Not enough for you? Bisindole also has anti-cancer properties. No matter who wins the 2024 presidential election, pharmaceutical companies face and uphill battle. “There is no leading candidate that’s a friend of the pharmaceutical industry at this point. Not DeSantis, not Trump, not Biden.” Low-dose colchicine (LoDoCo, seriously) — the gout med — just got FDA approval “to be used in low dose to prevent cardiovascular events in patients with proven coronary disease.”Hairy mole goodness, hidden ear passages, yet another weight-loss drug, and more
The next next weight-loss drug
Speaking of weight-loss drugs…
We didn’t include a photo. You’re welcome.
A new path for gene therapy
Europe prepares for the next one
A better way to deliver mRNA
The Long Read: Why is hep C still a thing?
Short Takes
Toothpaste as bacteria killer
Dark future for PhRMA
Mo fo’ LoDoCo
June 30, 2023 ✒ Andrew Kantor
When OTC analgesics don’t work for acute back pain, low-dose, short-duration opioids are often the next step. But Aussie researchers found that they don’t work any better than placebos (and, of course, you kinda want to avoid opioids in general). In a study of more than 340 patients suffering from low back or neck pain, a team of Australian researchers found there was no difference in pain severity after six weeks between those who received opioids versus a placebo sugar pill. “It was quite a surprise to us. We thought there would be some pain relief, but overall there was no difference.” Possible downside: The research could convince prescribers not to give opioids when they can actually do good. It’s like this: A study by a group of those shifty Danes found that “Women in their 50s who took estrogen and progestin hormone replacement therapy for menopausal symptoms had an increased risk of dementia within 20 years.” The important bit: As experts point out, that probably means that women who were showing signs of dementia are the ones who sought out HRT. (One big reason is that the effect showed up within a year of beginning HRT — and that’s just “biologically implausible.”) There’s even an editorial with the paper titled, “A causal link remains unlikely.” But that didn’t stop CNN, and presumably other news outlets (including HealthDay News), to phrase it as “HRT use by younger women linked to dementia.” Because that’s more exciting than, “Women with signs of dementia during menopause likely to seek out hormone treatment.” Coming soon: “Aspirin use linked to headaches.” Can vitamin D supplements help prevent heart attacks? One headline for the story on vitamin D reads, “Vitamin D supplements may reduce risk of heart attacks in older adults”. Another dials it back with, “Mixed Results on Vitamin D’s Benefit for Aging Hearts.” But what did the authors of the actual paper have to say? Vitamin D supplementation might reduce the incidence of major cardiovascular events, although the absolute risk difference was small and the confidence interval was consistent with a null finding. (Emphasis ours.) There are often stories about the benefits of coffee, although the terms coffee and caffeine are sometimes (wrongly) used interchangeably; some of coffee’s benefits come from decaf as well. The latest twist comes out of Portugal, where researchers found that even coffee’s wakefulness effect is about more than just the caffeine. First, they found that (no surprise) drinking coffee or taking caffeine directly “made people more prepared to move from resting to working on tasks.” But here’s the cool bit: [D]rinking coffee also increased the connectivity in the higher visual network and the right executive control network – parts of the brain which are involved in working memory, cognitive control, and goal-directed behavior. This didn’t happen when participants only took caffeine. In other words, if you want to feel not just alert but ready to go, caffeine alone won’t do – you need to experience that cup of coffee. The drug maker has said it will “plant and maintain more than 50 million trees by the end of 2025,” and is already more than 20% to the goal with projects in Australia, France, Ghana, Indonesia, the UK, and the US. The maintain part is important. Lots of tree-planting efforts simply plant and abandon, but without maintenance especially during the first few years, the trees just die. To kill cancer cells, you have to find something that differentiates them from normal cells. One of those things is a compound called acrolein that’s unique to cancer. Japanese scientists found that an organic molecule called azide can attach to those cancer cells and, when paired with a fluorescent compound, can light up the cancer. Well well well, they said — if we can attach a fluorescent compound, maybe we can attach a radioactive bomb. That “bomb” is actually a radionuclide called astatine-211 that emits alpha particles as it decays. And the nifty thing about alpha particles is that A) they’re deadly, and 2) they only travel a fraction of a millimeter. In other words… In theory, when astatine-211 is anchored to the inside a cancer cell, the emitted alpha particles should damage the cancer cell, but not much beyond. They tested this on mice, and you betcha it worked — 100% of the mice survived when it was injected into the tumor (80% when injected into the blood). Not only will this work with a lot of different kinds of cancer, thanks to the azide’s targeting ability, “[W]e can use this method to treat very early-stage cancer even if we don’t know where the tumor is.”AZ meets the Lorax, when placebos equal opioids, radiation-bombing cancer, and more
When opioids do nothing
Health journalists not doing their jobs
Bad CNN! No cookie!
Vitamin D non-story
Coffee (not caffeine) gives the get-up-and-go
Shout-out to AstraZeneca
A cancer-seeking radioactive missile
June 29, 2023 ✒ Andrew Kantor
There might be a surprising — and inexpensive — treatment for couples who are “experiencing unexplained infertility”: good ol’ vaginal progesterone, used safely for decades. British researchers who conducted a small study found that women who used the progesterone (400 milligrams twice a day for 14 days) conceived twice as often as the untreated women — 15.3% compared to 7.0%. (The researchers point out the small sample size, though, which means it could have happened by chance.) Oh, and the miscarriage rate with the progesterone treatment was half that of the women who weren’t treated. They don’t know what’s going on — “It could be that treating women with vaginal progesterone is helping the womb to become more receptive to a fertilized egg” — but the results are encouraging. “We need to do further research to prove these results in a larger group of people, but this trial suggests a potential treatment for couples with unexplained fertility. Given its safety and low price, there is no harm in offering this treatment in the meantime.” The hot new way to treat pancreatic cancer is by targeting a gene called KRAS, where mutations drive pancreatic cancer. But there’s a problem. Inhibiting the KRAS gene actually comes back to bite — it turns on a different gene called ERBB, and that just undoes the drug’s hard work: “when KRAS goes down, ERBB goes up and drives KRAS and other related genes back up again.” So the obvious plan: Target both KRAS and ERBB. Which is what UC San Diego researchers did. (There’s already an FDA-approved ERBB inhibitor called Afatinib.) In the lab, that one-two combo worked a treat. “[T]he benefits of using the two drugs together were even larger than the sum of each one’s individual effect. In other words, the drug pairing was greater than the sum of its parts. Thus, the UCSD folks say, “[W]e strongly encourage the clinical testing of this drug combination for patients with pancreatic cancer.” Dutasteride, aka Avodart, is technically for treating an enlarged prostate, but it’s also (wink wink) sold as treatment to stop hair loss. But does it work? And if so, how? The folks at Healthline have all you need to know about dutasteride. (Spoiler: Yes, it does seem to work, but “it may be best to manage your expectations.”) It’s an old question: Why do some statin users get muscle pain and weakness? Now there’s an answer. It’s about an obscure enzyme called HMG-CoA reductase. Two facts about it: As you might imagine, “This connection between a rare disease and a common drug stunned the researchers.” Happy twist: The Israeli team that discovered that it was the cause of limb girdle muscle dystrophy also found a treatment. It’s a drug called mevalonolactone that “allows muscle cells to function more normally even without the HMG-CoA reductase enzyme.” That could mean a treatment for people for whom statins cause severe muscle pain. Sad twist: mevalonolactone may also increase cholesterol, so it would only be for the worst-off patients. This is the kind of interesting connection that might come into play later as we tease out what’s causing what. Johns Hopkins researchers have found a connection between the sense of smell as people age, and the chance of their suffering from depression. Or, put more science-y: “[R]esearchers found that individuals with decreased or significant loss of smell had increased risk of developing significant depressive symptoms at longitudinal follow-up than those in the normal olfaction group.” And the worse the loss of smell, the greater the depression. But which way does the connection go? Is the same factor causing both (e.g., altered serotonin levels, brain volume changes)? Or does one lead to the other — maybe less smell means less appetite means less socializing? “Losing your sense of smell influences many aspects of our health and behavior, such as sensing spoiled food or noxious gas, and eating enjoyment. Now we can see that it may also be an important vulnerability indicator of something in your health gone awry. “Smell is an important way to engage with the world around us, and this study shows it may be a warning sign for late-life depression.” This actually makes logical sense, but it’s good to have a study to prove it: When people have better access to prescription opioids, opioid-overdose deaths go down because “When access to prescription opioids is heavily restricted, people will seek out opioids that are unregulated,” as the lead author of a Rutgers paper explained. Add hypertension to the possible effects of long Covid — in women, at least. A small study (23 women) out of the University of Texas found that… … while only one participant with long Covid had been diagnosed with hypertension prior to contracting Covid-19, “two patients had received a new diagnosis of hypertension post-Covid-19, two had resting [blood pressure] values classified as Stage II hypertension, one as Stage I hypertension and two with high [blood pressure] based on the current guidelines.” The elevation in resting blood pressure was consistent.A better hair loss treatment? Plus fertility made easier, depression and smell, and more
Could a simple fertility treatment be right in front of us?
A pancreatic cancer double-punch
The Long(ish) Read: Keeping the hair?
Why statins cause muscle pain
Less smell, more depression
Short Takes
When opioids are outlawed, people become outlaws
And the latest long-Covid effect…
June 28, 2023 ✒ Andrew Kantor
When it comes to treating migraines, there’s one class of meds that often overlooked: anti-hypertensives. Blood pressure drugs, found Aussie researchers, almost all help with migraine pain, but they’re often overlooked by physicians as a first-line treatment. “[W]hile we can see from the analysis that the effect is true for almost all types of BP medicines, this is not reflected in the current clinical guidelines, which specify just one or two types (such as beta-blockers) but not the full range of therapies that could be useful.” Having trouble makin’ that baby, guys? Did you perchance have even a mild case of Covid-19? That might be your answer. Spanish researchers found that Covid-19 infection caused not only a drop in sperm count months after infection, but also a drop in sperm quality. Worse, this wasn’t just in the sperm that were hanging about while you were infected — the effect continues into the new crop*. “We assumed that semen quality would improve once new sperm were being generated, but this was not the case. We do not know how long it might take for semen quality to be restored and it may be the case that COVID has caused permanent damage, even in men who suffered only a mild infection.” * “Crop of sperm” is either a poor choice of words or a new rock band. Your call. Having a serious Covid infection might lead to chronic pain. It certainly increases the odds, according to researchers at New York’s Upstate Medical University. More than a quarter of the people in a study (25.5%) who had a moderate to severe infection reported chronic pain since their bout. That compared to fewer than 20% of those who were never infected. The bottom line, after the statisticians got involved, is that… “Adjusted probabilities show that chronic pain was roughly 4 percentage points more likely among those with more symptoms during infection than among the never-infected group.” Eli Lilly’s experimental weight-loss pill “helped people lose an average of 15% of their body weight after 36 weeks,” which is as good or better than giving yourself weekly injections of one of the other GLP-1 agonists. Called orforglipron, the pill is still in phase-2 trials, while Novo Nordisk’s semaglutide pill is a bit ahead (phase 3), but requires a 30-minute fast before and after taking it, which could be a complication considering the target audience. Eisai/Biogen’s Alzheimer’s drug Leqembi (aka lecanemab) is likely to get full FDA approval soon, but it comes with caveats that might make it a bit tougher for patients to get. Read the deets. For the first time in 20 years, malaria is spreading locally in the US — and it’s in Florida and Texas. Locally is the key, because cases reported here have always been acquired elsewhere. These, though, “are believed to be locally acquired” and transmitted by mosquitos. Getting people weaned off long-term opioids has to be done carefully, and an international group of clinicians, led out of Australia, has released a set of deprescribing guidelines. They recommend “that clinicians develop personalised deprescribing plans from the beginning for any patient being prescribed opioids” and also published detailed guidelines for creating such a plan. GSK’s vaccine for people at high risk of gonorrhea has received a ‘fast-track’ designation from the FDA. Called Neisseria, it’s currently in a phase 2 trial, but the new designation will mean FDA review could happen more quickly.Covid hurts men where it counts, plus simple migraine meds, malaria makes a comeback, and more
The easy migraine treatment
When your sperm get long Covid
Speaking of Covid…
Another weight-loss pill shines in trial
The Long Read: Getting the new Alzheimer’s meds
Short Takes
Malaria is back
Weaning off opioids the right way
Gonorrhea vax gets fast-tracked
June 27, 2023 ✒ Andrew Kantor
Georgia ranked 45th out of the 50 states and DC for the performance of its healthcare system in the latest annual report from the Commonwealth Fund. The study considered a long list of factors, including “Avoidable deaths from preventable and treatable causes,” access to healthcare, maternal care and mortality, and mental health care. (Of note, this report included the pandemic years, so every state saw its overall score take a hit.) What hurt Georgia a lot: The good stuff: a low rate of alcohol- and drug-related deaths. You can read the overview of the study here, and see the details of Georgia’s performance here (7-page PDF) A new tactic against antibiotic resistance can, it seems, keep bacteria from evolving that resistance in the first place. It’s called dequalinium chloride (DEQ), and right now it’s just “proof-of-concept for evolution-slowing drugs.” Essentially, Baylor College of Medicine researchers found that when stressed (like, say, with impending destruction) certain of the bacteria’s genes can activate to “increase production of protective molecules.” Not only does that program protect the bacteria at the moment, it can also affect its genes for the long term — i.e., making it resistant to the antibiotic. But DEQ, the Baylorites say, can “dial down the master bacterial stress response.” That not only makes the bacteria more susceptible to antibiotics, it prevents its children from inheriting that resistance. Given together with cipro, DEQ reduced the development of mutations that confer antibiotic resistance, both in laboratory cultures and in animal models of infection, and bacteria did not develop resistance to DEQ. Of patients with major depressive disorder, more than a quarter fit into what Stanford researchers say is a new subtype of depression they call the cognitive biotype. Here’s the interesting part: First they tested to see how many fit into this category (which is indicated by “difficulty with the ability to plan ahead, display self-control, sustain focus despite distractions and suppress inappropriate behavior”). That was about 27% of patients. Then they tested to see how three common antidepressants affected them. Result: Patients with this new subtype were less likely to be helped by typical drugs like escitalopram, sertraline, or venlafaxine. [T]he overall remission rates — the absence of overall depression symptoms — were 38.8% for participants with the newly discovered biotype and 47.7% for those without it. This difference was most prominent for sertraline, for which the remission rates were 35.9% and 50% for those with the biotype and those without, respectively. So what could help? They’re thinking guanfacine, aka Intuniv or Tenex, might do the trick; testing is ongoing. “Moms lose significant sleep and free time during kids’ school year, new study finds”. The old thinking: Variants in any of more than 100 genes could lead to early menopause — i.e., before the age of 40. But now British researchers have found that a whopping 98% of women carrying variations of those genes in fact had menopause after 40. In other words, some women might be diagnosed with ‘premature ovarian insufficiency’ when it doesn’t apply at all. As the senior author put it (in, obviously, a lovely British accent), “It now seems likely that premature menopause is caused by a combination of variants in many genes, as well as non-genetic factors.” Using a new type of biosensor, Johns Hopkins researcher found that ruxolitinib — already FDA approved for treating some cancers and skin conditions, can also treat cardiac arrhythmias by inhibiting the CaMKII protein. A 10-minute application of the drug was enough to prevent catecholaminergic polymorphic ventricular tachycardia, a congenital source of pediatric cardiac arrest, and rescue atrial fibrillation, the most common clinical arrhythmia. The finding could lead to new uses for the drug, including (they suggested) “the ‘pill in a pocket’ scenario” where patients could take a ruxolitinib-based medication occasionally as symptoms arise. For a long time, BMI (body mass index — the ratio of weight to height) was the go-to measurement for obesity. But as you might imagine for such a crude comparison, it’s on its way out as a reliable tool. [P]eople with the same BMI may have substantially different body fat percentage based on a variety of factors such as age, muscle mass, sex and race. In an example from one large study, adults with a BMI of 25 had a body fat percentage ranging from 14% to 35% for men, and 26% to 42% for women. GSK, the company formerly known as Glaxo Smith Kline, decided it needed to stop investors from freaking out over impending lawsuits over Zantac. You remember Zantac, right? The heartburn drug that ended up causing cancer? Anyway, the company settled a lawsuit with a guy from California before it could go to trial, and that “could set a precedent for thousands of cases set to go to trial next year” and which gave investors jitters. Merck is now facing a slew of lawsuits over Singulair, its asthma and allergy medicine. The FDA required a black-box warning because of psychiatric side effects. Now, the plaintiffs say, they have evidence that Merck knew about those dangerous side effects long before that warning was required — it just didn’t disclose them.A drug to stop evolution, a new type of depression, why BMI is useless, and more
Report: Georgia’s health needs improvement
Take that, Darwin
A new depression subtype (and why antidepressants don’t always work)
Captain Obvious uses earplugs (and locks the door)
Premature menopause is more complicated than we thought
Old drug, new heart treatment
The Long Read: Why BMI is yesterday’s metric
Short Takes: On the legal fronts
GSK settles Zantac suit
What did Merck know and when did it know it?
June 24, 2023 ✒ Andrew Kantor
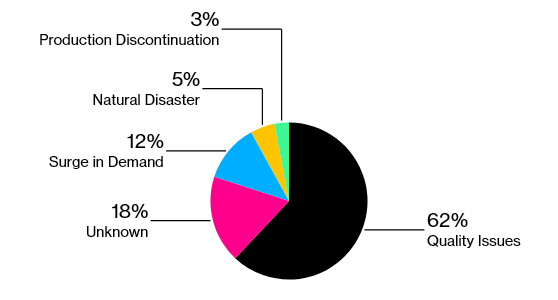
The US military is going all trust but verify on the FDA. The Department of Defense is apparently concerned enough about the quality of generic drugs — many of which come from facilities (foreign and domestic) that have had … issues — that it’s talking to independent lab Valisure to test generic drugs for contamination. The move raises questions about the Food and Drug Administration’s ability to adequately police generic medicines. With mounting drug shortages, most of which are caused by quality problems, military officials have gone so far as to call vulnerabilities in the drug supply chain a national security threat. Fun fact: Kaiser Permanente already does this. “Kaiser, which serves 12.7 million Americans, started working with Valisure on additional drug quality checks more than two years ago.” And with the possibility of regulations being loosened in order to ease drug shortages, you can bet that quality is going to get a bunch more scrutiny. If for some reason you’re selling Elf Bar or Esco Bar disposable e-cigs, stop. They’re illegal, and the FDA is cracking down — it “issued warnings to 189 convenience stores, vape shops and other retailers” so far, and customs officials are seizing the stuff at ports. Fun fact: When vapes are outlawed, only outlaws will sell vapes. Under the law, companies were supposed to remove their vapes from the market and file FDA applications, but new products continue to launch. There aren’t any treatments for tinnitus, but that doesn’t mean people haven’t come up with some interesting ones. Do any stand out? Yes, as a matter of fact, said Brazilian scientists. Shooting lasers at it. Of course, no one calls it “shooting lasers in your ears” — it’s low-level laser therapy and associated photobiomodulation. And, per the study, it’s the best of a so-so lot of options. The contenders: The treatments tested were laser acupuncture, flunarizine dihydrochloride, Ginkgo biloba (a medicinal plant), and low-level laser stimulation of the internal auditory canal or meatus (transmeatal stimulation), on its own and combined with vacuum therapy, ultrasound, G. biloba or flunarizine dihydrochloride. “The best outcomes,” they found, “were observed in patients treated with laser acupuncture alone and transmeatal low-power laser stimulation alone.” Now you know. This is a story that runs every year, so we’ll keep it short. Remember that a bunch of medications you dispense might make your patients more susceptible to sunburn. The folks at Healthline have the list of common and less-common meds that might suggest a bottle of SPF 30 with every purchase. As much fun as I like to poke at the Atlantic, it does do good journalism … although it dies like to channel its inner Eeyore. If you’re interested in a balanced look at the Covid-origins debate, the magazine’s got you covered with the evidence, the questions, and the contradictions for both a lab-leak theory and a public-market theory, taking into account the latest revelations. [T]he origins question has broken down into a pair of rival theories that don’t—and can’t—ever fully interact. They’re based on different sorts of evidence, with different standards for evaluation and debate. Each story may be accruing new details—fresh intelligence about the goings-on at WIV, for example, or fresh genomic data from the market—but these are only filling out a picture that will never be complete. In between flu vaccines and flu treatment are flu preventatives — drugs given to people at high risk from the flu but who can’t be vaccinated. And the FDA has just fast-tracked one (CD388) from Cidara and Janssen. Scientifically speaking it’s technically a drug-Fc conjugate and officially for “the prevention of influenza A and B infection in adults who are at high risk of severe influenza, including those for whom vaccines are either ineffective or contraindicated.” President Biden signed an executive order designed to increase women’s access to contraception. The goal is to keep the issue of abortion from even arising in the first place by reducing unwanted and unplanned pregnancies. Plans going forward “could include convening pharmacies, employers, and insurers to discuss the issue.”Lasers vs tinnitus, DoD distrusts FDA, annual sunburn story, and more
DoD isn’t happy about med safety
FDA: Illegal vapes are illegal
Lasers beat pharma for tinnitus
Sunburn and meds
The latest Covid-origins overview
Short Takes
A new flu-blocking med
Just gonna put this out there
June 23, 2023 ✒ Andrew Kantor
False teeth might give people pneumonia. More specifically, dentures are apparently really, really good at harboring pneumonia-causing bacteria. If you have pneumonia and you’re wearing dentures, you’ll have more bacteria on those dentures. Seems obvious. But, assuming you clean those dentures regularly, you shouldn’t that much more than people without pneumonia. Yeah, well, British researchers found that maybe people need to do a better job cleaning and disinfecting*. “We were expecting to see a difference but were surprised to see 20 times the number of potentially pneumonia-causing bacteria on dentures in people with pneumonia, compared to people without.” Bottom line: Those false teeth are like low-rent housing for the kind of stuff you don’t want to be breathing or swallowing. * It would be impolite to make any joke about British dental care. Got patients seeing a chiropractor for pain? You’ve probably thought to yourself, “I bet it would help to give them a combo of hemp oil, calamari oil, and broccoli!” Well you’d be right. A study out of North Carolina State University found that just such a combination “can help manage pain intensity, interference, and oxidative stress when combined with standard chiropractic care.” Patients reported pain intensity decreasing by over half (52%) and a decrease in areas of pain interference like mood and quality of sleep. The authors also report decreases in oxidative stress markers. You know how they say when you reach your 20s your brain is pretty much set in its ways — you are who you are. Unless, that is, you take some psychedelic drugs. It seems that one feature all psychedelic drugs* have in common is that they… …reopen “critical periods” in the brain, when mammals are more sensitive to signals from their surroundings that can influence periods of brain development. They can help open the brain to being rewired — either learning something new (perhaps helping with stroke recovery) or being able to forget something that’s feels hardwired (PTSD trigger or and depression). It’s not a permanent treatment, though; the effect only lasts as long as the drug does, which is one reason use needs to be combined with at-the-moment therapy to take advantage of the brain’s temporary flexibility. Read more from the folks at Johns Hopkins, where they’re figuring all this out. * At least ibogaine, ketamine, LSD, MDMA and psylocibin For people with PTSD or concussions, persistent headaches can be a big problem. New research out of the VA has found that there might be a simple pharmacological solution: prazosin, the blood-pressure drug. Migraine drugs don’t work because, well, these aren’t migraines. And prazosin has been used for treating other aspects of PTSD, but no one thought to see about using prazosin for those headaches. Good thing they did. Before the trial began, study participants had an average of 18 headache days each month. By the end of the 12-week period, those taking prazosin only had headaches for an average of six days a month. […] Significantly more participants in the prazosin group had at least 50% fewer headaches during the 12 weeks of taking a full dose of medication. The European Medicines Agency has sort-of raised a yellow flag — a ‘thyroid cancer safety signal’ — for several Novo Nordisk drugs, including semaglutide. [T]he discussion followed the publication of a study suggesting that there might be an increased risk of thyroid cancers with the use of these drugs in patients with Type 2 diabetes. The safety signal just means the EMA wants Novo to keep a close eye on “potential adverse events from the use of approved drugs.” There’s no danger, everyone says, just the possibility. (We’re including this story so we can refer back to it in a few years if necessary.) The FDA has approved Eli Lilly and Boehringer Ingelheim’s drugs Jardiance and Synjardy to treat type 2 diabetes in children aged 10 to 17. And the FDA has approved a drug combo to treat HRR gene–mutated metastatic castration-resistant prostate cancer: Pfizer’s Talzenna (aka talazoparib) and Xtandi (that’s enzalutamide). This follows our story yesterday about the approval of abiraterone, olaparib, and prednisone to treat a different kind of metastatic castration-resistant prostate cancer. With a shrug, the FDA has sorta kinda recommended RSV vaccines for people 60 and older. Well, for people 60-65 yeah, why not; but they were iffy about the over-65 crowd. Instead of telling seniors that they should be vaccinated, the panel has said that people may get a dose of GSK’s Arexvy or Pfizer’s Abrysvo if it is right for them.Who needs calamari oil, danger from dentures, treating brain headaches, and more
They really need to clean their dentures
A yummy treat for chiro patients
How psychedelic drugs work
Treating PTSD headaches
There is (probably) no thyroid-cancer risk for semaglutide
Short takes
FDA approval #1: for kids’ diabetes
FDA approval #2: for prostate cancer
Yeah, whatevs, if they want it
June 22, 2023 ✒ Andrew Kantor
If you know Joe Ed, you know the guy’s got a heart of gold — and that he’s been working hard for the pharmacy profession for a long time. He’s not only been on GPhA’s board of directors, he’s also served as a Georgia Pharmacy Foundation board member and chair of the foundation’s mental health initiative, Pharmwell. If you know Joe Ed, you also know his story — and if you don’t you should check out “My story: Recovery is possible” in the February/March issue of Georgia Pharmacy magazine. Congratulations and a huge high-five from everyone at GPhA! Izabela Welch (At Large) Thomas Sherrer (At Large) Bryce Allfrey (At Large) Maria Thurston (representing ACHP) You can see all of GPhA’s leadership — new and returning — at GPhA.org/about. Carl Heindel (region 1) Amanda Cherry (region 6) Kandon Render (region 7) Jennifer Herrell (region 9) Warren Koehler (region 11) You can see the region boundaries and the region presidents at GPhA.org/regions. The world’s first saliva-based pregnancy test is (probably) coming to the US of A. (It’s already available in the UK and Ireland, and the company has applied for FDA authorization.) The plus: You don’t have to pee on a stick. The minuses: It’s slightly less accurate than urine-based tests, and it takes 30 excruciating minutes to get a result. In clinical trials of more than 300 women, the test proved to be around 95% accurate when taken from the first day of a missed period. It’ll probably retail for $12 or $13. Good news for some of us: Apparently a midday nap means a bigger brain. Sorry, a “larger total brain volume — a marker of good brain health linked to a lower risk of dementia and other diseases.” (At least for those aged 40 to 69.) So found British researchers who compared brain size and cognitive ability between those who nap and those who don’t. Eyebrow raiser: They determined these ‘habitual nappers’ not by interviewing co-workers, but based on 97 genetic markers that were already known to indicate — I kid you not — “people predetermined to nap.” Then they compared their brain volume to regular folks. The research team estimated that the average difference in brain volume between people programmed to be habitual nappers and those who were not was equivalent to 2.6 to 6.5 years of ageing. Another tidbit to take home: “Naps of 30 minutes or less provide the best short-term cognitive benefits.” Fun fact: Someone about to have an epileptic seizure emits an odor that can be detected by trained dogs. The problem, obviously, is that you need to have a dog with you at all times, which can be cumbersome. Enter engineers at Sandia National Laboratories, who have developed “a miniaturized sensor system that can detect the specific gases released from the skin of people with epilepsy before a seizure.” “We were able to identify a bouquet of eight VOCs that were unique to seizures. Of those, three VOCs were considered principal, appearing in every sample taken from someone having a seizure. These VOCs start building in concentration prior to seizure onset.” The device is already tiny, but it currently requires a bit of gauze attached to the skin to work. That’s not a big deal, they say, and they hope to have a sellable device like a wristwatch on the market by the end of 2024. Yep, next year. q Medications through the nose — the idea holds a lot of promise, but it’s not as simple as reformulating a drug. Medscape has the details of the challenges and potential of nasal delivery. The nasal route is quick, needle-free, and user-friendly, and it often requires a smaller dose than other methods, since the drug doesn’t have to pass through the digestive tract, losing potency during digestion. The paper: “Fetally-encoded GDF15 and maternal GDF15 sensitivity are major determinants of nausea and vomiting in human pregnancy”. What it means: An international group of researchers, led by Cambridge University and USC, has confirmed the cause of morning sickness. It’s a hormone called GDF15, most of which comes from the fetus and placenta. Twist: Some women produce more GDF15 even when not pregnant, and they’re less likely to experience morning sickness. “[T]he severity of nausea and vomiting of pregnancy is the result of the interaction of fetal-derived GDF15 and the mother’s sensitivity to this peptide, which is substantially determined by her prior exposure to the hormone.” The downside: There’s no treatment for this, but at least it a researchable target. “As Adderall shortages persist, Takeda’s rival Vyvanse is now in short supply”. The FDA has approved a combination of olaparib (aka Lynparza), abiraterone, and prednisone to treat one of the most serious forms of prostate cancer — the BRCA-mutated metastatic castration-resistant type. It took a while for the approval to come through: A study from Merck published in 2022 found that the drug combo reduced risk of death or disease progression of 34% and an average progression free survival period of more than two years. Spit-based pregnancy test, how to get a bigger brain, and a big welcome to GPhA’s new leadership (and more!)
Welcome to the presidency, Joe Ed!
 A big Buzz congrats to GPhA’s newly sworn-in 2023–24 president, Joe Ed Holt of Valdosta.
A big Buzz congrats to GPhA’s newly sworn-in 2023–24 president, Joe Ed Holt of Valdosta.… and welcome to GPhA’s leadership members!
Newly elected to the Board of Directors
Newly elected region presidents
Coming soon: a new kinda of pregnancy test
I’m not lazy, I’m enlarging my brain
Nasal news
A seizure-scent warning device
The Long Read: Up the Schnoz edition
The cause of morning sickness
Short Take
First they came for the Adderall and I said nothing, for I did not take Adderall
Prostate-cancer combo